Endovascular embolization is the first-line treatment for intracranial aneurysms and vascular malformations. The possibility of inducing transitory secondary alopecia with this technique is well known by interventional neuroradiologists, but has received little attention in dermatology publications and even less in the dermatopathology literature, in which there are still no published descriptions of the histopathologic findings characteristic of this condition.
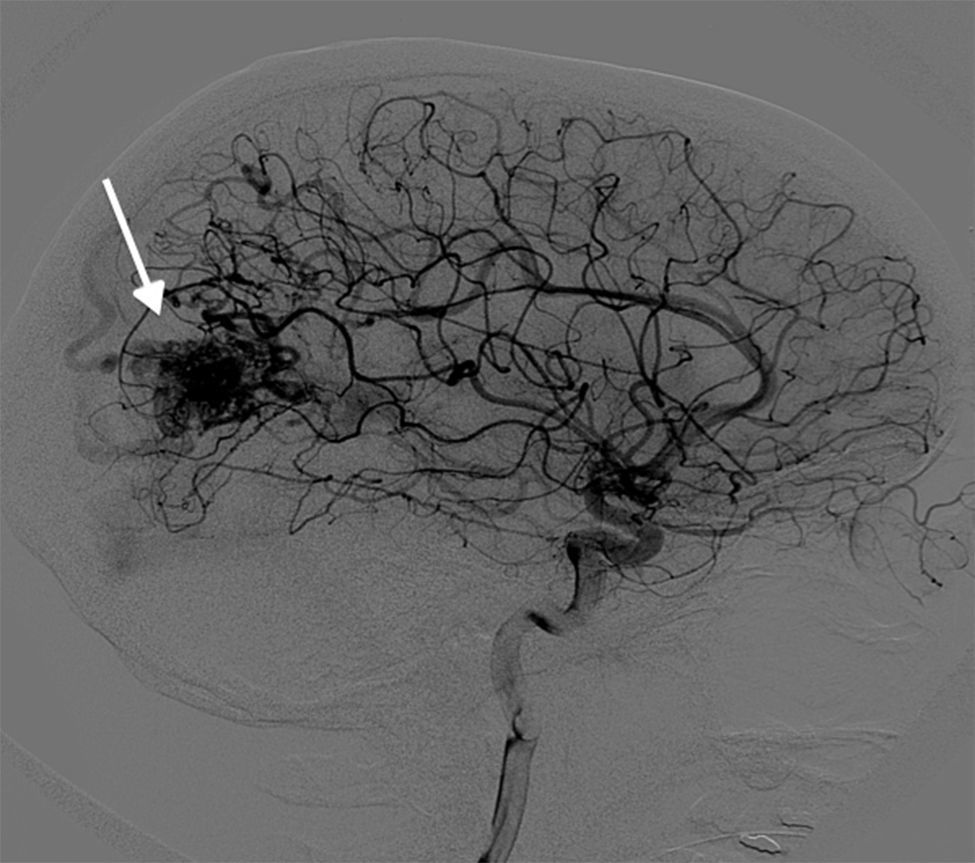
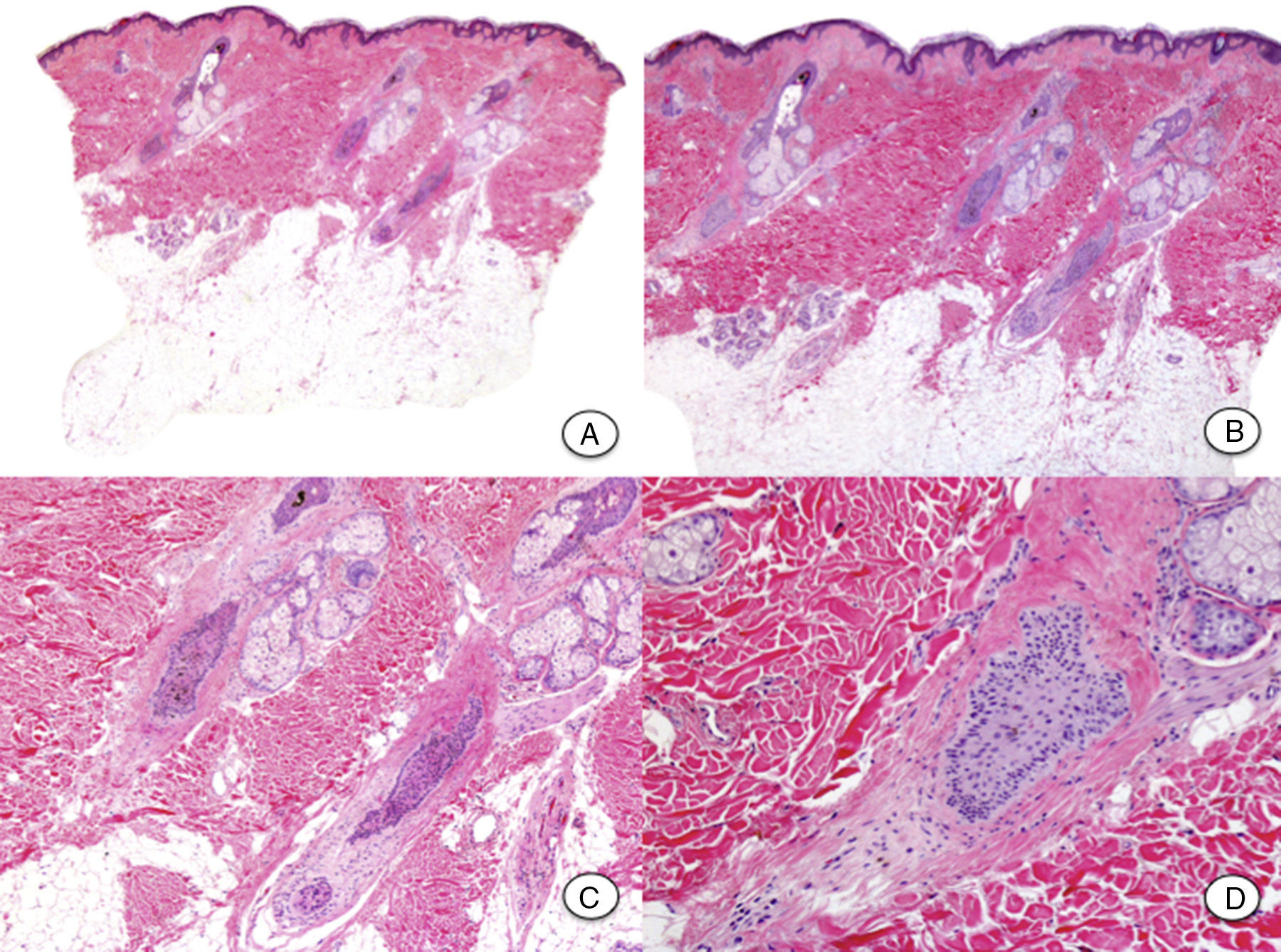
We report a new case of transitory rectangular alopecia after endovascular embolization and provide the first description of its histopathologic characteristics. The patient was a 32-year-old woman who underwent endovascular embolization to treat an intracranial arteriovenous malformation (Fig. 1). She consulted for hair loss of rapid onset in the left parieto-occipital region 1 month after the procedure. On physical examination, a well-defined rectangular plaque of alopecia with a strongly positive hair pull test was present in the left parieto-occipital region (Fig. 2). On trichoscopy, dystrophic hair shafts were observed in the follicular orifices, with no exclamation mark hairs. A skin biopsy taken from the plaque of alopecia revealed a high percentage of follicles in catagen, with no signs of damage to the follicular epithelium or radiodermatitis. The hair follicles appeared retracted, with an undulating, corrugated outer root sheath and with the presence of apoptotic cells (Fig. 3). In addition, the typical fibrous stela of follicles in catagen extended beneath the follicular bulb. It was decided to take a wait-and-see approach, without performing treatment. The plaque of alopecia showed a spontaneous and progressive improvement, with complete repopulation within 2 months.
Histopathology after staining with hematoxylin and eosin. A, No hair follicles are visible in the hypodermis. B, The dermis is spared and presents retracted hair follicles with no inflammatory infiltrate. C, The outer root sheath of the retracted hair follicles has an undulating, corrugated morphology, typical of catagen phase. D, Characteristic fibrous stela of follicles in catagen.
Alopecia after radiotherapy to the head and neck is extensively documented in the literature; however, few reports have been published on alopecia after diagnostic and therapeutic endovascular procedures and the condition is probably underdiagnosed. Fluoroscopy, a technique that uses the fluorescent properties of x-rays to obtain images in real time, is an important aid when performing endovascular embolization as it allows us to take video images of, for example, the movement of fluids. Taking images over a long interval can give rise to radiation-induced adverse effects, as patients receive high doses of radiation to a single area. Transitory rectangular alopecia after endovascular embolization is considered to be a specific form of acute radiodermatitis caused by the marked sensitivity to radiation of scalp hair follicles in anagen.1 The follicular cycle is interrupted abruptly by an acute lesion of mitotically active cells in the follicular matrix. This produces a premature and synchronic entry of all follicles into catagen phase, and the hair shafts are eliminated from affected follicles. However, the follicular cycle reinitiates when the harmful stimulus ceases, hence the complete repopulation of these lesions within 2 to 4 months after the procedure.1
The typical clinical presentation of transitory rectangular alopecia after endovascular embolization is as a plaque of alopecia of artifactual morphology that appears a few weeks after the intervention, in the area of scalp that received the highest dose of radiation. Onset depends mainly on total fluoroscopy time (more than 100minutes) and on the total dose received (definitive cicatricial alopecia will occur at doses over 7Gy and transitory alopecia at doses between 3 and 5Gy).2 However, when calculating the total radiation dose used in the intervention, it is important also to take into account prior diagnostic procedures that the patient has undergone, such as angiography, as the effects of these techniques on the hair follicles are cumulative.2,3 In addition, certain biological factors such as age, hair density, hormone status, and some genetic factors, can also influence the onset of this type of alopecia, although the underlying mechanisms are still poorly understood.4
It is important to differentiate transitory rectangular alopecia after endovascular embolization from postoperative alopecia and alopecia areata,4 as these are also nonscarring alopecias that are of rapid onset and present a circumscribed morphology. Postoperative alopecia is due to hypoxia caused by pressure on the reclined head during a long general anesthetic. Alopecia areata has a more complex and multifactorial etiology and pathogenesis. In the majority of cases, the diagnosis of transitory rectangular alopecia after endovascular embolization is based on the history of radiation to the area and the artifactual morphology of the lesions (typically rectangular). However, the absence of inflammation and the presence of dystrophic hair shafts can make it difficult to distinguish the condition from alopecia areata.1 In these cases, histopathology of a biopsy from the affected area is useful to differentiate the 2 entities. From a histopathological point of view, transitory rectangular alopecia after endovascular embolization should theoretically show changes compatible with anagen effluvium, associated with a minimal inflammatory infiltrate, although the findings will depend to a large extent on the moment at which the biopsy is performed. In our case, the biopsy showed a minimal inflammatory infiltrate and all the follicles were in catagen after the abrupt cessation of their cycle. We did not observe a honeycomb-like morphology of the infiltrate around the follicular bulb, typical of alopecia areata, or signs of radiodermatitis in the interfollicular epidermis or in the follicular epithelium. The absence of areas of scarring confirmed the transitory nature of the alopecia, as was observed clinically.
With the progressive increase in the number and complexity of endovascular embolization techniques, treating ever more complex lesions and requiring longer fluoroscopy times,5–7 it is likely that consultations for transitory rectangular alopecia after endovascular embolization will increase in the near future. It is therefore important that dermatologists are aware of the clinical characteristics and histopathologic features of this condition, so that they can reassure patients and inform them that the clinical course will be favorable.
Please cite this article as: Bernárdez C, Alcaraz I, Molina-Ruiz AM, Requena L. Transitory Rectangular Alopecia After Endovascular Embolization: A Case Report and Description of the Histopathology Findings. Actas Dermosifiliogr. 2015;106:848–850.