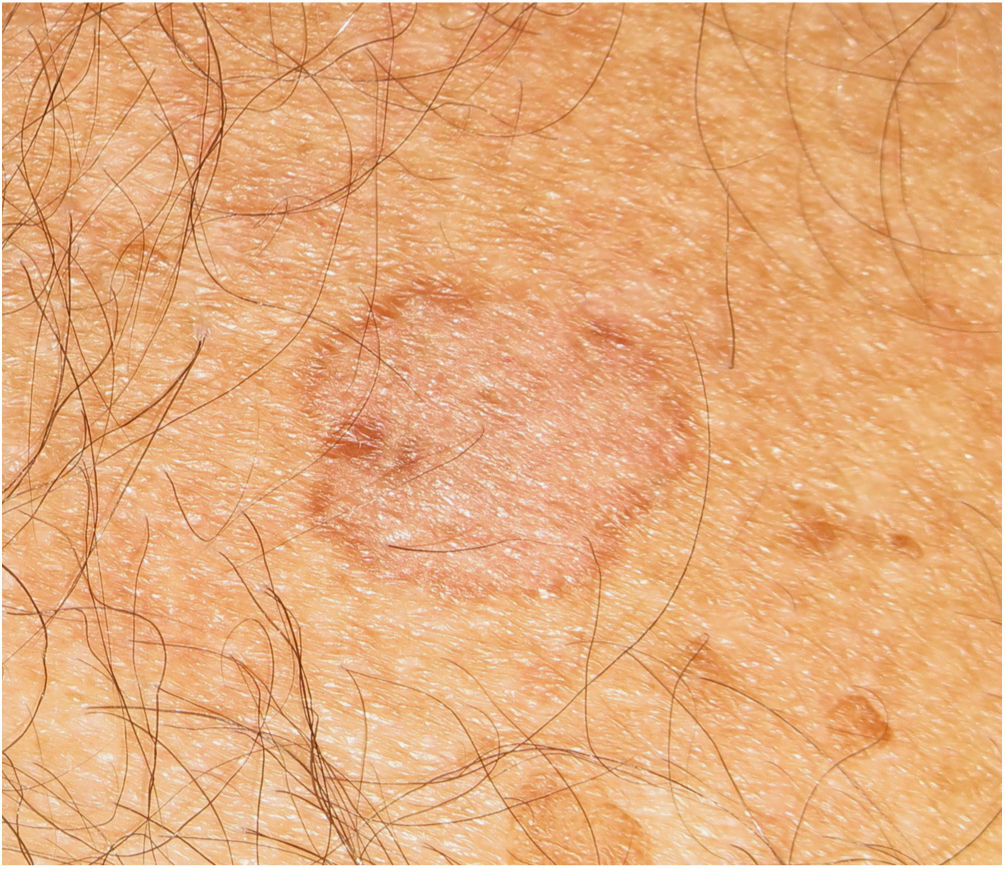
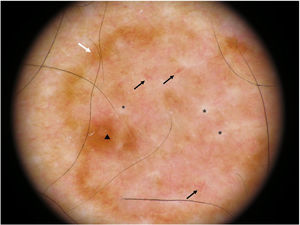
Examination of a 77-year-old man in the dermatology clinic revealed a 1.5-cm light brown spot with eccentric pigmentation in the right pectoral region (Fig. 1).
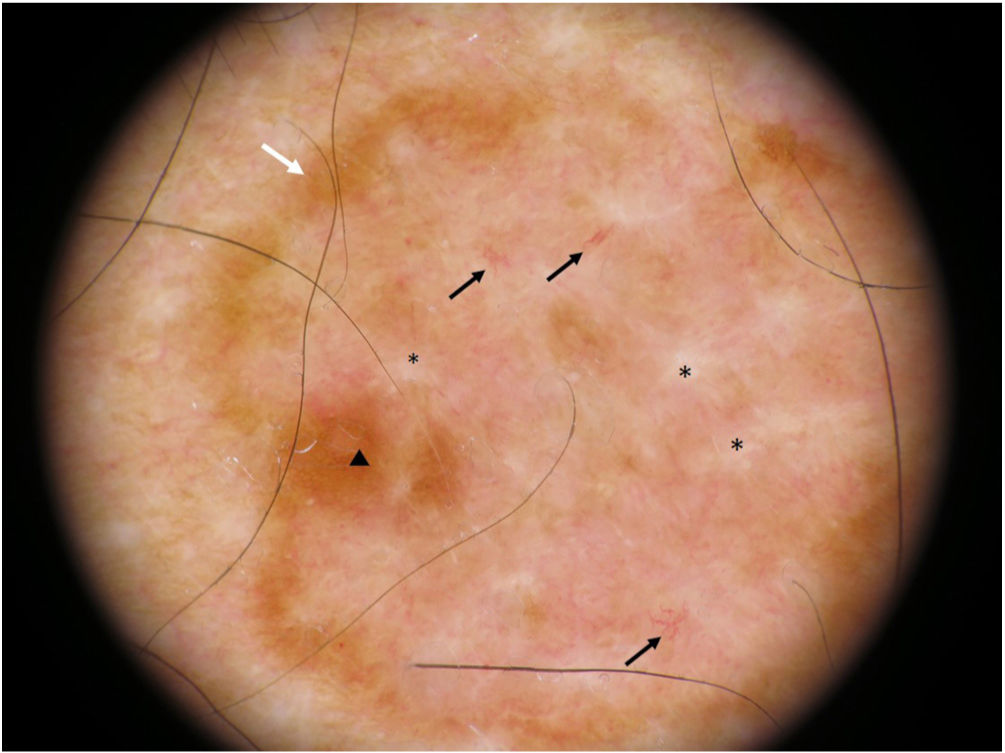
DiagnosisDermoscopic examination showed erased areas containing white lines and atypical vascularization in the center and a characteristic fine reticular pattern at the periphery (Fig. 2).
Dermoscopic image. Note the well-defined eccentric pigmentation (triangle), the characteristic reticular pattern at the periphery (white arrow), the structureless center with complete disruption of the reticular structure and white lines (asterisks), and the erythematous background with atypical vascularization (black arrows).
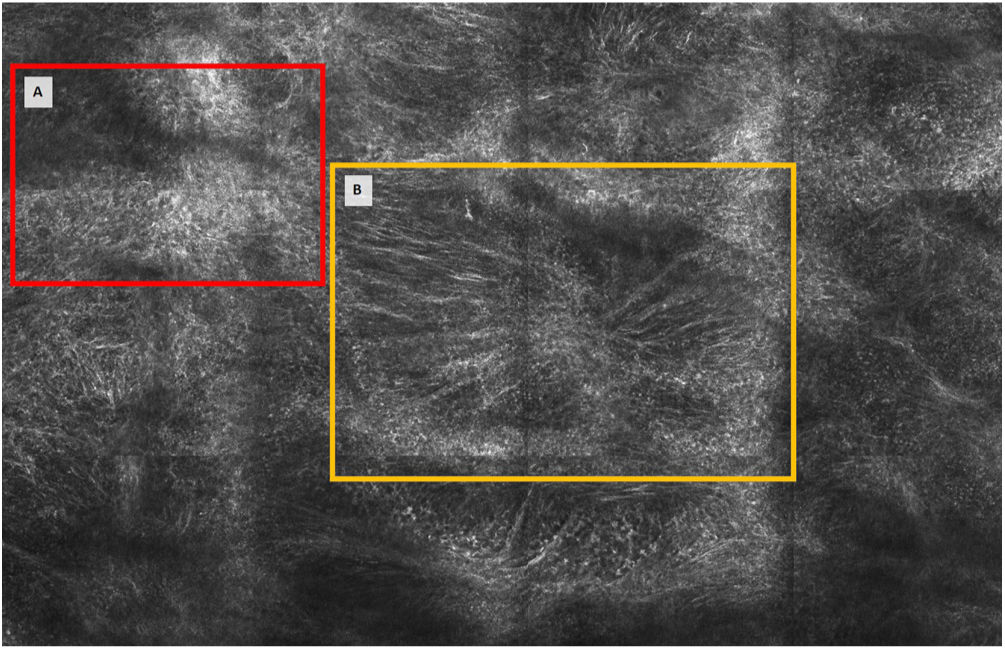
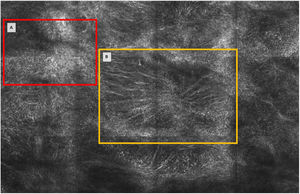
Examination by confocal microscopy showed an epidermis with abundant dendritic cells and numerous junctional thickenings at the dermoepidermal junction (Fig. 3). The lesion was excised and histologic examination confirmed a diagnosis of extrafacial lentigo maligna (LM).
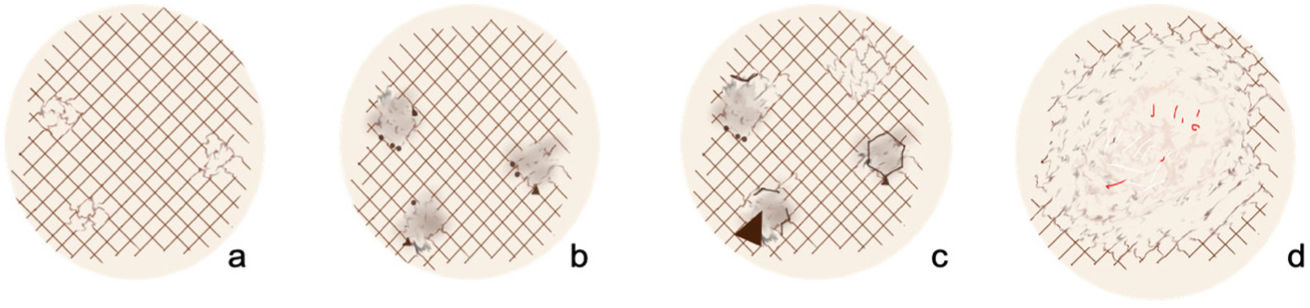
Extrafacial LM is a lentiginous form of melanoma associated with chronic sun damage.1 Its incidence is increasing in Spain for a number of reasons, including longer life expectancy and improved clinical identification of these lesions and their dermoscopic features.2–4 A clinical progression model with dermoscopic features (Fig. 4) based on confocal microscopy findings has been proposed for extrafacial LA.2,5 The first features observed are areas of reticular disruption, followed by erased areas surrounded by pigment dots and triangular structures, which progressively evolve to form angulated and zig-zag lines. More advanced lesions show large erased areas with atypical vascularization and typically contain traces of a fine peripheral reticular pattern pointing to the melanocytic nature of the lesion.2
Modified dermoscopic extrafacial lentigo maligna progression model adapted from Gamo-Villegas et al.2 A, Reticular disruption. B, Erased area and triangular structures. C, Angulated and zig-zag lines. D, Large areas.
The greatest diagnostic challenges are thus posed by early-stage lesions (when the only finding is reticular disruption) and advanced lesions (when practically all structures have been erased). Identification of advanced lesions is crucial. We recommend paying special attention to atypical vascularization, white lines, and the characteristic traces of the reticular pattern at the periphery.
FundingNone declared.
Conflicts of InterestThe authors declare that they have no conflicts of interest.