Cutaneous metastasis, a condition with variable clinical presentation, can be the first manifestation of internal malignancy, although it is rarely seen in hepatocellular carcinoma (HCC).1 In patients with HCC, the presence of cutaneous metastases is associated with a dismal prognosis, an increased likelihood of metastases at other sites, and a median survival of less than 5 months.2,3 This letter describes the case of a liver transplant recipient in whom multiple cutaneous metastases were the first sign of HCC recurrence.
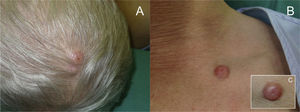
The patient was a 57-year-old man with a personal history of type 2 diabetes mellitus and liver transplant for treatment of alcoholic liver cirrhosis complicated by HCC. At the patient's regular post-transplant follow-up visits at the hepatology unit, good graft function was seen and there was no evidence of tumor recurrence. Seven months after transplant, the patient presented with rapidly growing asymptomatic lesions on the scalp and in the left supraclavicular region that had appeared several weeks earlier. Physical examination revealed 3 firm, erythematous-violaceous tumors with well-defined borders, measuring between 1 and 2cm in diameter, in the right temporal-parietal region of the scalp (Fig. 1A) and in the left supraclavicular region (Fig. 1B). Some of the tumors had a small central erosion and a pronounced vascular component (Fig. 1C).
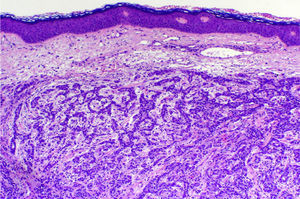
Histopathologic examination of the lesions revealed a proliferation of neoplastic cells in the dermis arranged in trabeculae, alveoli, and, in some places, pseudoglandular patterns (Fig. 2). The cells were cuboidal, with granular cytoplasm, hyperchromatic nuclei, and marked cellular pleomorphism. Several mitotic figures were also visible. The tumor cells were positively labeled with antibodies against cytokeratin AE1/AE3 and alpha-fetoprotein, and with the hepatocyte antibody. The morphologic and immunohistochemical findings were consistent with a diagnosis of cutaneous metastases of HCC.
Two weeks after histologic confirmation of the metastases, the patient presented to the emergency department with productive cough with whitish sputum and lower chest pain on both sides. The symptoms had appeared 3 days earlier. A chest radiograph showed a poorly defined radiopaque area in the basal region of the right lung field (Fig. 3A). In view of the patient's medical history, a computed tomography scan was performed, confirming the presence of a large mass measuring 4.3cm in the right lower lobe, and showing multiple pulmonary nodules and mediastinal lymph node involvement (Fig. 3B). Metastases were also observed in the liver, around the kidneys, and in a suprarenal gland (Fig. 3C), as well as in subcutaneous tissue and muscle tissue. One month later, the patient once again presented to the emergency department with disorientation and generalized tonic-clonic seizures. Brain magnetic resonance imaging revealed a prominent left choroid plexus and an irregularly shaped, high-uptake image consistent with a metastatic lesion (Fig. 3D). Following gradual deterioration in general health, the patient died just 6 weeks after the diagnosis of cutaneous metastases.
A, Anteroposterior chest radiograph showing a poorly defined radiopaque area in the basal region of the right lung field. B, Thoracic computed tomography scan showing a large mass measuring 4.3cm in the right lower lobe and multiple smaller pulmonary nodules. C, Abdominal computed tomography scan showing intrahepatic, perirenal, and right suprarenal metastases. D, Brain magnetic resonance imaging showing a prominent left choroid plexus and an irregularly shaped, high-uptake image consistent with a metastatic lesion.
HCC is the most common primary malignant tumor of the liver, and its incidence has increased in recent years. However, cutaneous metastases of HCC are very rare, accounting for 0.2% to 2.7% of all cutaneous metastases.4 These metastases are of interest in part because they can be the first manifestation of the primary tumor5 or, as in our case, the first sign of disease recurrence.
Cutaneous metastasis of HCC occurs most frequently in men over 50 years of age, usually in the sixth decade of life,1 and usually manifests as a single painless, fast-growing lesion. The most common location is the head (usually the face), followed by the chest, the abdomen, and the limbs. The lesions can take a variety of clinical forms but are usually firm, bluish-red or purple, 1 to 5cm in diameter, and nonulcerated.1,4–6 They may also be necrotic or purulent or resemble pyogenic granulomas.7
Three different mechanisms8 by which a liver tumor can produce cutaneous metastases have been described: continuous growth from the liver parenchyma, systemic spread of disease, and tumor implantation or seeding following manipulation of the lesion using various diagnostic or therapeutic methods.
Histopathologic diagnosis is possible when a hepatocellular component—bile production in part of the tumor, intercellular bile canaliculi, or a trabecular growth pattern—is present.1 From an immunohistochemical perspective, the hepatocyte antibody has proved to be very helpful in the diagnosis of poorly differentiated tumors.8
The presence of cutaneous metastases of HCC is associated with a very poor prognosis, an increased likelihood of metastases at other sites, and a median survival of less than 5 months.2,3 This case highlights the fact that a dermatologist may be the first specialist to detect the recurrence of an internal malignancy when metastases have not reached sites other than the skin or have not manifested clinically.
Please cite this article as: Alonso-González J, et al. Metástasis cutáneas múltiples de carcinoma hepatocelular como primer signo de recidiva tumoral en paciente transplantado. Actas Dermosifiliogr. 2012;103:339-41.