Sarcoidosis has been associated with various autoimmune processes, including primary biliary cirrhosis, autoimmune hepatitis, vitiligo, thyroiditis, and pernicious anemia,1 as well as connective tissue diseases such as Sjögren syndrome, polymyositis, systemic lupus erythematosus, and systemic sclerosis.2,3
We report the case of a 59-year-old woman who in 2002 presented with progressive dyspnea, weight loss, and anorexia that had begun 1 year earlier. The patient's medical history included asthma and hypertension. A plain chest radiograph and chest computed tomography scan revealed a reticulonodular interstitial pattern in the middle and upper lung fields accompanied by mediastinal lymphadenopathy, a clinical picture suggestive of sarcoidosis. Lung function testing showed a restrictive ventilation pattern (FVC, 44%; FEV1, 38%) and a carbon monoxide diffusing capacity of 38% (normal>80%).
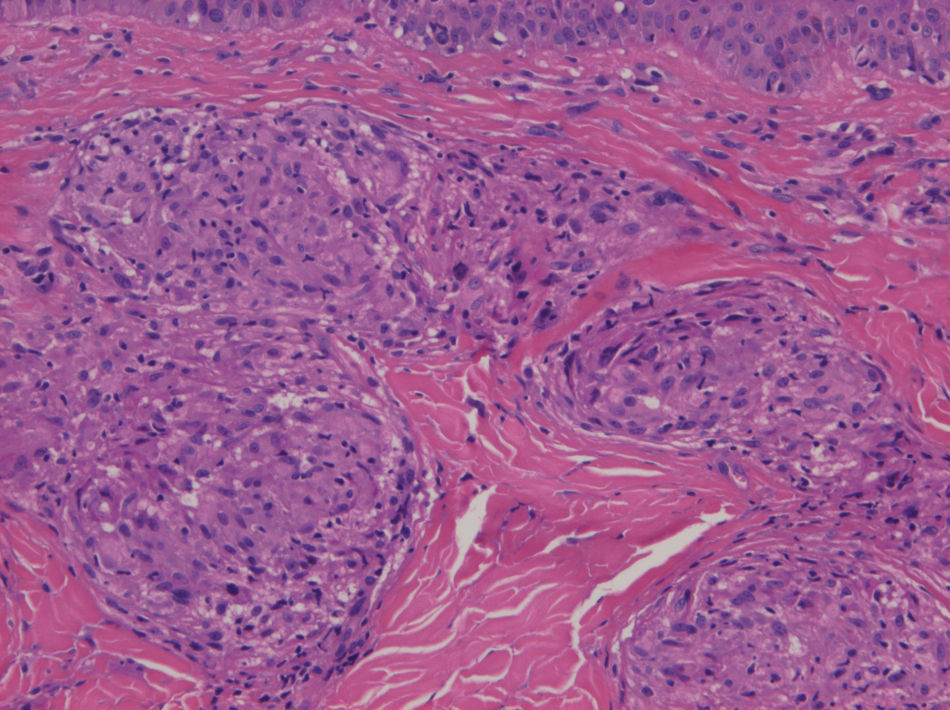
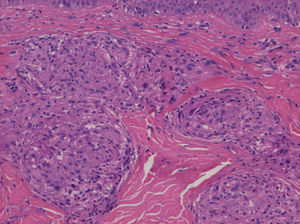
During the physical examination, erythematous-desquamative papules and plaques on the back and arms were observed (Fig. 1). Histology of these lesions detected noncaseating granulomas with scarce lymphocytes, a finding compatible with a diagnosis of sarcoidosis (Fig. 2). Blood tests showed increased levels of angiotensin-converting enzyme at 271.1 U/L (reference range 19-79 U/L) and aldolase 13.7 U/L (reference value<7 U/L). The patient tested positive for lupus anticoagulant and high-titer antinuclear antibodies (>1:320) including anticentromere antibodies.
The patient reported the symptoms of Raynaud phenomenon. A thorough physical examination revealed sclerodactyly with scarring on the fingertips and telangiectasis on the fingertips and lips (Fig. 3). During follow-up, a pruritic, erythematous-violaceous plaque was found on the right forearm; histologic testing of this lesion showed the presence of thickened collagen fibers in the dermis.
A plain radiograph of the hands and forearms demonstrated calcinosis. Esophageal manometry showed hypotonia in the middle and distal esophagus. Echocardiogram revealed diastolic dysfunction. No abnormalities were found in a biopsied muscle specimen.
The patient was diagnosed with sarcoidosis and CREST syndrome (calcinosis, Raynaud phenomenon, esophageal dysmotility, sclerodactyly, and telangiectasia), a type of systemic sclerosis. After treatment with prednisolone (60mg/d) and nifedipine (10mg/12h), the clinical and radiographic aspects of the skin and lung involvement related to sarcoidosis improved. Azathioprine (100mg/d) was later added to the regimen. The dose of prednisolone was tapered gradually and the drug was discontinued 1 year after start of treatment; treatment with azathioprine was maintained.
In 2004, the patient presented with an episode of anterior uveitis; in the same year she was admitted to hospital for pulmonary sarcoidosis progression. At that time, systemic corticosteroid treatment and oral colchicine were added to her treatment regimen. Systemic corticosteroid treatment was withdrawn in 2006, colchicine in 2008, and azathioprine in 2009. The patient is currently asymptomatic and receiving no treatment. The skin lesions associated with sarcoidosis have disappeared and her lung function test results are normal.
In our review of the literature we found 24 patients with systemic sclerosis and sarcoidosis.2–8 Fifteen of these patients were diagnosed with systemic sclerosis between 2 and 30 years prior to being diagnosed with sarcoidosis. In 6 patients both diseases appeared simultaneously, and in 3 sarcoidosis appeared before systemic sclerosis.
It is important to emphasize that it can be difficult to differentiate between these 2 diseases because the respiratory manifestations may be similar.4,6 Skin tests play a crucial role in the diagnosis of both processes. In our patient, histopathologic examination of the skin lesions confirmed sarcoidosis. We found only 1 case of cutaneous sarcoidal granulomas in the literature.8 In the present case, a thorough examination of the skin revealed systemic sclerosis (CREST syndrome). Whether concomitant sarcoidosis and autoimmune disease is a mere coincidence or the result of a common pathogenic mechanism has not been clearly established.3-6 Cox et al.3 and Takahashi et al.8 suggest that these 2 entities are probably the result of different pathogenic mechanisms because they do not appear simultaneously and the clinical course is different in each case. De Bandt et al.,4 however, suggest that a common etiology exists because most patients present with sarcoidosis and systemic sclerosis simultaneously.
Immunologic abnormalities found in patients with sarcoidosis include increased production of T cell derived cytokines (IL-2, IFN-γ) during the formation of granulomas, and an increase in macrophage-derived cytokines (IL-1, IL-6, IL-8, IL-15, tumor necrosis factor α, IFN-γ, and granulocyte-macrophage colony-stimulating factor), chemokines (macrophage inflammatory protein β and IL-16), and fibrogenic cytokines (transforming growth factor β, platelet-derived growth factor, and insulin-like growth factor 1) that induce fibrosis in patients with a persistent form of the disease.9 In systemic sclerosis, the cytokines implicated in the induction of fibrosis are transforming growth factor β and platelet-derived growth factor, the same cytokines implicated in persistent sarcoidosis.10
In conclusion, it is important to understand the processes involved in each of these two diseases and to take the appropriate action in patients with systemic sclerosis who develop sarcoid granulomas and in patients with sarcoidosis who develop sclerodermic lesions.
Please cite this article as: López-Ferrer A, et al. Esclerodermia sistémica asociada a sarcoidosis con afectación cutánea a propósito de un caso. Actas Dermosifiliogr.2012;103:337-8.