Trichomycosis axillaris, also called trichobacteriosis or trichomycosis palmellina, is a common skin infection caused by bacteria of the genus Corynebacterium spp., particularly Corynebacterium flavescens. It typically affects hair of the axillas, although it can also occur in pubic and perianal hair and, very rarely, scalp hair.
The prevalence is highest in tropical countries, with a warm and humid climate. Excessive sweating, inadequate hygiene, and not shaving the area favor its appearance. The condition is observed most often in young adults, and is more common in men than in women.1,2
A diagnosis of trichomycosis axillaris is suspected on the basis of clinical findings, and can sometimes be supported by additional techniques such as Wood light, direct microscopy, and dermoscopy. Confirmation of the diagnosis is based on culture, although false negatives are not unknown. The diagnosis is sometimes made retrospectively, after observing a rapid response to the use of hygienic measures and topical antibiotics.2,3
We present a typical case of trichomycosis axillaris and we review the dermoscopic findings.
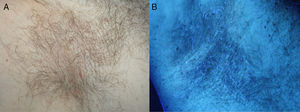
The patient was an 84-year-old man with a past history of atrial fibrillation and systemic hypertension on treatment with acenocumarol and enalapril, and surgical excision of a basal cell carcinoma and superficial spreading melanoma. He consulted for axillary bromhidrosis that had started 2 months earlier. Examination revealed soft, yellowish-white, irregular masses with a bad odor, adherent to the central segment of the hairs in the axilla (Fig. 1A). Weak, yellow-white fluorescence was observed with Wood light (Fig. 1B). On dermoscopy, irregular yellowish-white masses were observed around the hairs, some forming white concretions with a brush-like or feathery appearance (Fig. 2). Direct examination with potassium hydroxide (KOH) revealed numerous mucoid sheaths around the hairs (Fig. 3). On Gram stain, hair shafts were observed to be massively colonized by gram-positive coccobacillary structures.
A diagnosis of trichomycosis axillaris was made and 2 weeks of treatment with topical clindamycin was prescribed, leading to complete resolution of the condition.
Three clinical forms of trichomycosis are recognized: flava, rubra, and nigra. Trichomycosis flava is the most common and is characterized by the presence of odorous mucoid sheaths adherent to the hair shafts, forming thick, irregular yellowish-white nodules that can cover the hairs completely. The root of the hair and the adjacent skin are not usually affected. The chemical composition of this substance has still not been elucidated, although it is believed to derive from bacterial metabolism in the apocrine glands.1–3
The unpleasant odor is the main reason for seeking care, but, given its asymptomatic nature, the condition can often be a casual finding during physical examination.4
Diagnosis is reached through a full medical history, physical examination that includes the use of Wood light, dermoscopy, direct examination with KOH, and Gram stain.
Dermoscopy is a simple technique for all dermatologists. Initially it was used to study melanocytic lesions, but more recently its has also been used to facilitate the diagnosis of nonmelanocytic lesions and of inflammatory and infectious diseases. The dermoscopic characteristics of dermatoses that affect the hair, such as pediculosis, pseudofolliculitis, and alopecia areata have already been described.5,6
In trichomycosis, dermoscopy reveals yellowish-white masses with a waxy appearance, adherent to the hair. The dermoscopic findings in our patient were similar to previous reports, and some authors have used the term feather sign or brush sign.7,8 Concretions with the appearance of a rosary of crystalline stones have also been described.9
The differential diagnosis includes trichorrhexis nodosa, monilethrix, pseudomonilethrix, trichorrhexis invaginata, pediculosis, peripilar sheaths, and piedra.10
Treatment consists of general measures such as adequate hygiene and shaving of the affected areas, together with control of the hyperhidrosis and the use of topical treatments (benzoyl peroxide or antibiotics such as erythromycin or clindamycin).1,3
In conclusion, trichomycosis axillaris is probably underdiagnosed. Dermoscopy is a useful, quick, and inexpensive technique that will support the clinical diagnosis by identifying characteristic signs of the condition.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Rojas Mora E, Freites Martínez A, Hernández-Núñez A, Borbujo Martínez J. Trichomycosis axillaris: Clinical, Wood lamp, and dermoscopic diagnostic images. Actas Dermosifiliogr. 2017;108:264–266.