A 56-year-old man, originally from a rural area in Paraguay and working as a gardener, presented with a large ulcerated facial lesion. His relevant past medical history included smoking and moderate alcohol consumption. Nearly 2 years prior to this presentation, he had developed a non-painful and non-pruritic papular lesion on his left cheek, which had eventually progressed to cover a large part of his face. Additionally, he had a several-year history of chronic cough and a 6-month history of significant weight loss.
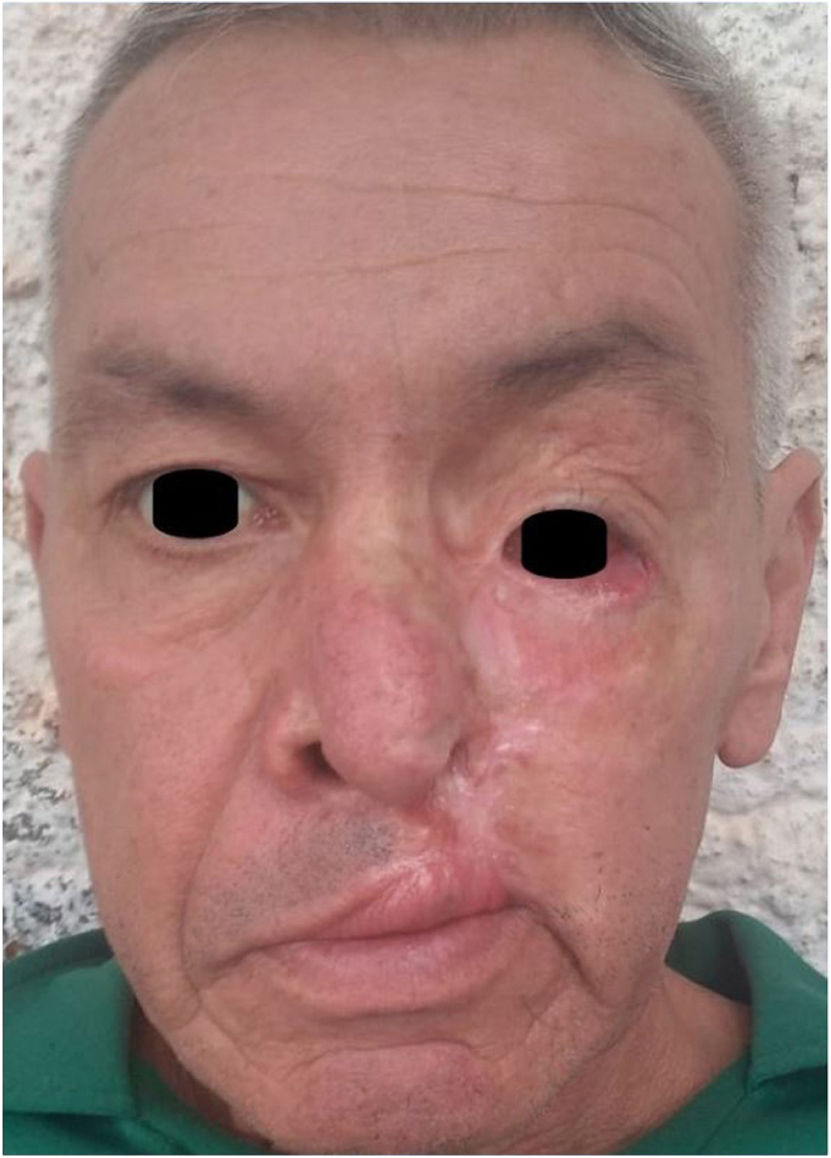
Physical examinationThe physical examination revealed the presence of a fibrinous-based ulcerative plaque with well-defined borders, irregular elevated edges, crusted areas, and 10cm x 8cm hypertrophic regions. The lesion predominantly touched the left side of the face and involved the nasal bridge, eyelids, cheek, upper lip, both wings, nasal fossae, and both mucosas (figure 1). Palpable lymphadenopathies were f in the left cervical and supraclavicular chains, with no other skin lesions being observed.
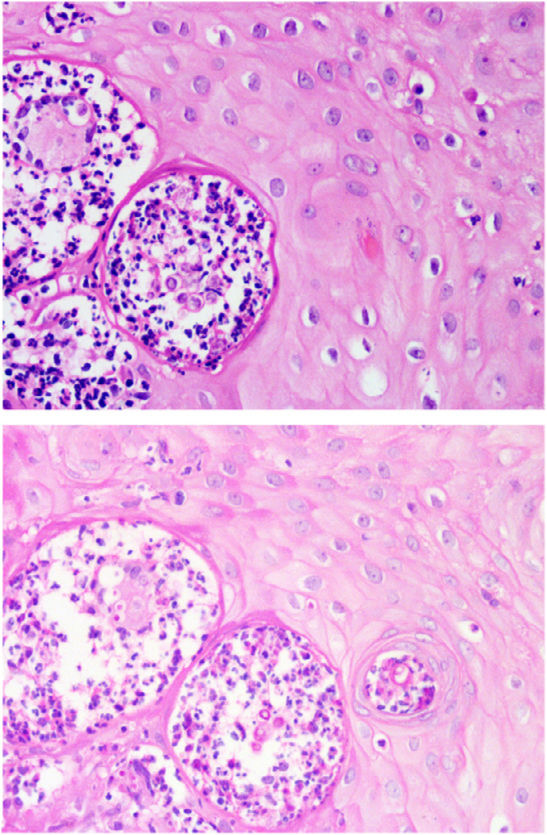
HistopathologyHistopathological examination confirmed the presence of pseudoepitheliomatous hyperplasia of the epidermis and a dense dermal inflammatory infiltrate with formation of suppurative-type granulomas. Fungal spores with multiple exospore projections were seen in the cytoplasm of multinucleated giant cells and in the stroma (figure 2, top, 40x, hematoxylin and eosin), which stained positively with PAS staining (figure 2, bottom, 40x, PAS).
Other supplementary studiesDirect examination of the lesion and sputum revealed the presence of fungal spores with birefringent walls and exospore projections. Both mycological cultures tested negative after 45 days of incubation. The thoracic tomography scan showed consolidations with a bilateral micronodular pattern and septal thickening.
What is the diagnosis?
DiagnosisChronic multifocal paracoccidioidomycosis.
Treatment and disease progressionTreatment started with itraconazole 200mg/day. The patient showed clinical improvement within a week of starting treatment, and complete healing of the lesion in just 3 months (figure 3). At the time of this report, the patient remains on regular treatment and follow-up.
CommentParacoccidioidomycosis (PCM) is a deep mycosis caused by fungi of the Paracoccidioides genus, which is endemic in humid areas of Latin America, such as Brazil, Colombia, Argentina, Venezuela, Peru, and our country, Paraguay.1,2 Epidemiological data are not precisely known because PCM is not a mandatory reportable disease. However, it is estimated that the incidence of PCM in endemic areas is 3 to 4 new cases per year per million inhabitants.3
The chronic form is the most common one among adults, predominantly males. Most patients have a history of rural origin, tobacco use, and alcohol consumption. PCM can touch any organ, system, or apparatus, with varied and nonspecific clinical signs. Skin lesions occur in 30% to 54% of the patients, being the face the most common location and with an ulcerative-vegetative pattern.4
PCM can pose a diagnostic challenge due to the polymorphism of its presentation. This case is remarkable due to the exuberance of the skin lesion, which requires ruling out other infectious diseases such as leishmaniasis, tuberculosis, atypical mycobacteriosis, other deep mycoses, as well as epithelial neoplasms such as basal cell or squamous cell carcinoma.4 However, in the case reported here, the patient's epidemiological characteristics suggested the need to rule out the presence of deep mycosis.
It is known that the definitive diagnosis is achieved by identifying Paracoccidioides in culture or through molecular biology (PCR) of the affected tissue. However, the performance and availability of these studies are limited.5 Diagnosis based on the identification of multiple budding yeast through direct examination or in pathological anatomy is a rapid, cost-effective, and valid alternative, since the therapeutic approach for other fungal variants found with these methods is similar.
Starting treatment early is crucial regarding prognosis, because these lesions can progress to fibrosis, resulting in permanent anatomical and functional changes.6
FundingThis study was funded by the authors themselves.
Conflicts of interestNone declared.