The patient was a 90-year-old woman who had a personal history of severe hypoacusis and osteoporosis and was not receiving chronic treatment. She consulted for several asymptomatic lesions on her chest, shoulders, and upper back. The lesions had appeared suddenly 5 years earlier, had never been treated, and had been stable since first onset.
Physical ExaminationPhysical examination revealed multiple well-defined erythematous-violaceous telangiectatic macules ranging in diameter from 5mm to 4cm (Fig. 1). The lesions did not blanch with pressure and were negative for the Darier sign.
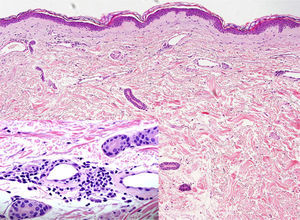
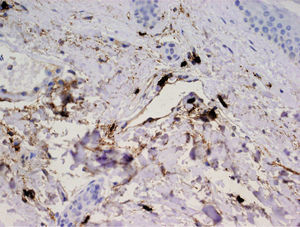
HistopathologyHistologic examination revealed dilated vascular structures in the superficial capillary plexus with peripheral inflammatory infiltrate characterized by a predominance of mast cells (Fig. 2). Staining showed the mast cells to be tryptase-positive (Fig. 3).
What Is Your Diagnosis?
DiagnosisTelangiectasia macularis eruptiva perstans (TMEP)
Clinical Course and TreatmentThe laboratory workup included a complete blood cell count, biochemistry, liver and kidney function tests, and a serum tryptase test. Serum tryptase was slightly elevated at 16.3μg/L (13.5μg/L being the upper limit of normal). Despite this finding, the patient and her family declined to continue with the exploration due to the patient's advanced age.
CommentMastocytosis comprises a group of diseases characterized by an excessive accumulation of mast cells in the skin, and occasionally in the tissue of other organs.
Three clinical variants of mastocytosis with cutaneous involvement have been described: urticaria pigmentosa (either its typical clinical manifestation of plaques and nodules or TMEP), diffuse cutaneous mastocytosis, and mastocytoma.
TMEP was first described by Weber in 1930.1 Thought to be a rare subtype of urticaria pigmentosa, it occurs in less than 1% of mastocytosis patients. TMEP occurs mainly in young and middle-aged adults, although cases of pediatric onset have been reported. A familial form of TMEP was described in 4 pediatric patients in 3 generations of a single family.2
It manifests clinically as erythematous macules comprising purplish or brownish asymptomatic telangiectasias that are negative for the Darier sign and located primarily on the trunk and upper limbs. Unilateral segmental manifestations of TMEP that may lead to a differential diagnosis with unilateral nevoid telangiectasia have also been reported.3
Histologically, TMEP is characterized by an increase in the relative number of mast cells distributed around dilated capillaries and venules in the superficial capillary plexus. In most cases of TMEP, the number of mast cells does not increase very much in absolute terms, making it difficult to diagnose the disease by means of hematoxylin–eosin staining. Therefore, immunohistochemical staining for tryptase and/or c-kit (CD 117) is recommended.4
Although TMEP has been considered to be a form of mastocytosis that only affects the skin, it can cause systemic symptoms, such as hypotension, flushing, pruritus, abdominal pain, and anaphylaxis due to the release of mediators by mast cells. In other cases, it can lead to symptoms caused by the infiltration of other organs, such as splenomegaly, adenopathy, hepatomegaly, and anemia. Finally, in isolated cases, this variant of mastocytosis has been associated with myeloproliferative, lymphoproliferative, and myelodysplastic syndromes.5
The choice of treatment depends on whether systemic or exclusively cutaneous involvement is detected. Cases involving only the skin have been treated satisfactorily with topical and intralesional corticosteroids, topical calcineurin inhibitors, 585nm vascular laser treatment, and psoralen-UV-A (PUVA) therapy.6
Conflicts of InterestThe authors declare that they have no conflicts of interest.
The authors would like to thank Jesús Cuevas Santos and Luis Cristian Perna Monroy for providing the histopathological images.
Please cite this article as: Martín-Fuentes A, et al. Lesiones maculares telangiectásicas en una mujer de 90 años. Actas Dermosifiliogr. 2012;103:65–6.