Hand eczema affects up to 15% of the adult population is a common cause of dermatologic consultation. It has a marked psychological and occupational impact, with mayor socioeconomic implications.1,2 Chronic hand eczema (CHE) is considered to exist when the lesions persist for more than 3 months or the patient presents more than 2 episodes in a year. Five clinical subtypes of CHE have been identified: hyperkeratotic, fissured, dyshidrotic, nummular, and pulpitis,2 although overlap is common. CHE may arise on a background of atopic dermatitis, be caused by contact dermatitis (allergic or irritant), or be idiopathic.
Key factors in the management of CHE include the use of emollients and the investigation and avoidance of possible triggers. Numerous treatment options are available: topical corticosteroids and calcineurin inhibitors, phototherapy, oral retinoids, and immunosuppressants.1–3 However, treatments must always be individualized.
Paraffin wax is a solid hydrocarbon derived from petroleum or coal. It is used in the food and textile industries, as well as in the manufacture of paper and of candles. The dermocosmetic industry also employs paraffin wax as a base for some emollients. The possibility to perform paraffin wax baths comes from the low melting point of this wax (approximately 37.5°C).4,5 Paraffin wax baths provide superficial heat, improving local blood flow and relieving pain6; they have traditionally been used in arthritis of the hands.7 Recently they have also been shown to improve post-traumatic rigidity of the hands8 and ankles5 and to be useful in the treatment of carpal tunnel syndrome.6 Paraffin wax baths have also been widely used in the dermocosmetic field in order to improve skin quality through their reparative effects on the skin barrier, acting as a very potent emollient. However, their use in CHE has not been reported in the literature.
We therefore undertook a study to determine the efficacy of paraffin wax baths in the treatment of CHE. Thirteen patients (5 men and 8 women) with hyperkeratotic or fissured CHE, pulpitis, or a combination of these conditions were selected. The mean age of the patients was 63 years. Treatment was performed exclusively with paraffin wax baths, 5 days a week for 4 consecutive weeks.
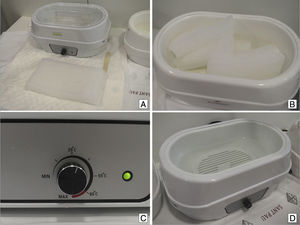
The device used for the treatment was a RehabMedic temperature-controlled bath measuring 36×26×18cm, with an eliptical design and rounded borders (minimum required voltage, 220V; mean power consumption, 150W).
The treatment protocol was as follows:
- 1.
Prepare the appropriate device and blocks of paraffin wax (Fig. 1A).
- 2.
Cut the paraffin wax blocks into appropriately sized cubes to be introduced into the tank (Fig. 1B).
- 3.
Set the thermostat to 35-40°C (Fig. 1C).
- 4.
Wait 90-120minutes for the paraffin to melt, and confirm that the temperature is optimal for the patient's hands to be introduced (Fig. 1D).
- 5.
Submerge 1 hand completely for 3 to 4seconds and withdraw. Repeat this procedure 5 to 8 times until a film of paraffin wax covers the hand, forming a white glove (Fig. 2A). Repeat the procedure with the other hand. If the device is of sufficient size, both hands can be treated simultaneously (Fig. 2B).
- 6.
Maintain both hands in sealed plastic bags for 15 to 20minutes (Fig. 2C).
- 7.
Remove the paraffin wax glove (Fig. 2D).
Evaluation was performed at the end of the complete treatment cycle using the DermaSat questionnaire, validated by the Spanish Contact Dermatitis and Skin Allergy Research Group (GEIDAC)9; this questionnaire evaluates patient satisfaction after the treatment.
The results are shown in Table 1. Efficacy was considered very good or good in 46% and 54%, respectively. Similar results were observed for comfort and medical follow-up. Impact on the quality of life was considered very positive in 30%, positive in 53%, and fair in 15%. No significant side effects were detected, but 51% of patients considered time consumption to be significant. The overall opinion of the patients was very good in 54% and good in 46%.
Series of Patients Treated With Paraffin Baths.
| Sex | Age | Eczema Subtype | Etiology | Time Since Onset, y | Previous Treatments | Efficacy | Comfort | Impact | Monitoring | Adverse Effects | Overall Opinion | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | F | 52 | Hyperkeratotic/fissured | AD | >5 | Emollients, topical CS, CI, CsA | Excellent | Good | Excellent | Excellent | Fair | Excellent |
| 2 | M | 74 | Pulpitis | Idiopathic | >5 | Emollients, topical CS, CI, PUVA | Excellent | Excellent | Good | Excellent | Fair | Good |
| 3 | M | 72 | Hyperkeratotic/fissured | Idiopathic | <1 | Emollients, topical CS | Good | Excellent | Excellent | Excellent | Excellent | Excellent |
| 4 | F | 36 | Hyperkeratotic/fissured | ICD | <1 | Emollients, topical CS | Excellent | Excellent | Excellent | Excellent | Excellent | Excellent |
| 5 | M | 70 | Pulpitis | Idiopathic | >5 | Emollients, topical CS, PUVA | Good | Good | Good | Excellent | Fair | Good |
| 6 | M | 58 | Hyperkeratotic | Idiopathic | <1 | Emollients, topical CS, PUVA, retinoids | Good | Good | Good | Fair | Good | Good |
| 7 | F | 62 | Hyperkeratotic/fissured | ICD | >5 | Emollients, topical CS, PUVA, MTX | Excellent | Excellent | Excellent | Excellent | Excellent | Excellent |
| 8 | M | 85 | Hyperkeratotic/fissured | Idiopathic | >5 | Emollients, topical CS, PUVA, MTX, retinoids | Good | Poor | Good | Good | Good | Excellent |
| 9 | F | 82 | Pulpitis | Idiopathic | >5 | Emollients, topical CS | Excellent | Excellent | Good | Excellent | Fair | Good |
| 10 | F | 72 | Hyperkeratotic | Idiopathic | >5 | Emollients, topical CS, CI | Good | Excellent | Fair | Good | Good | Excellent |
| 11 | F | 63 | Hyperkeratotic/fissured | Idiopathic | 1 – 5 | Emollients, topical CS, CI | Good | Excellent | Fair | Good | Fair | Good |
| 12 | F | 52 | Hyperkeratotic/fissured | Idiopathic | 1 – 5 | Emollients, topical CS, PUVA, retinoids | Good | Fair | Good | Excellent | Excellent | Good |
| 13 | F | 45 | Hyperkeratotic | Idiopathic | >5 | Emollients, topical CS, CI, PUVA, retinoids | Excellent | Good | Good | Excellent | Excellent | Excellent |
Abbreviations: AD, atopic dermatitis; CI, Calcineurin Inhibitors; CS, corticosteroids; CsA, Ciclosporin A; F, female; ICD, irritant contact dermatitis; M, male; MTX, methotrexate; PUVA, psoralen–UV-A.
We believe that these results are very promising, taking into account the good risk-benefit relationship. Furthermore, the impact of the time required to perform the procedure could be reduced by home treatment after training at our center, adapting the protocol to the needs of each patient and each moment in time. We realize that this is a preliminary study with significant limitations, but we consider it to be an very positive initial approximation on which to base more complex studies that could elevate the level of evidence of the treatment and thus, in the future, introduce this procedure into CHE treatment algorithms.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Mir-Bonafé JF, Serra-Baldrich E, Rozas-Muñoz E, Puig L. Baños de parafina para el tratamiento del eccema crónico de las manos. Actas Dermosifiliogr. 2017;108:261–264.