Cutaneous lymphomas are a neoplastic abnormality of the skin that present in 4% of all lymphomas. Eighty percent of cutaneous lymphomas originate in T lymphocytes and, of these, half are mycosis fungoides. The incidence of this disease has been calculated at 0.4 cases per 100,000 inhabitants per year and it mainly presents in older adults, with an average age of 60 years. Approximately 70% of patients are white and the disease occurs more frequently in men than in women. Follicular or folliculotropic mycosis fungoides is a rare variant of this type of T-cell cutaneous lymphoma.
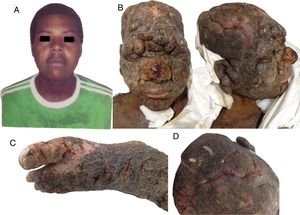
A 28-year-old man born on the Pacific coast of Colombia, who was a member of an outlawed armed group living in the jungle, visited the emergency department with skin lesions that had appeared 4 years earlier and which had become generalized. The patient had no prior diagnosis and had not received any treatment. Physical examination revealed multiple coalescing hyperkeratotic infiltrated tumorous lesions on the face, scalp, torso, back, arms, and legs. The patient presented facies leonina on the face, with loss of adnexa, madarosis, and loss of eyelashes and body hair. The scalp showed suppurating cerebriform lesions. No involvement of the oral or genital mucosa was observed. Palpation revealed no enlarged lymph nodes or organs (Fig. 1). Empirical treatment with ampicillin–sulbactam and vancomycin was instated, skin biopsies were taken, and an analysis of disease extension was performed. The patient died from cardiorespiratory failure due to sepsis and multiorgan failure. The skin biopsies were reviewed post mortem by the dermatology department and revealed findings suggestive of folliculotropic mycosis fungoides; this finding was also supported by immune-staining tests (Fig. 2). Owing to the suspected diagnosis, a molecular study was performed of the tissue embedded in paraffin; the study confirmed clonal rearrangement of the T-cell receptor gamma (TCRG) chain. These findings support the diagnosis of a lymphoid tumor (Fig. 3). Tests for infection with human immunodeficiency virus, syphilis, and Leishmania were negative. Leprosy was ruled out by serologic studies and lymph node aspirates. Cultures for deep mycoses and mycobacteria were also negative. Computed tomography of the chest and abdomen revealed no abnormalities. The study of the bone-marrow sample was normal.
Clinical images of the patient: A, Image of the patient at 24 years of age, 4 years before the consultation. B, Photographs at the time of consultation, showing tumoral lesions on the face and scalp, associated with facies leonina. C, Severe involvement of the left foot. D, Involvement of the scalp with purulent exudate.
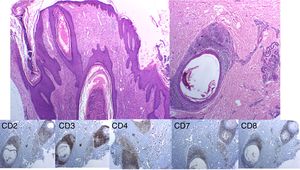
Histopathology images. Immune staining with hematoxylin–eosin shows a hyperplasic perifollicular epidermis with infiltration of the follicular epithelium by numerous lymphocytes, some of which are atypical. Immune staining and immunophenotyping of these lymphocytes shows CD3+, with partial loss of CD2 and CD7, and a CD4:CD8 ratio of 4:1.
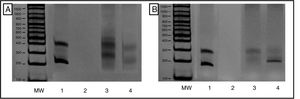
Evaluation of T-cell receptor gamma chain rearrangement using multiplex polymerase chain reaction (PCR). Results viewed in 6% polyacrylamide gel, in accordance with BIOMED-2 protocols. A, T Vγ1-8 and Vγ10 receptor cells. B, TCR Vγ9 and Vγ1. MW indicates molecular weight marker; 1, InVivoScribe «0021» positive control; 2, PCR mix and molecular biology grade water instead of DNA; 3, polyclonal control (pool of lymphocytes from healthy patients); and 4, Patient sample showing monoclonal product of approximately 200 nucleotides from the T-cell receptor regions Vγ9 and Vγ11.
Follicular or folliculotropic mycosis fungoides is a rare variant of this type of T-cell cutaneous lymphoma, which affects the hair follicles and generally does not affect the epidermis.1 The World Health Organization and the European Organization for Research and Treatment of Cancer (WHO-EORTC) consider it to be a variant of mycosis fungoides.2 Folliculotropic mycosis fungoides affects the head and neck in 85% of cases, in the form of pruritic follicular papules, acneiform lesions, or cysts, associated with alopecia, and often with involvement of the eyebrows.3 The lesions tend to be local and generalized forms are extremely rare.4 The manifestation of facies leonina has been described in folliculotropic mycosis fungoides, although it is rare; a 2015 systematic review found only 24 patients with this association.5 Ishibashi et al. reported the case of a patient who also had a severe presentation of this disease with facies leonina, images of which are very similar to the patient described by us.6 The folliculotropic variant tends to be more aggressive than the plaque phase in mycosis fungoides and the mortality rate is similar to that of the tumoral phase.7 Folliculotropic mycosis fungoides is also more refractory. Molecular clonality testing can be of considerable help in determining the diagnosis in cases such as this, where diagnosis is difficult. The test can be performed on samples of skin, lymph node, bone marrow, or peripheral blood.8 Detection of one or more clones does not necessarily indicate neoplasia and the test results should therefore be assessed together with the clinical, histologic, and immunophenotyping findings.9
In conclusion, we report the case of a patient with folliculotropic mycosis fungoides confirmed by means of skin biopsy, immune staining, and molecular biology study, with severe and generalized presentation involving more than 90% of the body surface and associated with facies leonina. The skin disease led to a bacterial superinfection, which is frequently reported with this entity, followed by sepsis and death of the patient. This case is perhaps one of the most severe and aggressive forms of the disease reported to date.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
The authors would like to thank Dr Ana Cristina Ruiz and Dr Natalia Olaya for their contributions to the case.
Please cite this article as: Uribe-Bojanini E, Santa-Vélez C, Rueda-Cadena X, Morales SD. Micosis fungoide foliculotropa de presentación grave y letal. Actas Dermosifiliogr. 2019;110:412–414.