Immunoglobulin (Ig) 4–related disease is a clinical and patholological entity with a broad spectrum of clinical manifestations.1 Recognized as a systemic disease in 20032 after the description of patients with special forms of autoimmune pancreatitis, IgG4-related disease is associated with various extrapancreatic manifestations, with the skin being one of the organs affected. The course of the disease has yet to be suitably characterized. In 2015, Yélamos3 made a preliminary appraisal of the dermatologic aspects of the disease. What has changed since then?
In epidemiological terms, IgG4-related disease seems to be more common in elderly men, with a mean age of 61.4 (13.4) years and a sex ratio of 4:1 (men:women).4,5 Based on histopathology findings, the prevalence of IgG4-related disease in Japan is estimated to be 2.63-10.2 cases per million inhabitants, with an incidence of 336-1300 new cases per year.4
Clinically, the disease presents with a subacute course, and most patients have asthenia or weight loss. In addition, affected patients usually have allergic rhinitis, bronchial asthma, or atopic dermatitis; therefore, the dermatologist plays a particularly relevant role.
When diagnosing and monitoring the disease, we must highlight 3 points6:
- a
No specific diagnostic antibodies have been identified.
- b
IgG4 levels can help in the initial diagnosis but not to monitor the disease. There is a correlation with serum IgG4 levels and the number of organs involved.
- c
Plasmablast level (CD19+, CD20–, CD27+, CD38+) (>2000/mL) is a useful biomarker of activity, although it is not widely used or available in most hospitals.
Irrespective of the criteria set, histopathology is characterized by 2 findings that are extraordinary and practically rule out IgG4-related disease: the presence of granulomas and the presence of a neutrophilic infiltrate.7 Imaging tests are very useful for identifying possible locations for biopsy specimens, and positron emission tomography/computed tomography with fluorodeoxyglucose is the most appropriate, since it evaluates the extension of the disease (uptake is particularly marked in the salivary glands and lymph nodes and in vascular invasion) and the response to immunosuppressive treatment.
Have there been advances in our knowledge of skin disease?
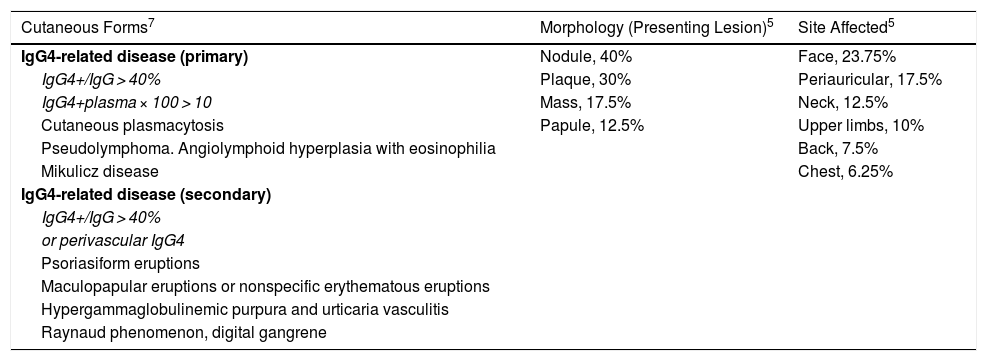
Based on a literature review and their own experience, Tokura et al.8 reported various patterns of cutaneous expression. Table 1 shows the primary and secondary forms of skin involvement, the main morphologies of the lesions, and the site affected according to data from the systematic review of Bennet et al.5
Cutaneous Expression of IgG4-Related Disease.
| Cutaneous Forms7 | Morphology (Presenting Lesion)5 | Site Affected5 |
|---|---|---|
| IgG4-related disease (primary) | Nodule, 40% | Face, 23.75% |
| IgG4+/IgG > 40% | Plaque, 30% | Periauricular, 17.5% |
| IgG4+plasma × 100 > 10 | Mass, 17.5% | Neck, 12.5% |
| Cutaneous plasmacytosis | Papule, 12.5% | Upper limbs, 10% |
| Pseudolymphoma. Angiolymphoid hyperplasia with eosinophilia | Back, 7.5% | |
| Mikulicz disease | Chest, 6.25% | |
| IgG4-related disease (secondary) | ||
| IgG4+/IgG > 40% | ||
| or perivascular IgG4 | ||
| Psoriasiform eruptions | ||
| Maculopapular eruptions or nonspecific erythematous eruptions | ||
| Hypergammaglobulinemic purpura and urticaria vasculitis | ||
| Raynaud phenomenon, digital gangrene |
The first data from the Spanish registry of IgG4-related disease were published in 2015. As the prevalence of the disease is low,9 the data retrieved can help us to better characterize it. Salivary gland involvement affects 16% and is closely related to skin involvement. Therefore, given the clinical suspicion and ease of access, skin biopsy can be complemented by salivary gland biopsy to provide the dermatologist with information on the disease, bearing in mind that obliterative fibrosis need not always be present, in contrast with other organs.
Treatment should be tailored to the characteristics of the patient. Of note, not all manifestations of IgG4-related disease require treatment, although close multidisciplinary follow-up is necessary. Rituximab, systemic corticosteroids, and azathioprine are the main drugs used for treatment of the disease.6
Please cite this article as: Ródenas-Herranz T, Linares-Gonzalez L, Ruiz-Villaverde R. FR-Enfermedad relacionada con IgG4, 4 años después. Actas Dermosifiliogr. 2021;112:461–462.