Small-cell neuroendocrine carcinoma (SCNC) in the sinonasal region is a relatively rare, aggressive tumor with a high rate of recurrence and metastasis. It was first described in 1965 by Raychowdhuri1 and approximately 50 cases have been published since that time. The majority of SCNCs affect the lungs and only around 4% are located at other sites.2
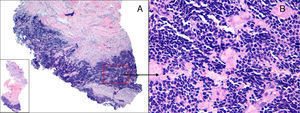
We present the case of a 32-year-old woman with no past history of interest. She consulted for progressively increasing pain and inflammation on the dorsum of the nose that had started 2 months earlier. Physical examination revealed a solid, fixed nodule with a smooth surface on the right lateral surface of the dorsum of the nose. The nodule measured approximately 3cm in its longest diameter (Figure 1); in addition, there was a palpable right jugulodigastric lymph node. Magnetic resonance imaging of the paranasal sinuses revealed a nodular lesion of the external nose that eroded the right nasal bones. On skin biopsy, a diffuse infiltration of neoplastic cells was observed in the deep dermis, hypodermis, and muscle layer. The cells were small and round, with scant cytoplasm and basophilic nuclei (Figure 2A andB). Immunohistochemistry (Figure 3) showed a phenotypic profile positive for neuroendocrine (chromogranin A and CD56) and epithelial (cytokeratin AE1/AE3) markers and for thyroid transcription factor1 (TTF-1) and negative for cytokeratin20 (CK20), cytokeratin7 (CK7), protein S-100, glial fibrillary acidic protein (GFAP), neurofilaments, and Epstein Barr virus (EBV) antigen. The cervical lymph node was biopsied and the histologic and immunohistochemical findings were consistent with SCNC arising from the seromucous glands of the sinonasal region. Study of tumor spread by cervical-thoracic-abdominopelvic computed tomography (CT) revealed multiple proliferative malignant implants in the liver. The case was discussed in the tumor committee and, in view of the presence of disseminated disease, salvage surgical treatment of the primary tumor was excluded and it was decided to start chemotherapy with cisplatin and etoposide, combined with radiation therapy. Six months after the diagnosis of the carcinoma, after 8 cycles of chemotherapy, the patient died of liver failure secondary to metastatic infiltration by the tumor.
A, A 5-mm biopsy of the nasal nodule. A diffuse proliferation of neoplastic cells is visible in the deep dermis, hypodermis, and muscle layer. Hematoxylin and eosin, original magnification×10. B, The neoplastic cells are small, round, and monomorphic, with scant cytoplasm and basophilic nuclei. Hematoxylin and eosin, original magnification×400.
SCNC of the sinonasal region arises from the APUD cells of the neuroendocrine system that are occasionally present in the seromucous glands of the nasal cavity and in the accessory salivary glands.3 These tumors affect men and women equally, and the mean age at onset is 50 years. No risk factors have been identified, nor is there evidence to suggest that the presence of EBV is related to the pathogenesis of this tumor; infection by this virus has been well documented in other types of sinonasal carcinoma.4
Histopathology study using hematoxylin and eosin (H&E) stain reveals a diffuse infiltration of neoplastic cells that mainly affects the dermis and that is formed of small cells with scant cytoplasm and large, densely hyperchromatic nuclei; mitotic figures and areas of necrosis can be seen.
Immunohistochemistry, though nonspecific, is the most useful diagnostic tool and is based on positivity for markers of epithelial differentiation (CK, AE1/AE3, and CAM 5.2) and neuroendocrine differentiation (chromogranin A, synaptophysin, and/or neuron-specific enolase [NSE]. Immunohistochemistry is negative for protein S-100 and neurofilaments, which helps to exclude other diseases that can have a similar appearance with H&E stain, such as small cell melanoma and stesioneuroblastoma.4
The diagnostic challenge, because of the similar clinical and histological characteristics, arises with 2 diseases: Merkel cell carcinoma, which is usually CK20-positive5 and TTF-1–negative6; and skin metastases of small-cell lung cancer,7 whose cells stain positive for CK7 and TTF-1. In the case of SCNC of the sinonasal region, CK7 and CK20 are negative and, if the cells are positive for TTF-1, imaging studies must be performed to confirm the absence of lung disease. In our patient, we confirmed the absence of a lung tumor by CT, which was performed as part of the workup for tumor spread.
Although there is little experience in the management of this type of tumor, neoadjuvant cytoreductive chemotherapy with cisplatin and etoposide is considered to be the treatment of choice.8 Other authors recommend wide excision of the lesion as the initial treatment, associated with radiation therapy and chemotherapy,9 as long as metastatic disease has been excluded at the time of diagnosis.
Metastases usually affect the brain, lung, and skeleton. Mean survival after diagnosis is between 2 and 3 years, and the most unfavorable prognostic factors are locoregional invasion and associated paraneoplastic endocrine syndromes.10
It is important for dermatologists to be aware of the existence, characteristics, and clinical course of SCNC of the sinonasal region in order to differentiate it from other neuroendocrine tumors that can be clinically and histologically indistinguishable, such as Merkel cell tumor.
Please cite this article as: Rivas-Tolosa N, Llombart B, Traves V, Guillén C. Carcinoma neuroendocrino de células pequeñas de la región nasosinusal no carcinoma de células de Merkel: presentación de un caso. Actas Dermosifiliogr. 2015;106:143–145.