Scabies is a skin condition caused by the human mite Sarcoptes scabiei var. hominis. Transmission is direct, through skin contact, between members of a family or people in intimate relationships and, more rarely, via fomites. Conditions such as overcrowding in the usual place of residence, poorly ventilated spaces, and prolonged direct contact with people infected by the mite are risk factors for contracting the infection. The main clinical characteristic is pruritus as an antigenic response to the saliva, eggs, and feces of the mite.1
An increase in cases of scabies has recently been reported in Turkey in the context of the policy undertaken in that country to confine people to their homes owing to the COVID-19 pandemic.2 During the lockdown in Spain owing to the COVID-19 pandemic, the dermatology department at Hospital Universitario Miguel Servet in Zaragoza observed an increase in reporting of cases of familial scabies.
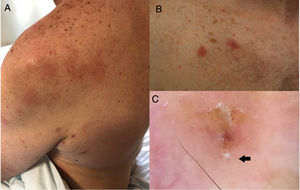
Table 1 shows a series of cases of familial scabies, reported during the confinement due to COVID-19, between March and May of 2020. A total of 4 families of between 2 and 5 members were affected. The youngest affected members were twin girls aged 3 years. Previous treatments were between 2 and 6 cycles of topical permethrin. Several of these patients presented resistance to the first-line treatment used, 5% topical permethrin, and administration of oral ivermectin was required to eradicate the disease. One patient presented a coexisting maculopapular rash due to COVID-19 with a positive PCR test, which revealed the presence of scabietic nodules when it disappeared (Fig. 1). During lockdown, oral ivermectin was prescribed at our hospital to 19 patients, twice the rate for the same period of time in the previous months (9 patients).
Familial Cases of Refractory Scabies Recorded in our Department.
| Family | Number of members | Sex and age | Initial therapy and number of cycles performed | Resolution with permethrin | Second-line treatment and number of doses administered | Resolution with oral ivermectin |
|---|---|---|---|---|---|---|
| 1 | 5 | Father, 47 y | Topical permethrin, 5%×4 | No | Oral ivermectin, 200μg/kg×2 | Yes |
| 1 | Mother, 47 y | Topical permethrin, 5%×3 | No | Oral ivermectin, 200μg/kg×2 | Yes | |
| 1 | Son, 7 y | Topical permethrin, 5%×2 | No | Oral ivermectin, 200μg/kg×2 | Yes | |
| 1 | Daughter, 3 y | Topical permethrin, 5%×2 | No | Oral ivermectin, 200μg/kg×2 | Yes | |
| 1 | Daughter, 3 y | Topical permethrin, 5%×2 | No | Oral ivermectin, 200μg/kg×2 | Yes | |
| 2 | 3 | Father, 59 y | Topical permethrin, 5%×4 | No | Oral ivermectin, 200μg/kg×2 | Yes |
| 2 | Mother, 46 y | Topical permethrin, 5%×3 | Yes | No | – | |
| 2 | Daughter, 14 y | Topical permethrin, 5%×6 | Yes | No | – | |
| 3 | 2 | Mother, 56 y | Topical permethrin, 5%×6 | Yes | No | – |
| 3 | Daughter, 17 y | Topical permethrin, 5%×6 | Yes | No | – | |
| 4 | 5 | Father, 60 y | Topical permethrin, 5%×6 | No | Oral ivermectin, 200μg/kg×2 | Yes |
| 4 | Mother, 45 y | Topical permethrin, 5%×6 | No | Oral ivermectin, 200μg/kg×2 | Yes | |
| 4 | Daughter, 25 y | Topical permethrin, 5%×6 | No | Oral ivermectin, 200μg/kg×2 | Yes | |
| 4 | Daughter, 17 y | Topical permethrin, 5%×6 | No | Oral ivermectin, 200μg/kg×2 | Yes | |
| 4 | Son, 14 y | Topical permethrin, 5%×6 | No | Oral ivermectin, 200μg/kg×2 | Yes |
The incubation period of scabies is known to be 4 weeks, on average.3 This may explain why an increase in the number of cases was observed a month after the beginning of lockdown, favored by the permanent close contact between people living in the same household. The lockdown was necessary to slow the COVID-19 pandemic. An increasing number of reports has been observed of diseases that have been made more severe or have led to death owing to the lockdown.4 The increased intimate and constant contact imposed by the lockdown has caused scabies to spread within families and has made it more difficult to treat. In our experience, oral ivermectin provides a safety and efficacy profile that may make it the treatment of choice in these cases.5 Nevertheless, cleanliness in the home and treatment of fomites is essential to ending the infestation.
The authors would like to thank Estrella Simal Gil, Ana Morales Callaghan, Isabel Abadías, Oihana Pascual Martínez, and Yolanda Gilaberte for their valuable contributions to this article.