Compression therapy is the basis for treating the cause of venous ulcers and preventing recurrence. Various systems are currently available for applying compression, and adapting them to patients’ needs can improve adherence to treatment. Understanding the principles that underlie compression therapy is essential for success. Although this paper focuses mainly on venous ulcers, compression has also proven beneficial for other conditions, such as lymphedema and wounds resulting from injury or inflammation.
La compresión terapéutica es el pilar fundamental del tratamiento etiológico y de la prevención de recidivas de la úlcera venosa. En la actualidad disponemos de diferentes sistemas y estrategias para adaptar la terapia compresiva a las necesidades de cada paciente y aumentar su adherencia al tratamiento. Es fundamental el conocimiento de los principios teórico-prácticos de este tratamiento para lograr el éxito terapéutico. A pesar de que este artículo se centre fundamentalmente en la úlcera venosa, la terapia compresiva también ha mostrado un beneficio en otras patologías como el linfedema, las heridas post-traumáticas o las de causa inflamatoria.
Venous ulcer is the most advanced stage of chronic venous insufficiency, that is, the result of poorly controlled venous hypertension. The prevalence of this condition is increasing alongside aging of the general population.1,2
While some patients benefit from surgery or intravenous approaches for treatment of venous hypertension, compression therapy can be considered the mainstay for treatment of the underlying cause of venous ulcer. International clinical guidelines rate this type of therapy with level of evidence 1 and grade of recommendation A.3 However, despite its demonstrated effectiveness, appropriate compression therapy is not widely used for treatment of venous ulcer in Spain.4
Therefore, the objective of this paper is to review the theory supporting compression therapy, evidence in favor of its use, and its practical application in the treatment of venous ulcer and in the prevention of recurrence.
Compression therapy is applied to the leg mainly to increase venous and lymphatic return. The effects of compression go beyond merely reducing edema and play a role in tissue remodeling. Therefore, interest in compression therapy is not limited to the decongestion phase, but also covers maintenance treatment for venous edema, lymphedema, and phlebolymphedema.5
The main effects of compressive therapy are as follows6–9:
- -
Reduction in edema
- -
Tissue remodeling
- -
Reduced filtration of fluid from vessels to tissue
- -
Increased lymphatic drainage
- -
Release of anti-inflammatory mediators and reduction in inflammatory molecules and cells
Successful adherence to compression therapy requires the patient, the patient’s family, and, of course, medical staff to understand the indication for treatment. However, before providing the patient with explanations or recommendations, it is important to know his/her beliefs, previous negative experience, and social and family context.10
While the main indication for compression therapy in leg injury is treatment and prevention of venous ulcer, the interest of this approach is not restricted to this type of ulcer.
The inflammatory process underlying any leg injury involves abnormal microcirculation, with greater capillary filtration and increased intravenous pressure due to the effect of gravity. Therefore, despite the absence of reflux or obstruction, the patient may develop venous hypertension that hampers healing, thus making venous return by compression therapy essential.11 Irrespective of the cause (injury, surgery, vasculitis, pyoderma gangrenosum), compression therapy seems to be a good antigravity and anti-inflammatory approach for any leg injury providing there are no contraindications (see Contraindications).12–14
Properties of the BandageA band is known as a bandage when it is placed on a patient’s leg; therefore, its properties are different. A band is more or less elastic, whereas a bandage is stiffer or less stiff. Below, we provide the terminology used to discuss the properties of fabrics in vitro and in vivo.
Extensibility and elasticity:
Extensibility and elasticity are in vitro properties of the bandage or compression stocking.
Extensibility is the ability of the fabric to stretch in response to the tension applied. Elasticity is the ability to return to the original length when this tension is reduced. In simple terms, a stocking or bandage with considerable extensibility will also have considerable elasticity and vice versa. Bands can be classified according to their properties, and we generally refer to low and high elasticity (or short or long stretch).5
Multilayer and multicomponent:
The first characteristic is inherent to any type of bandage. A band applied to the leg will necessarily be a multilayered bandage, even if only 1 band is applied, since there is always some overlap between layers.
If we place 1 or more similar fabrics, the bandage is known as a monocomponent bandage. If we overlap fabrics with different physical properties, the bandage is known as a multicomponent bandage.
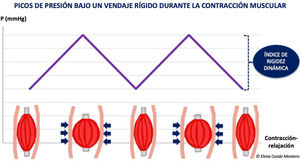
StiffnessStiffness is a property of the bandage and, therefore, an in vivo characteristic. Stiffness is defined as the resistance of the bandage to modifications in the volume of the calf muscles. The stiffer the bandage is, the more effective it will be for reducing venous hypertension while walking (ambulatory venous hypertension), since resistance to muscle contraction creates high-pressure peaks that lead to short and intermittent venous occlusions, much in the same way as the normal functioning of a valve.15 During rest, these peaks are not reached, and the pressure is lower (Fig. 1).
The concept of a “stiffer” or “less stiff” bandage should replace the current classification of a bandage as “elastic” and “inelastic”. Given that all bandages are multilayer and that many are multicomponent, the mechanical characteristics of a bandage vary with respect to those of the band. In fact, friction between the layers of a bandage increases the stiffness of the bandage, especially when a cohesive component is involved.5 The concept of friction also explains the greater stiffness resulting from the combination of 2 stockings (class I and II) than the application of a single stocking (class III).
Pressure Under the BandageProviding there are no contraindications (see Contraindications), healing of venous ulcers can be promoted by applying strong pressure on the ankle (> 30-40 mmHg). This pressure is measured using a device that is placed on the ankle and indicates the pressure applied in the area at rest (B1, transition between the Achilles tendon and the gastrocnemius). However, the pressure differs at the various points along the leg and depends on a series of factors, all of which are covered in the well-known Laplace law5: the pressure under the bandage at a specific point increases as tension increases (force applied to the bandage during placement), as the number of layers increases, when the radius is lower for the circumference at the specific point (greater prominence, e.g., pretibial region), and with a narrower band. The ability to maintain this degree of tension over time depends on the properties of the components of the bandage.
Padding techniques can be explained by this physical law. The main objectives of padding are as follows5:
To ensure a consistent leg circumference in patients with abnormal limb morphology (Fig. 2).
To protect bony prominences and other areas that are likely to be subject to excess pressure (e.g., the pretibial region and the area of the Achilles tendon) (Fig. 3).
To increase retromalleolar pressure in the case of wounds that lie behind the malleolus in order to overcome the “tent” effect that is usually observed in this concave area (Fig. 4).
To avoid venous congestion (erythematous-purpuric color) resulting from excess pressure on the cutaneous microcirculation and the more superficial venous system.
Contraindications and Special SituationsA review of guidelines and consensus documents, such as that performed by an expert panel in 2016,16 reveals considerable variability in the contraindications, risk factors, and complications associated with compression therapy.
Despite the heterogeneous nature of the recommendations, there is agreement on 2 absolute contraindications:
Occlusive artery disease with critical limb ischemia (ankle-brachial index [ABI], < 0.5).
Decompensated heart failure.
Given these contraindications, it is essential to suitably evaluate the wound, the leg, and the patient before prescribing any type of compression therapy. Palpation of the posterior tibial and pedal pulses is the first measure, and this is generally sufficient for application of compression therapy. If these pulses cannot be palpated, it will be necessary to measure the ABI. The ABI is the ratio of systolic arterial pressure in the ankle (measured in the posterior tibial and pedal arteries, selecting the highest value) to systolic arterial pressure in the arm. An ABI of 0.9-1.3 is considered normal. The cutoff point for critical limb ischemia is an ABI < 0.5; therefore, with a value of 0.6-0.8, despite the presence of peripheral artery disease, the patient can benefit from adapted compression therapy (stiff bandages and pressures below 30 mmHg) when indicated after evaluation by a specialist. Given that in some diabetic patients, this index may be falsely high owing to calcification of the arterial media, the patient should be referred to a vascular surgeon.5
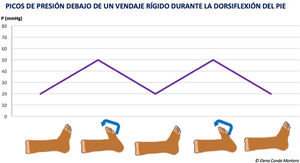
Relative contraindications also vary according to the guideline. Therefore, these relative contraindications should be understood as situations where compression therapy is to be used after taking into account specific considerations so that it is safe and well tolerated by the patient. Such situations include immobility and/or some degree of arterial disease: in the case of immobile patients with peripheral arterial disease and an ABI > 0.5, a bandage with a high stiffness index at pressures lower than 30 mmHg is a safe and effective option if the patient performs dorsiflexion exercises of the foot. Moreover, there may be a double benefit, since the reduced edema can improve arterial flow (Fig. 5).17
Despite the multiple potential comorbidities, the exhaustive follow-up of these patients makes compression therapy a safe technique.
Types of Systems and Materials in Compression TherapyLow-elasticity bandages (short stretch)The fabrics used in low-elasticity bandages stretch very little (less than 100%) or not at all (nonelastic bandages). One example of a nonelastic bandage is the zinc bandage, which is used for the traditional Unna boot and continues to be a very interesting alternative bandage, providing a specific anti-inflammatory benefit in stasis dermatitis.18 Bandages composed of nonelastic bands are stiff, with low resting pressures, high working pressures, and considerable peak pressures associated with muscle contraction. The main drawback is that bandages composed of short-stretch bands must be changed frequently, since, pressure is quickly lost with reduced swelling.5
High-elasticity bandages (Long Stretch)The components of highly elastic bandages always contain elastane fibers, which enable the bandage to stretch to twice its original length. Given that these bandages adapt to the diameter of the leg, with no resistance to muscle contraction, there is little difference between resting and working pressure; therefore, they are less effective for reducing edema. Since they exert high pressure during resting, they are more poorly tolerated by patients, especially those with some degree of arterial disease.5
Multicomponent bandage systemsMulticomponent systems are formed by bandages of different characteristics, on which the greater or lesser stiffness of the bandage will depend. They may be composed of 2, 3, or 4 bandages, with fixing, compression, and padding functions. Many of these systems come with pressure indicators, thus enabling them to be applied easily by nonexpert personnel (Fig. 6). These bandages can be worn continuously for up to a week without having to be changed. The frequency of changing will depend on the control of the wound exudate and maintenance of appropriate placement and subsequent pressure of the bandage.5
Compression stockingsThe pressure exerted by compression stockings does not depend on the professional who places the bandage. In addition, this approach makes it easier to wear shoes and carry out other activities of daily living. Various fabrics and models have been marketed, although the stocking can be custom-made for patients whose measurements are outside the normal range. Depending on the type of mesh, stocking fabric is classed as circular-knit and flat-knit. The latter is stiffer and is mainly indicated in patients with phlebolymphedema.5
Compression stockings are classified according to the pressure exerted at B1. The most widely used type in Spain is the German type (Table 1).
Treatment of venous ulcer normally requires 2 overlapping stockings to reach the recommended pressure of 30-40 mmHg, thus making placement easier.
Various devices have been marketed to facilitate placement.5
Self-Adjusting compression systems with a Velcro closureSelf-adjusting systems include an adjustable compression device with low-elasticity fabric and Velcro closures. They are easily placed, thus enabling the patient to use the device him/herself and readjust the pressure as it gradually decreases (Fig. 7). Self-adjusting systems provide autonomy and better quality of life for patients who find it difficult to use a stocking or who do not have access to a health professional when the bandage must be changed. The stiffness achieved with these devices is very similar to that obtained with short-stretch bands, with the additional benefit that the pressure can be adjusted throughout the day.19
Intermittent pneumatic compressionIntermittent pneumatic compression devices are formed by air chambers that surround the leg and are connected to a system that produces gradual proximal to distal pressure alternating with pressure-free intervals. Its main interest lies in its use as an adjuvant to other compression systems in immobilized patients or situations in which other types of compression therapy cannot be used.20
Available EvidenceSeveral systematic reviews have analyzed the results of randomized controlled trials that compare the effect of compression therapy on venous ulcers with no compression, as well as the effect of the different compression therapy systems. The results of these reviews show that compression therapy is associated with faster healing than no compression.21–23 Comparison of the different types of compression therapy shows that multicomponent systems are associated with a more marked clinical benefit than monocomponent systems.21,22
As far as the different multilayer systems are concerned, 2-layer bandages have proven to be as effective as 4-layer bandages for treatment of venous ulcer, with the advantage that they are easier to apply.24
In the case of compression stockings for treatment and prevention of venous ulcers, the grade of recommendation is the same as that of bandages.25
Velcro-based systems seem to be a comfortable alternative that can prevent relapse, even though the available evidence on their efficacy is scarce.26
The effectiveness of compression therapy for prevention of venous ulcer is closely associated with strict adherence to treatment.27 Various studies support the use of compression therapy to avoid recurrence of venous ulcers, although studies on the most effective type of compression are clearly lacking.28 Recent clinical trials conclude that recurrence is less common with class III compression stockings.29 However, as previous studies have shown that patients who adhere to their compression therapy (irrespective of the class used) experience fewer recurrences, we should continue to recommend a grade of compression that is adjusted to the needs of the patient.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Conde Montero E, Serra Perrucho N, de la Cueva Dobao P. Principios teórico-prácticos de la terapia compresiva para el tratamiento y prevención de la úlcera venosa. Actas Dermosifiliogr. 2020;111:829–834.