A 22-year-old woman with no significant past medical history presented to the clinic with a 2-month history of an asymptomatic skin eruption on her right upper extremity. Over time, the lesions had grown in both number and extent. The patient denied any previous bleeding or trauma in the affected region.
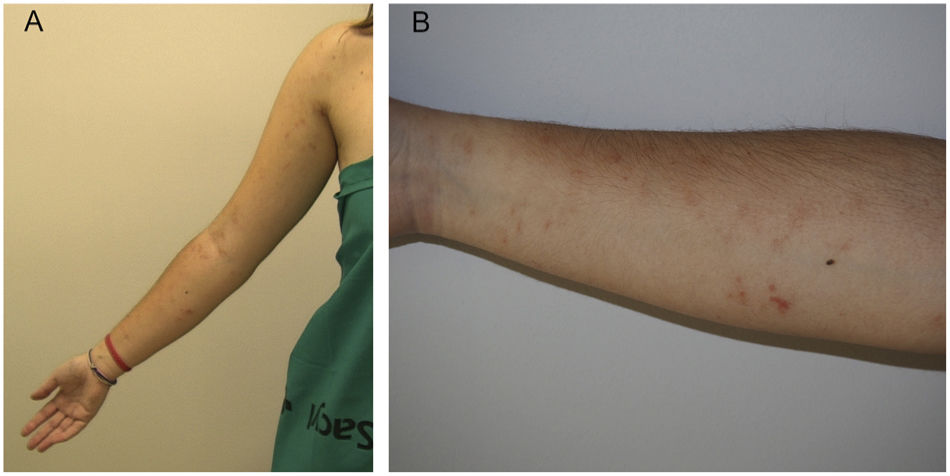
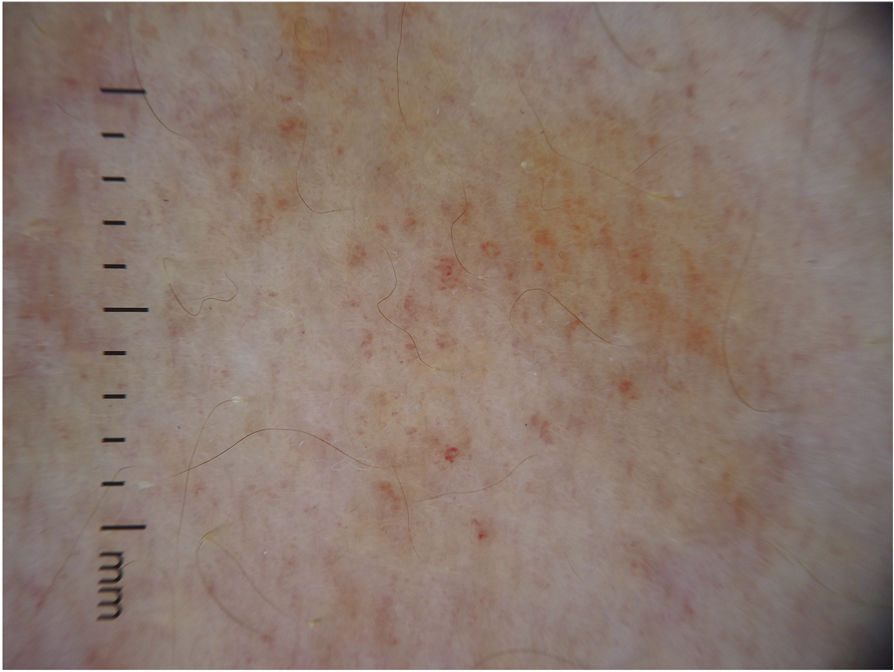
Physical examinationSkin examination revealed the presence of reddish-brown macules strikingly distributed in a linear pattern on the anterior and inner regions of the patient's right arm and forearm (fig. 1). On closer inspection, the lesions were composed of pinpoint petechiae (fig. 1B). Dermoscopy showed the presence of red dots and lines over a homogeneous brown area (fig. 2).
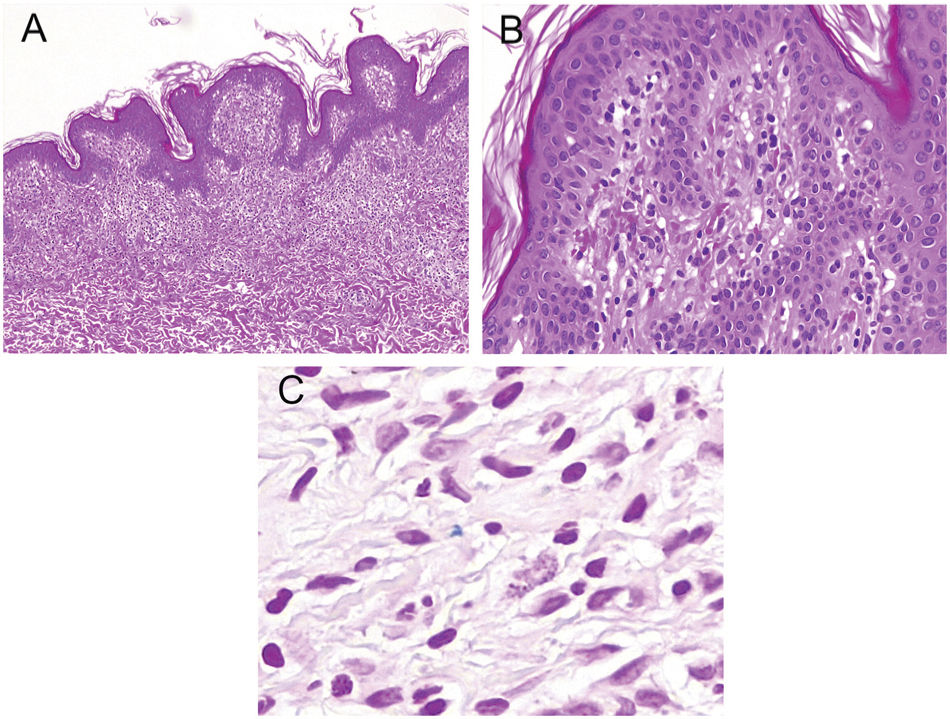
HistopathologyA slight perivascular lymphohistiocytic infiltrate with focal erythrocyte extravasation was identified, without other notable findings (fig. 3A and B). Perls’ staining showed of a few iron deposits on the superficial dermis (fig. 3C).
Additional testsA complete blood test, including platelet count, coagulation study, and vitamin C levels, revealed no other pathological findings.
What is your diagnosis?
DiagnosisUnilateral linear capillaritis (ULC).
Disease progression and treatmentGiven the nature of this condition, the absence of symptoms, and the tendency for spontaneous resolution, we decided no to treat the patient. The lesions disappeared within 6 months without leaving any scars or post-inflammatory hypo- or hyperpigmentation.
CommentULC is a rare variant of pigmented purpuric dermatosis (PPD), first described by Riordan et al. in 1992.1 ULC is characterized by purpuric macules with a linear or pseudo-metameric distribution affecting a single limb.2 Although ULC typically occurs on the lower extremities of young men, it can also affect the upper limbs.3
PPDs are disorders caused by capillaritis of unknown origin. All the different entities within PPDs exhibit similar histopathological findings, such as perivascular lymphocytic infiltrates, erythrocyte extravasation, and hemosiderin deposits.4 The clinical features help differentiate the various subtypes of the disease.
The differential diagnosis includes other dermatoses of linear or Blaschkoid distribution, such as psoriasis, linear verrucous epidermal nevus, linear lichen striatus, linear lichen planus, certain viral exanthems, unilateral nevoid telangiectasia, and serpiginous angioma. Additionally, other PPD variants—particularly lichen aureus—should be ruled out as they can also clinically present with a linear or segmental morphology. In this regard, finding a dense band-like dermal infiltrate, separated from the epidermis by an unaffected papillary dermis area (Grenz zone), would be of interest.5 However, in our case, the rapid resolution of the lesions and the presence of vacuolar degeneration, along with a series of hemosiderophages, suggest ULC rather than lichen aureus.
As with other PPD variants, topical corticosteroids have proven effective for treating pruritus. Psoralens and UVA phototherapy, ascorbic acid, rutin, and griseofulvin have been used with variable effectiveness. The prognosis of ULC is good, with lesions typically resolving spontaneously within less than 2 years.1,3,5
In conclusion, we have described a case of a rare PPD variant—ULC— in a woman with an atypical location but with clinical, dermoscopic, and histological findings characteristic of this condition.
FundingNone declared.
Authors’ contributionsThe authors made substantial contributions to the idea and design of the study, drafting and critical revision of the manuscript, approving its final version for publication.
Conflicts of interestNone declared.