A 12-year-old girl with no medical history was referred to the pediatric plastic surgery department for a lesion that had appeared 3 months earlier on the back of her right hand and consisted of an indurated, slightly raised brownish plaque that was painful to the touch (Fig. 1).
The first diagnostic test performed was a Doppler ultrasound, which revealed a subcutaneous lesion compatible with an arteriovenous malformation. Subsequent magnetic resonance imaging (MRI) supported this suspicion. After presenting the case to the Vascular Anomalies Committee at our center, we opted for treatment with embolization and subsequent surgery. Embolization was not possible due to imaging findings compatible with thrombosis of the malformative nidus. As the patient was asymptomatic at the time, a wait-and-see approach with ultrasound monitoring was adopted.
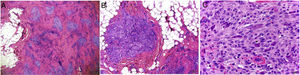
One year later, the patient requested treatment for pain related to trauma and the visible lesion was surgically resected. Histopathology of the lesion indicated a plexiform fibrohistiocytic tumor without tumor-free margins. The neoformation affected the subcutaneous cellular tissue and superficial areas of the skeletal muscle, sparing the overlying skin. It presented a plexiform distribution, with tumor nests composed of spindle cells or monomorphic epithelioid cells accompanied by giant multinucleated cells. A fibrous stroma with dilated vessels was evident between the nests. The proliferative index was less than 3% and no atypical mitoses, necrosis, or xanthomatous cells were observed (Fig. 2). Immunohistochemistry was negative for CD31, CD34, Wilms tumor protein 1 (WT1), and glucose transporter-1 (GLUT1).
A thoracic computed tomography scan, performed as part of the tumor extension study, revealed a nodule of 3mm in the right lower pulmonary lobe. The pediatric thoracic surgery team proceeded with thoracoscopic resection of the nodule, which was compatible with a carcinoid tumorlet.
The results of imaging studies of the right hand revealed a residual lesion with invasion of muscle and tendon and erosion of the cortical bone of the fourth metacarpal. After discussing the case with a multidisciplinary team consisting of oncologists, plastic surgeons, traumatologists, radiologists and pathologists, 2 therapeutic options were established: close clinical observation or complete resection of the lesion. Ultimately, the family opted for surgery, and the fourth and fifth fingers of the right hand were amputated. Currently, the patient is asymptomatic and is undergoing follow-up and rehabilitation.
Plexiform fibrohistiocytic tumor, first reported by Enzinger and Zhang in 1988,1 is a rare soft-tissue tumor with intermediate potential for malignancy.2 It shows a predilection for children and young adults, affecting those under 20 years of age in 60%–70% of cases.3,4 It is more prevalent in females and does not predominate in any ethnic group.5 Its etiology is unknown, but congenital cases and those related to previous trauma have been reported.3–6
Clinically it presents as a painless, slow-growing, indurated mass or plaque (1–3cm) that affects the dermis and hypodermis. It can sometimes cause pain, ulceration, or changes in the color of the overlying skin, and in rare cases, including the present case, spreads to the skeletal muscle. It usually affects the upper limbs, mainly the fingers, hand, or wrist. Cases of lower limb, trunk, head, and neck involvement have been reported.3–6
Initial clinical and radiological diagnosis is challenging. MRI shows an infiltrative lesion or plaque at the level of the subcutaneous tissue, with no specific signal characteristics that allow differentiation from other benign (including some types of vascular anomalies) or malignant entities.7 The definitive diagnosis is based on pathological findings. Histology shows nodules or fascicles of histiocytes, fibroblasts, and osteoclast-like cells, arranged in a characteristic plexiform pattern. Immunohistochemistry reveals CD68+ histiocytic cells and fibroblasts positive for smooth muscle actin and vimentin.3–6,8
Surgical resection with negative margins is the treatment of choice. Local recurrence has been documented in 12.5%–40% of cases, and is often detected 1–2 years after surgery.3 After complete resection the clinical course of this tumor is typically benign, although regional lymph node (6%) and lung (2%–19%) metastases have been reported, necessitating long-term follow-up of affected patients.3–5
In summary, we describe a case of plexiform fibrohistiocytic tumor in a 12-year-old girl. The decision to resect the tumor, despite a relatively low risk of nodal and pulmonary metastases, posed a conflict for the treating physicians as it involved amputation of 2 fingers on the affected hand. Ultimately the family, perhaps influenced by the incidental diagnosis of a pulmonary nodule in the tumor extension study, opted for surgery to avoid the potential risk of future metastasis.
We wish to emphasize the importance of pathological anatomy in the diagnosis of soft-tissue tumors, which comprise multiple entities, the management and prognosis of which can vary considerably.
Conflict of InterestThe authors declare that they have no conflict of interest.
The authors thank Dr. Rodriguez and Dr. Espinola, pathologists at Hospital 12 de Octubre, Madrid, for providing the histological images associated with this clinical case. Thanks also to the staff in the departments of Pediatric Traumatology (Dr. Martí); Pediatric Thoracic Surgery (Dr. Morante, Dr. Lopez, and Dr. Antón-Pacheco); Pediatric Hemato-Oncology (Dr. Perez and Dr. Baro); and Pediatric Radiodiagnosis (Dr. Gallego) of the Hospital 12 de Octubre, Madrid, for their contributions to decision-making and patient management.