Surgery for an ingrown toenail of the great toe is a common procedure that requires an anesthetic neuromuscular blockade of the entire digit. Various digital block techniques have been described, but no evidence-based recommendations on the best choice have emerged. We aimed to compare the V block to the H block in this type of surgery.
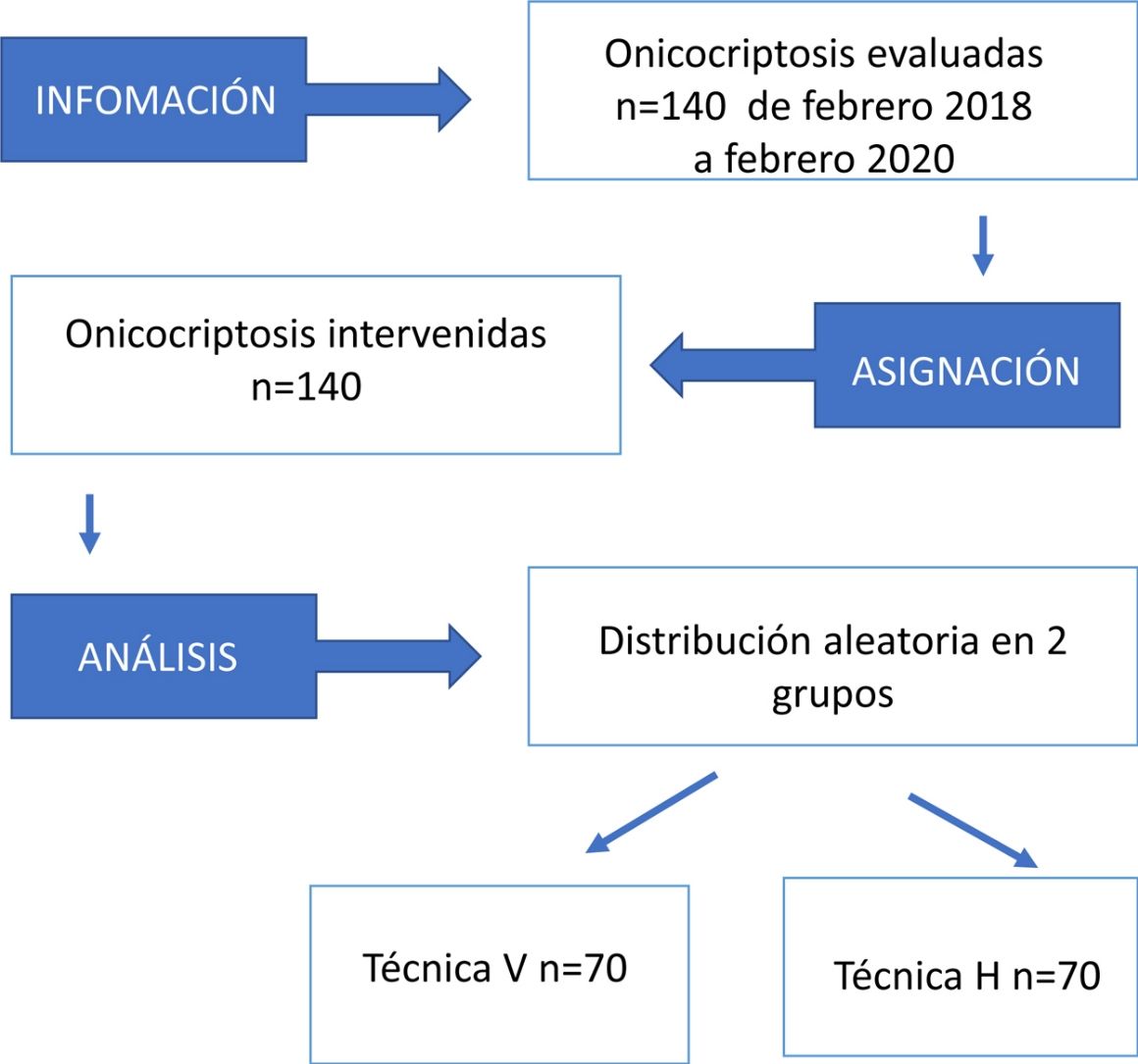
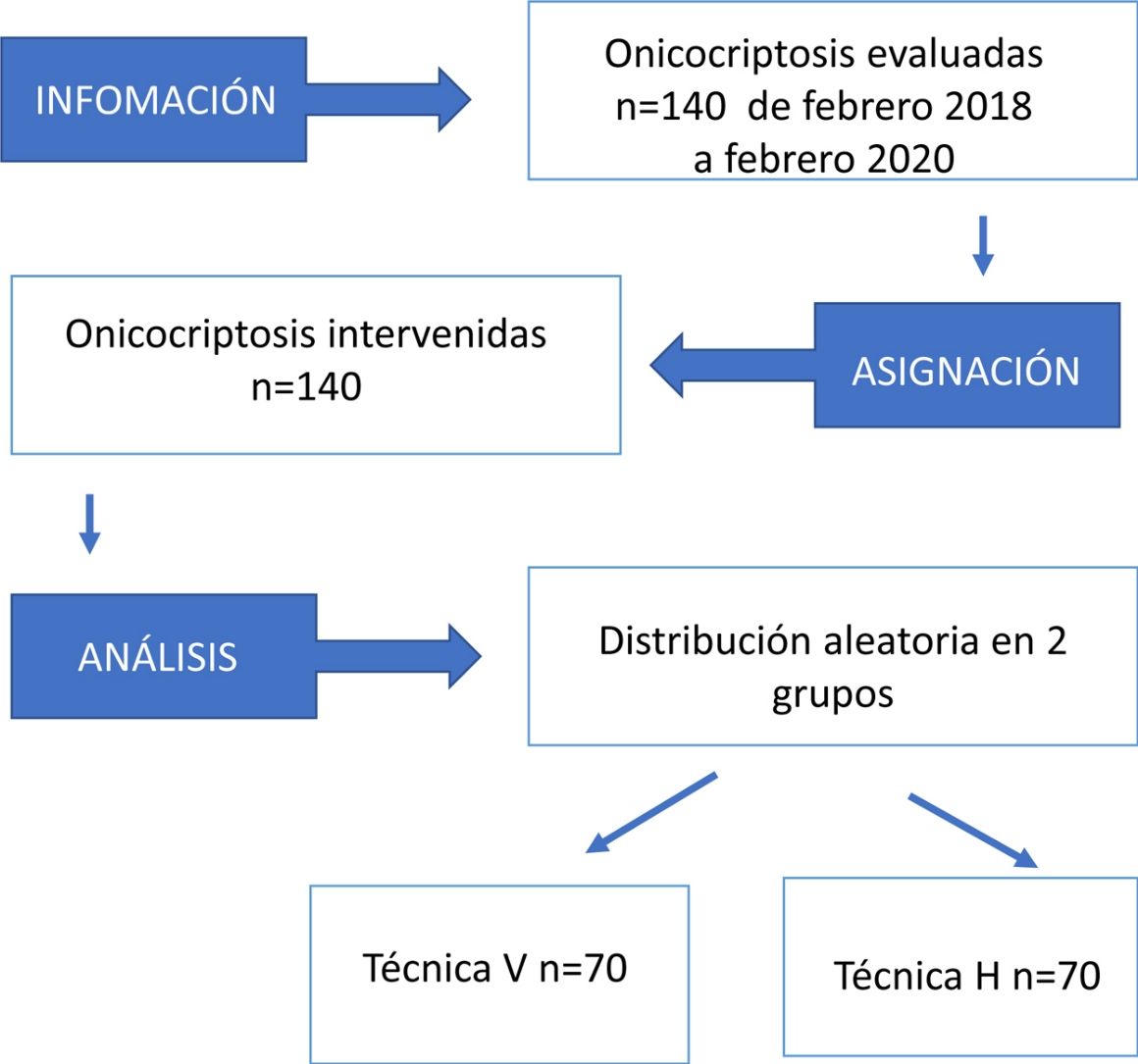
Material and methodsMulticenter randomized clinical trial in patients undergoing onychocryptosis surgery between February 2018 and February 2020. We recorded sex, age, foot intervened, type of blockade used (H block or V block), efficacy 10 and 20min after injection of the anesthetic, and number of attempts.
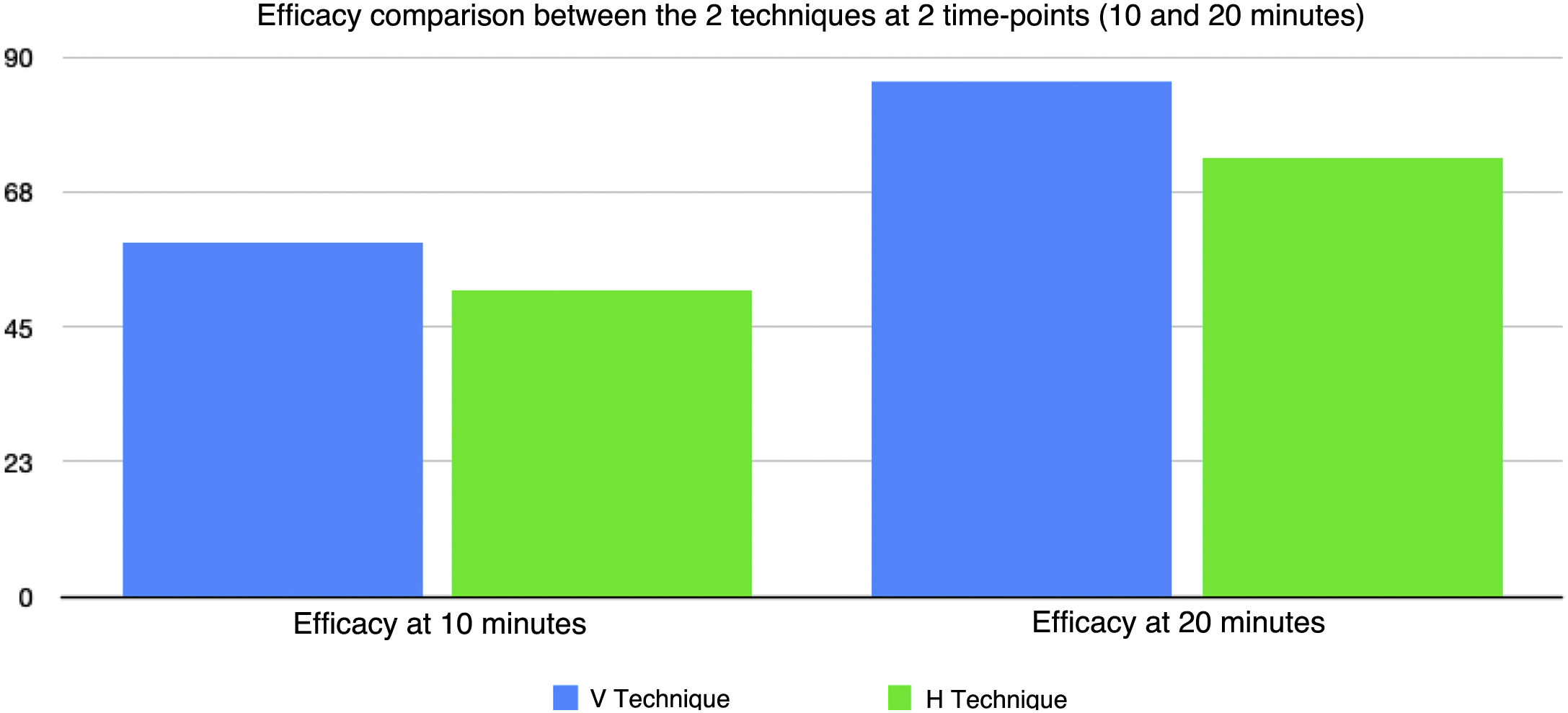
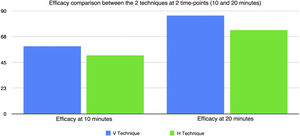
ResultsA total of 140 surgeries to treat ingrown toenails were assigned to 2 groups (H block or V block) of 70 patients each. The same anesthetic, dose, and volume were used in all cases. The V technique produced a better neuromuscular block in 7.2% more cases at 10min and in 12.8% more at 20min.
ConclusionsBoth block techniques are safe and effective. The V block is a good alternative to the H block in patients undergoing surgery to treat an ingrown toenail.
La cirugía en onicocriptosis del primer dedo del pie es un procedimiento común que requiere de un bloqueo anestésico completo del dedo. Existen diferentes técnicas, pero no hay recomendaciones basadas en la evidencia sobre el mejor tipo de técnica de anestesia. En este contexto, nuestro objetivo fue evaluar si el bloqueo anestésico en V presenta ventajas respecto al bloqueo en H.
Material y métodosSe realizó un estudio observacional, prospectivo y multicéntrico en pacientes sometidos a cirugía de onicocriptosis entre febrero de 2018 y febrero de 2020. Se distribuyó a los pacientes aleatoriamente en 2 grupos. Se recogieron los siguientes datos: sexo, edad, tipo de bloqueo según técnica (técnica H o técnica V), eficacia de la técnica a los 10 y 20min posteriores a la infiltración, pie afectado y número de refuerzos anestésicos.
ResultadosSe incluyeron 140 intervenciones quirúrgicas sobre uñas con onicocriptosis, que se dividieron en 2 grupos. Se compararon las variables después de realizar los distintos abordajes anestésicos con el mismo agente anestésico, dosis y volumen. A 70 intervenciones se les asignó la técnica H y a otras 70 intervenciones se les asignó la técnica V. Al analizar los tiempos de eficacia, se observó que la técnica V fue mejor en un 7,2% a los 10min y en un 12,8% a los 20min frente a la técnica H.
ConclusionesLos 2 métodos de bloqueo anestésico son seguros y eficaces. La técnica V es una buena alternativa a la técnica H en pacientes sometidos a cirugía de onicocriptosis.
Onychocryptosis, also known as ingrown toenail, is a nail condition that occurs when the lateral nail folds penetrate the skin and cause inflammation and pain/infection.1 The condition usually presents on the great toe, although it can occur on other toes. The most frequent causes are incorrect nail cutting, hereditary factors, biomechanical or structural abnormalities of the foot, hyperhidrosis, and inappropriate footwear.2
When conservative treatment is not effective, surgery is needed. We have undertaken a review of this condition, as well as the anesthetic techniques used for surgery.
Different surgical techniques have been described for treatment of ingrown toenails,3,4 with phenol-alcohol procedures being the most widely studied and used.5,6
All these surgical procedures are performed under local anesthetic. Of the possible local anesthetic techniques, digital nerve block is the most widely used for the great toe.7
The most widely known digital nerve block for the great toe is ring block or H block, first described by Frost in 1952.8 This requires 2 injection sites, one on each side of the proximal phalanx of the great toe, with the needle directed laterally towards the dorsal aspect.
Inappropriate execution of this anesthesia technique, which may depend on the characteristics of the patient and the experience of the surgeon, is associated with poor diffusion of the anesthetic, and further injections may be necessary. When this occurs, several injections are required, increasing the dose of anesthetic, and postoperative pain in the injection site.
An alternative to H block is V block, first described in 2017.9 This is a new technique, with a steeper learning curve, but one which allows anesthetic block of the great toe with a single injection to the dorsal area of the proximal phalanx followed by pointing the needle laterally in 2 directions.
As there are no comparative studies of the effectiveness of these techniques in terms of latency time and duration of the anesthesia, it is not clear which is most appropriate for onychocryptosis surgery of the great toe.
In this study, these 2 local anesthetic techniques were compared with the aim of observing possible differences and advantages with each one.
Material and MethodsThis was an observational, multicenter, prospective, randomized study to compare the 2 anesthesia techniques, where efficacy was assessed at 10 and 20min after the intervention (H or V block).
The procedures were conducted in the Clínica de Podología SS and in the Hospital Clinic, Barcelona, Spain.
Approval was obtained from the ethics committee of the University of Barcelona, with registry number IRB 00003099, the Drug Investigation Ethics Committee of the Hospital Clinic, Barcelona, with registry number HC 2019/0051, and the Drug Investigation Ethics Committee (CEIm) of the Hospital Odontològic Universitat, Barcelona, with registry number 2007-43.
All patients were provided with the necessary information prior to anesthesia and surgery, and all signed an informed consent. In the case of minors, consent was signed by their parents or legal tutors.
The first patient was enrolled in February 2018 and the last in February 2020.
The study included patients of both sexes and different ages, with Mozena stage I and II (IIA and IIB) ingrown toenail and ASA I and II physical status according to the American Society of Anesthesiologists.
Those patients with a history of sensitivity or allergy to amide local anesthetics, those who were pregnant or lactating, and those with infection, neuropathy, cognitive deficit, and Raynaud syndrome were excluded.
A clinical protocol was designed that included data collection. For every patient, sex, age, and type of block (H or V technique), the efficacy of blockade after 10 and 20min after injection, the foot affected, and number of booster anesthetics were recorded.
The participants were divided into 2 groups according to the anesthetic technique (H/V block). Patients were randomly assigned to the type of anesthetic block using the number of their medical history; those whose medical history number ended with an even digit were assigned to H block while those whose number ended with an odd digit were assigned to V block.
ProcedureBefore starting the anesthesia, an aseptic foot-cleaning protocol was followed (shaving, cleaning with soaped sponges, and application of povidone/iodine solution).
The device used was a 5mL syringe with a 0.6×25mm 23G needle.
In both techniques, anesthetic block of the great toe used a 5mL solution of lidocaine B anesthetic. Braun 20mg/mL solution for injection (lidocaine hydrochloride) without epinephrine was used, always within the safety limits, below the maximum dose (400mg).
An aspiration test was applied before each injection to avoid intravascular infiltration.
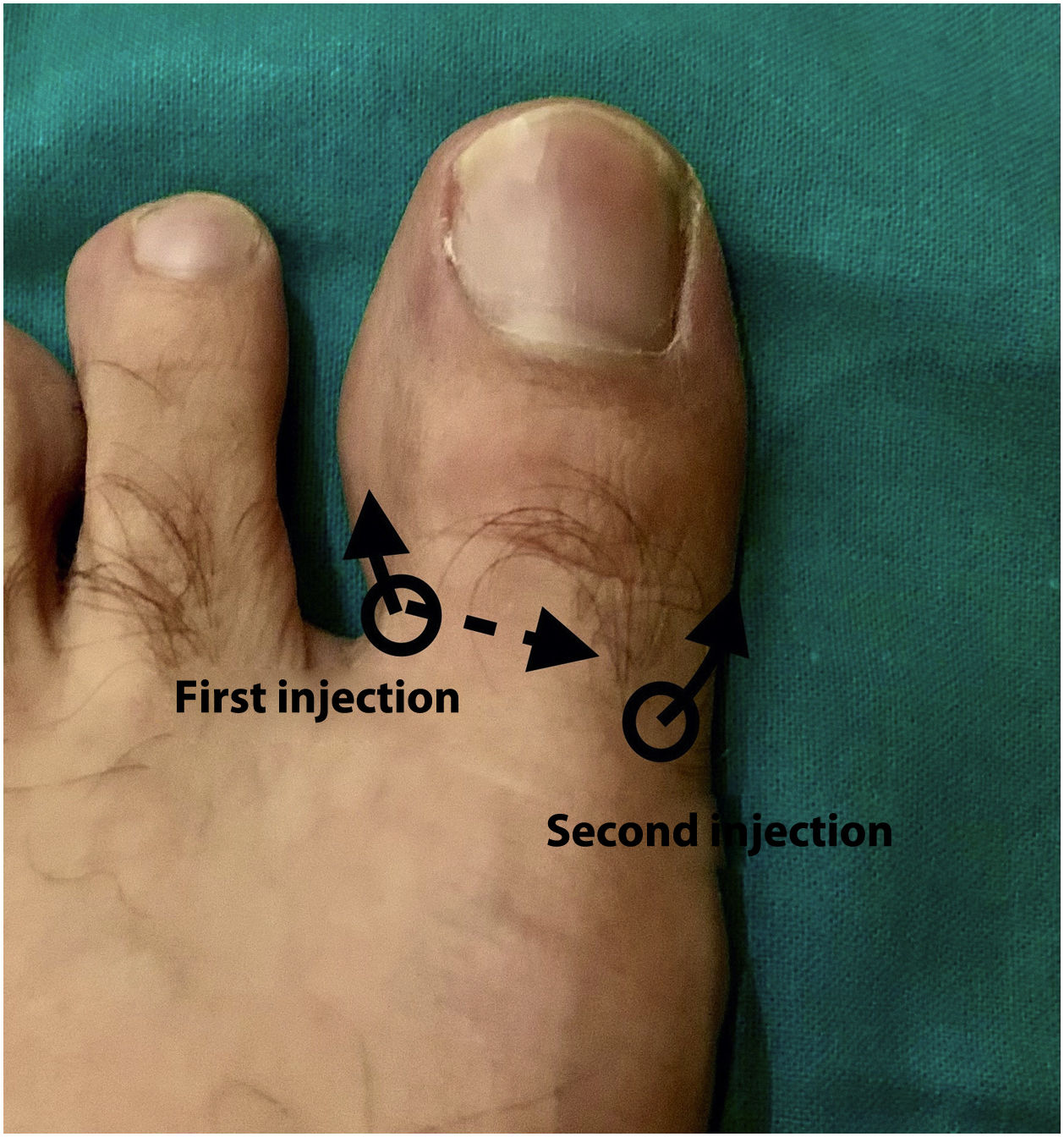
Description of the H TechniqueIn the H technique (Fig. 1), 2 injection sites are used on either side of the toe, directing the needle laterally after 1 of the injections.
Performing the H technique. First injection at the dorsal level in the peroneal canal, directed underneath the long extensor of the great toe and then towards the plantar region. The second injection is performed in the dorsum of the great toe in the tibial canal directing the needle towards the plantar region.
The first injection site is in the dorsal medial (peroneal) aspect of the toe and we inject 2mL of anesthetic solution.
Once the anesthetic agent has been introduced, and without fully withdrawing the needle, it is turned 90 degrees, and a slight dorsiflexion of the toe is done to pass the needle underneath the extensor tendon of the toe where we inject 1mL of anesthetic solution.
The second injection site is in the dorsal lateral (tibial) aspect of the toe and 2mL of anesthetic solution are injected.
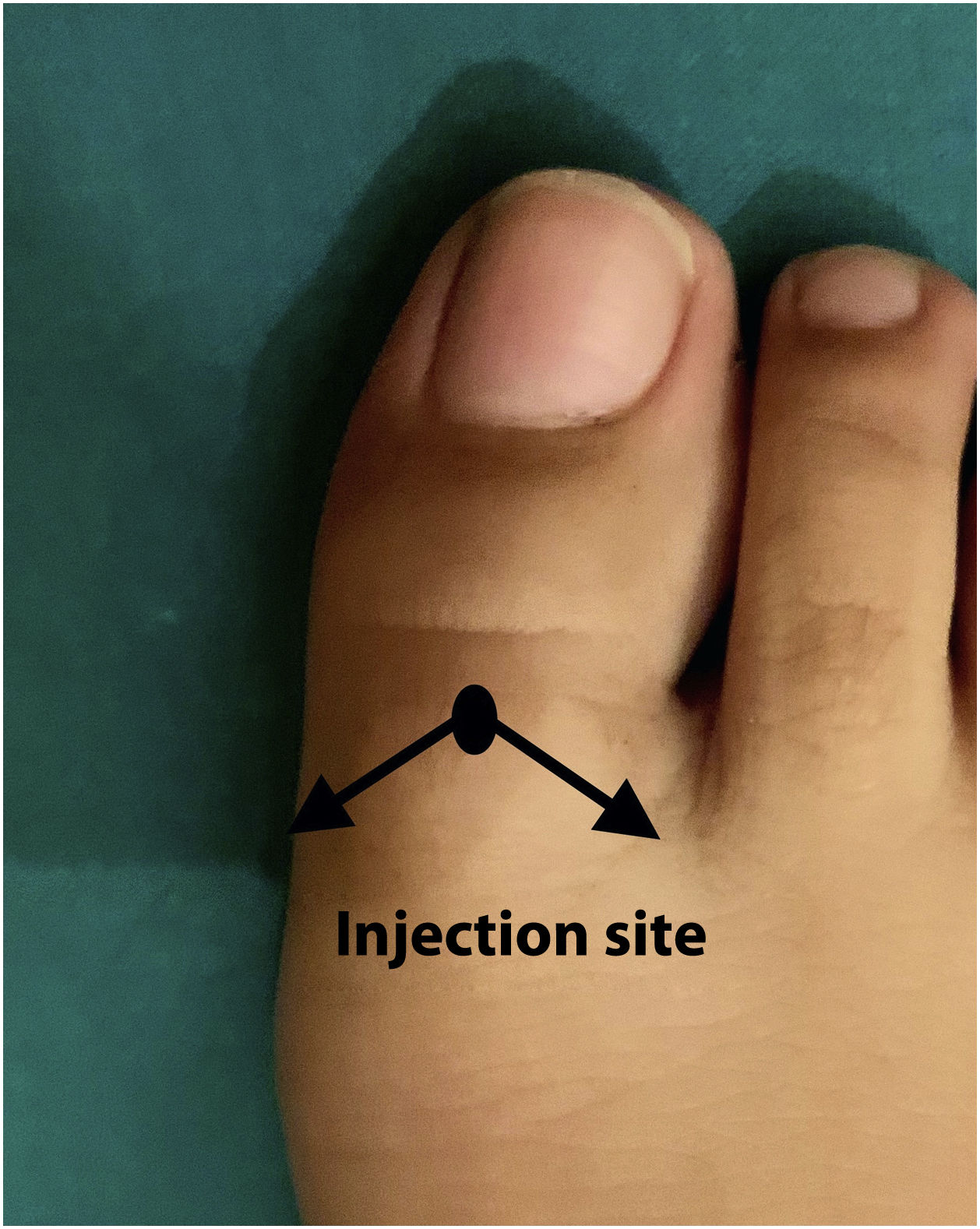
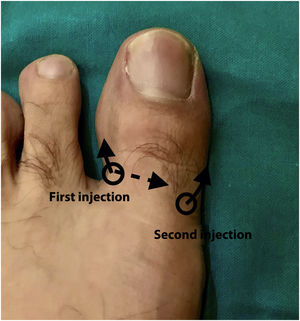
Description of the V TechniqueIn V block (Fig. 2), a single injection site is used in the dorsum of the toe, with the needle pointed laterally in 2 directions.
We pinch the dorsum of the toe slightly with our fingers above the proximal phalanx, and then perform subcutaneous injection above the long extensor tendon of the great toe. The injection is made vertically, with aspiration prior to injection of 1mL of anesthetic.
Then, without removing the needle, this is turned 45 degrees and pointed towards the lateral/proximal area of the phalanx in the direction of the plantar aspect of the toe. With this maneuver, the tibial canal of the nail is blocked.
One mL of anesthetic is used in the plantar region and the needle is withdrawn towards the dorsum raising wheals with a total volume of 2mL of solution.
Subsequently, starting from point 1, the same maneuver is performed in the medial/proximal area, pointing the needle 45 degrees towards the plantar area, to anesthetize the peroneal canal of the nail. One mL of anesthetic is used in the plantar region and the needle is withdrawn towards the dorsum raising a wheal with a total volume of 2mL of solution.
Confirmation of Anesthetic EffectThe effect of anesthetic block was assessed 10 and 20min after performing each of the 2 techniques. Timepoints for assessment of the anesthetic effect were selected according to the latency time of lidocaine: 5–10min corresponding to onset of the initial effects and 20min, that is, twice the time of onset of latency.
To assess the effect of anesthetic block after performing one of the 2 anesthesia techniques, the sides of the toe were pinched with Adson forceps and the patients were asked whether they felt the anesthetized toe, with lack of feeling or loss of feeling of pain.
In terms of the anesthetic effect, those patients who did not perceive complete anesthetic block underwent further rescue injections in the areas of the toe without sensation of anesthesia.
ResultsThe final study sample consisted of 140 surgical procedures on ingrown toenails (52 males and 88 females) with a mean age of 40.93 years and a range of 12–90 years.
In 72 patients, the ingrown toenail was on the right foot, and in 68 it was on the left.
A total of 70 interventions for ingrown toenail (19 males and 51 females) used V block and a further 70 (33 males and 37 females) used H block.
The anesthesia times were longer with the V technique. At 10min after the V technique, 58.6% of patients had complete anesthetic block; at 20min, this percentage increased to 85.7%. Additional rescue injections were only needed in 14%.
With the H technique, 51.4% and 72.9% had anesthetic block after 10min and 20min, respectively. Additional rescue injections were needed in 27% (Fig. 3).
DiscussionThe present study aimed to assess the efficacy and safety of 2 types of anesthetic block in the feet of patients with ingrown toenails. In these cases, the operation can only proceed if the block has been correctly performed.7–9
The ideal anesthetic should allow painless surgery, without anesthetic and local complications. It should be inexpensive and permit the procedure to be performed without stress for the surgeon or patient.10,11 Likewise, the choice of anesthetic technique should be on a case-by-case basis, according to the needs of each patient, the predicted duration of surgery, and the preferences of the surgeon.11
Although different agents are used for anesthetic block of the great toe, there is no consensus about the best anesthetic agent, with lidocaine and mepivacaine being the most widely used local anesthetics.
In the literature, there are several articles that compare these anesthetics with and without adrenaline, but there are no publications that explain how to appropriately perform anesthetic block of the big toe or that compare the different types of block.
Based on the literature and our clinical practice, in this study we used lidocaine as an anesthetic agent, given the large number of publications that support its safety and tolerability in different situations and specialties. Lidocaine is the most widely used local amide anesthetic for comparative studies of anesthetics.12 It was developed in 1943 by the Swiss Nils Lofgren and his colleague Bengt Lundqvist12 and is characterized by rapid onset of action, in around 5–10min, and a moderate duration of action of 1.5h.13,14 It is metabolized mainly by the CYP3A4 enzyme in the liver into pharmacologically active metabolites15 and is an appropriate choice of drug for infiltrations and regional and surface anesthesia.15
In the current economic climate, also of particular consideration is its low cost, without compromising patient safety. Lidocaine is actually slightly cheaper than mepivacaine.
All these characteristics make lidocaine one of the most suitable anesthetics for surgery of ingrown toenails.
There is, however, certain debate concerning the volume of anesthetic to use. Some authors favor using 2–3mL, with the understanding that larger volumes could cause ischemia in the great toe. Others, however, suggest using vasoconstrictors along with the anesthetic to reduce the total volume of anesthetic used.16,17
In our study, we did not use a vasoconstrictor and we found that there was no tissue damage or necrosis with a volume of 5mL.18
In all patients who participated in the study, the anesthetic blocks described earlier were applied uniformly without inducing ischemia. This is an important point, as the presence of ischemia increases the anesthetic effects regardless of the local anesthetic used. Once the anesthesia had been performed, it was verified that the area of the intervention was under complete anesthetic block before starting surgery. Subsequently, ischemia was induced at the base of the proximal phalanx of the great toe before starting surgery, without detecting intra- or postoperative bleeding.
To achieve appropriate anesthetic block, not only is the choice of anesthetic agent important but also the type of anesthetic block. H block requires 2 injection points whereas V block has the advantage of achieving greater anesthetic block with a single injection site. A single injection site could help reduce the patient's level of anxiety and also the risk of potential adverse effects such as vasovagal reactions.
Of note with the results was that although there were no significant differences between the 2 techniques, V block was effective in 85.7% of patients at 20min compared with 72.9% with H block at the same time-point and with the same anesthetic agent and volume of drug. Thus V block achieves 12.9% more anesthesia than the H technique.
In a small study conducted and published in 2020,19 in which these 2 anesthesia techniques were compared in the great toe of 16 patients with infected ingrown toenail, the V technique was more effective in 87.5% compared with 62.5% for the H technique. It therefore follows that the H technique reduces its anesthetic effect in infected ingrown toenails, as in our study the H technique was effective in 72% in patients without infection.
This could be because we inject the drug in an area further from the site of infection with the V technique compared with the H technique, and so the medium where the drug is injected has a different pH.
Another important advantage of the V technique compared with the H technique is the distribution of the anesthetic, given that 1mL is injected at the plantar level, raising small wheals when the needle is withdrawn, which could increase the efficacy of the V technique.
In addition, given the V technique requires a single injection site, the duration of the procedure is reduced and possibly, as mentioned earlier, the patient's anxiety is also reduced because of reduced discomfort with a single injection.
Although multiple injection techniques are associated with high success rates (90%), they are also associated with a risk of almost 1.7% of nerve damage20 if the path of the needle is close to the neurovascular bundle. Aspiration by withdrawing the plunger of the syringe before injection confirms that the needle is not in a vessel and so there is no risk of injecting the drug systemically thus potentially causing unwanted adverse effects.
There were no reports of paresthesia or other anesthesia-related symptoms in patients who participated in our study.
One of the limitations of our study was the number of patients included. A sample size calculation was performed and 126 subjects were found to be needed in each group to obtain conclusive results with statistical significance (confidence level of 95%). Therefore, a larger sample would be needed to confirm these differences between the 2 local anesthesia techniques.
Another limitation is the lack of prior studies defining or highlighting the differences between the 2 anesthetic block techniques for the great toe. We have therefore been unable to compare our own findings with those of other investigators or publications.
We also believe that it would have been interesting to measure the severity of pain immediately after anesthetic block with a visual analogue scale and compare the 2 techniques.
Another very interesting question would have been to count the number of positive aspirations. This would provide further information when selecting the best technique to use, as we could reduce the risk of complications due injection of anesthetic in blood.
It would also have been useful to measure the latency times of the anesthetic after performing each of the techniques to be able to compare the results of this study with pre-existing ones.
ConclusionBy way of conclusion for the present study, we can affirm that there are few studies supporting the use of anesthetic techniques in surgery for ingrown toenails. Although the present study has some limitations, our results suggest that both procedures are simple and well tolerated by patients, and that the V technique is a safe alternative to the H technique in patients who require surgery for ingrown toenail on the great toe.
The V technique is superior to the H technique in terms of greater anesthetic effect at 10 and 20min, and could be the better option in infected ingrown toenails and in patients sensitive to pain, given that it is potentially less painful to perform because it requires a single injection.
Conflicts of InterestThe authors declare that they have no conflicts of interest.