The skin is a fundamental organ in the transition from intrauterine to extrauterine life. The newborn infant experiences physiological changes and often presents benign, transient skin characteristics that vary according to maternal, gestational, and neonatal factors.
ObjectivesTo estimate the frequency of various dermatologic findings during the first 72 hours of life and to identify their association with maternal, gestational, or neonatal factors.
MethodsDescriptive, observational, cross-sectional study from April to July 2015 and July to November 2017 in the maternity ward of Centro Hospitalario Pereira Rossell. We examined the skin of neonates within 72 hours of birth. Proportions and 95% CIs were calculated for all findings. Associations between findings and factors were analyzed.
ResultsA total of 2811 neonates were included. We observed at least 1 neonatal skin finding in all of the neonates and found a median (interquartile range) of 8 (6–9) findings (minimum–maximum, 1–16). We observed 42 of the 46 possible characteristics we looked for; 99.9% of the findings were benign and transient. Among the findings were lanugo (98%; 95% CI, 97.7%–98.7%), physiological scaling (79.7%; 95% CI, 78.2%–81.1%), and sebaceous hyperplasia (73.3%; 95% CI, 71.6%–74.9%). Lanugo (P = .001), physiological scaling (P < .001), and erythema toxicum (P = .001) were observed significantly more often in full- and late-term neonates. Sebaceous hyperplasia (P = .001) and transient hyperpigmentation (P < .001) were found more often in newborn males. Erythema toxicum was more common after vaginal births (P = .008). Transient hyperpigmentation (P < .001) and dermal melanocytosis (P < .001) were seen more often in neonates of African descent.
ConclusionsAll neonates have skin characteristics that are part of their adaptation to extrauterine life. Most are benign and transient. Maternal age, type of delivery, and certain neonatal factors such as gestational age, birth weight, sex, and ethnicity are associated with specific findings.
La piel es fundamental en la transición de la vida intrauterina a la extrauterina. El recién nacido presenta cambios fisiológicos, siendo frecuente observar hallazgos cutáneos benignos y transitorios que varían según las características maternas, neonatales y de la gestación.
ObjetivosEstimar la frecuencia de diferentes hallazgos dermatológicos en neonatos en las primeras 72 horas de vida e identificar la existencia de diferencias de proporciones estadísticamente significativas con factores neonatales, maternos y de la gestación.
MétodosSe realizó un estudio descriptivo, observacional de corte transversal entre abril a julio 2015 y de julio a noviembre de 2017 en la maternidad del Centro Hospitalario Pereira Rossell. Se incluyeron neonatos de hasta 72 horas de vida, a los que se les practicó un examen dermatológico completo. Se presenta la proporción de cada uno de los hallazgos con el intervalo de confianza correspondiente. Se analiza la relación entre los hallazgos y determinados factores asociados.
ResultadosSe incluyeron 2811 neonatos. El 100% presentó al menos 1 hallazgo a nivel de la piel. La mediana fue de 8 lesiones por paciente (IIQ. 6 -9/Mn-Mx: 1-16). De los 46 hallazgos explorados clínicamente se encontraron 42. Las lesiones benignas y transitorias correspondieron a 99,9%. Entre ellas se observó: lanugo 98% (IC 97,7-98,7), descamación fisiológica 79,7% (IC 78,2-81,1) e hiperplasia sebácea 73,3% (IC 71,6-74,9). El lanugo (p = 0,001), la descamación fisiológica (p < 0,001), el eritema tóxico neonatal (p 0,001) se observaron con más frecuencia en los neonatos de término y postérmino. La hiperplasia sebácea (p = 0,001) y la hiperpigmentación transitoria neonatal (p < 0,001) se encontraron con mayor frecuencia en varones. El eritema tóxico neonatal aumentó en los nacimientos por parto vaginal (p 0,008). La hiperpigmentación neonatal transitoria (p < 0,001) y la melanocitosis dérmica (p < 0,001) se observaron en mayor proporción en afrodescendientes.
ConclusionesEl 100% de los neonatos presenta cambios a nivel de la piel, la mayoría benignos y transitorios como parte de la adaptación a la vida extrauterina. La edad materna, la vía de nacimiento, las características del neonato como la edad gestacional, el peso al nacer, el sexo, así como la etnia se asocian con la aparición de hallazgos específicos.
The skin plays a fundamental role during the transition between life inside and outside the womb. Skin anomalies at birth are common, but most are transient and benign, occurring as physiological responses to birth and limited to the first days or weeks of life.1,2 They are normally diagnosed clinically, but the signs vary according to ethnic, neonatal, maternal, and gestational factors as well as mode of delivery and culture. International studies have looked at the prevalence of various neonatal skin findings,3–11 but no work has been published on skin conditions of neonates in Uruguay.
The Centro Hospitalario Pereira Rossell is a university referral hospital for all of Uruguay. The hospital attends approximately 7000 births every year.12 Our aims were to describe the skin conditions we see in this center, report their frequency, and analyze significant associations between the findings and maternal, obstetric, and neonatal characteristics.
Material and MethodsThis descriptive observational cross-sectional study was carried out by the pediatric neonatology and dermatology departments of the center. It was approved by the hospital’s research ethics committee.
The sample size was calculated based on the annual number of births in the hospital and the following assumptions: analysis of findings with a minimum frequency of 3%, a 95% CI, and a design effect of 0.01 (1%). The sample size calculated to provide a level of precision of 0.5% was 2729 neonates.
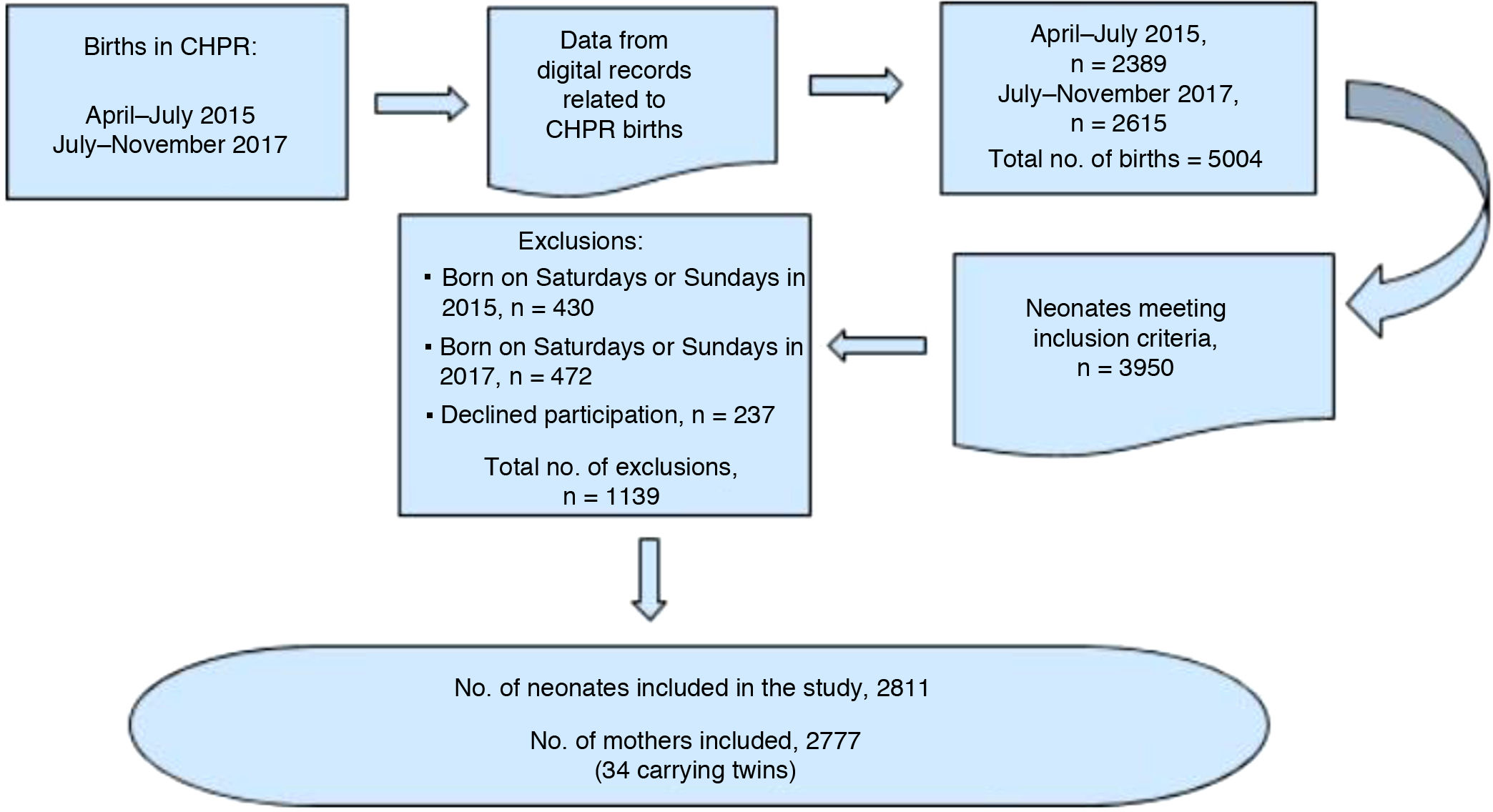
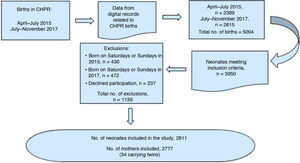
The neonates were recruited and examined consecutively Monday through Friday in the postnatal maternity ward within 72 hours of birth from April to July 2015 and July to November 2017. We excluded any neonates born on Saturday or Sunday or for whom consent to participate was not given (Fig. 1).
After the mothers gave their informed consent, a pediatric dermatologist and a neonatologist performed the dermatologic examination together. These specialists, trained to diagnose neonatal dermatoses, examined the skin, hair, nails, and mucosal surfaces to reach a clinical diagnosis. In case of doubt, they consulted a group of experts in the hospital’s pediatric dermatology department. A standardized form was used to collect data, including the perinatal history (maternal, obstetric, and neonatal information) stored in the computerized patient file kept by attending staff. Additional information was obtained by questioning the parents.
We looked for 46 dermatologic conditions grouped in 6 categories based on Harper’s classification of pediatric skin disorders2 and the 2018 nomenclature of the International Society for the Study of Vascular Anomalies.13 The examiners also noted the location, size, and number of lesions for some conditions on the list. The categories were as follows:
- 1)
Benign or transient findings: lanugo, physiological scaling, sebaceous hyperplasia, vernix caseosa, milium cysts, Epstein pearls, alveolar (Bohn) nodules or cysts, gland cysts, median raphe cysts, erythema toxicum neonatorum (ETN), transient neonatal pustular melanosis, miliaria crystallina or rubra, acral cyanosis, cutis marmorata, jaundice, rubor, sucking blister, pallor, teeth, neonatal acne, and harlequin coloring.
- 2)
Pigmented lesions: transient neonatal hyperpigmentation, congenital melanocytic nevus, café au lait macule, and dermal melanocytosis.
- 3)
Traumatic lesions: ecchymotic mask, serous/blood-filled sac, cephalohematoma, erosions, cuts, ecchymosis, and petechiae.
- 4)
Developmental abnormalities: affecting ears, digits, genitalia, the lips and/or mouth, or the sacral region; supernumerary nipples; hypospadias; and cutis aplasia.
- 5)
Epidermal nevi: sebaceous nevus.
- 6)
Vascular lesions: congenital hemangiomas, hemangioma precursors, capillary malformations (salmon patches), port wine stains, and arteriovenous anomalies.
We examined the associations between 7 variables mentioned in the literature1–11 and lesions with a prevalence of at least 5%. The first 2 variables were as follows:
- 1)
Maternal age according to the ranges specified by the American College of Obstetricians and Gynecologists, as follows: a) ≤18 years (adolescent mother), b) 19 to 34 years (ideal reproductive age range), and c) 35 years or older (older mother).
- 2)
Delivery mode: vaginal birth, cesarean section.
The remaining 5 variables were neonatal characteristics, as follows: sex, ethnicity, postnatal age in days, gestational age, and weight. Gestational age and weight were classified as suggested by the World Health Organization as follows: preterm (less than 37 weeks), term (between 37 and 41 weeks and 6 days), and postterm (42 weeks or more). Low birth weight was defined as less than 2500 g, normal weight as 2500 to 4000 g, and fetal macrosomia as a birth weight over 4000 g.
The normal distribution of continuous variables was assessed graphically and with the Shapiro–Wilk test. When the distribution was normal, results were expressed as mean (SD). Nonnormally distributed results were expressed as median, interquartile range (IQR), and the maximum–minimum range.
Categorical variables were described by raw frequencies and proportions (percentages) and their respective 95% CIs.
We assessed the association between findings and the categorical variables with the Pearson or Fisher tests. A P value less than .05 was considered statistically significant.
Data were processed with SPSS software, version 15.0.
ResultsNeonatal CharacteristicsA total of 2811 neonates entered the study, 1300 in the first period and 1511 in the second. Thirty-four were twins. The proportion of infants no more than 1 day old at the time of examination was 78.2%. Regarding sex, 50.9% were male and 49.1% were female. The mean gestational age at birth was 38.8 (1.33) weeks, and 95.2% were born at full term. The mean birth weight was 3252 (427) g; 90.2% of the infants weighed within the normal range.
Eighty-six percent of the infants were White, and 12.8% were mixed-race.
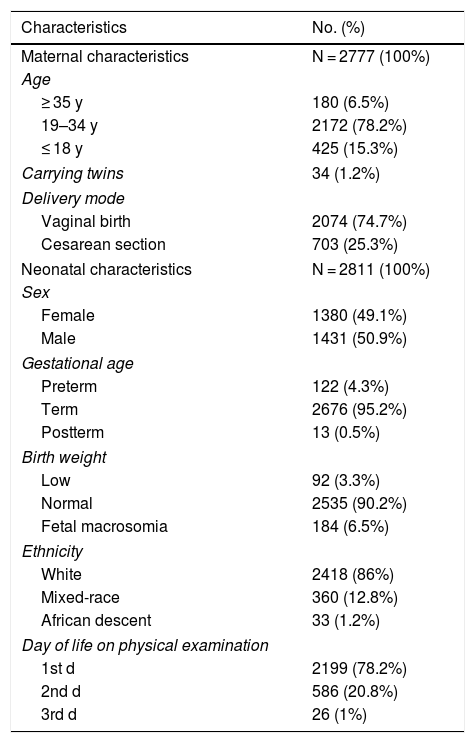
Maternal CharacteristicsThe median age of the 2777 mothers was 23 (IQR, 20–28; range, 13–48) years. Most infants (74.7%) were delivered vaginally (Table 1).
Characteristics of the Mothers and Newborn Infants in Centro Hospitalario Pereira Rossell Enrolled in the Study
| Characteristics | No. (%) |
|---|---|
| Maternal characteristics | N = 2777 (100%) |
| Age | |
| ≥ 35 y | 180 (6.5%) |
| 19–34 y | 2172 (78.2%) |
| ≤ 18 y | 425 (15.3%) |
| Carrying twins | 34 (1.2%) |
| Delivery mode | |
| Vaginal birth | 2074 (74.7%) |
| Cesarean section | 703 (25.3%) |
| Neonatal characteristics | N = 2811 (100%) |
| Sex | |
| Female | 1380 (49.1%) |
| Male | 1431 (50.9%) |
| Gestational age | |
| Preterm | 122 (4.3%) |
| Term | 2676 (95.2%) |
| Postterm | 13 (0.5%) |
| Birth weight | |
| Low | 92 (3.3%) |
| Normal | 2535 (90.2%) |
| Fetal macrosomia | 184 (6.5%) |
| Ethnicity | |
| White | 2418 (86%) |
| Mixed-race | 360 (12.8%) |
| African descent | 33 (1.2%) |
| Day of life on physical examination | |
| 1st d | 2199 (78.2%) |
| 2nd d | 586 (20.8%) |
| 3rd d | 26 (1%) |
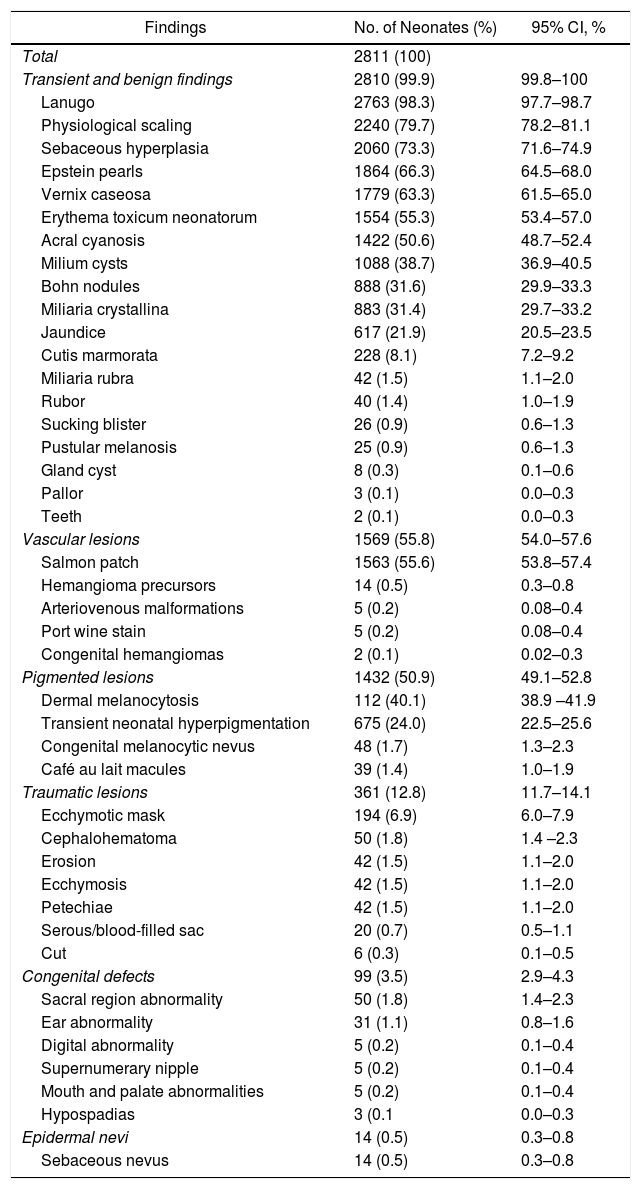
Table 2 shows the skin conditions observed. Forty-two of the 46 findings anticipated were found.
Dermatologic Findings in 2811 Neonates According to Category
| Findings | No. of Neonates (%) | 95% CI, % |
|---|---|---|
| Total | 2811 (100) | |
| Transient and benign findings | 2810 (99.9) | 99.8–100 |
| Lanugo | 2763 (98.3) | 97.7–98.7 |
| Physiological scaling | 2240 (79.7) | 78.2–81.1 |
| Sebaceous hyperplasia | 2060 (73.3) | 71.6–74.9 |
| Epstein pearls | 1864 (66.3) | 64.5–68.0 |
| Vernix caseosa | 1779 (63.3) | 61.5–65.0 |
| Erythema toxicum neonatorum | 1554 (55.3) | 53.4–57.0 |
| Acral cyanosis | 1422 (50.6) | 48.7–52.4 |
| Milium cysts | 1088 (38.7) | 36.9–40.5 |
| Bohn nodules | 888 (31.6) | 29.9–33.3 |
| Miliaria crystallina | 883 (31.4) | 29.7–33.2 |
| Jaundice | 617 (21.9) | 20.5–23.5 |
| Cutis marmorata | 228 (8.1) | 7.2–9.2 |
| Miliaria rubra | 42 (1.5) | 1.1–2.0 |
| Rubor | 40 (1.4) | 1.0–1.9 |
| Sucking blister | 26 (0.9) | 0.6–1.3 |
| Pustular melanosis | 25 (0.9) | 0.6–1.3 |
| Gland cyst | 8 (0.3) | 0.1–0.6 |
| Pallor | 3 (0.1) | 0.0–0.3 |
| Teeth | 2 (0.1) | 0.0–0.3 |
| Vascular lesions | 1569 (55.8) | 54.0–57.6 |
| Salmon patch | 1563 (55.6) | 53.8–57.4 |
| Hemangioma precursors | 14 (0.5) | 0.3–0.8 |
| Arteriovenous malformations | 5 (0.2) | 0.08–0.4 |
| Port wine stain | 5 (0.2) | 0.08–0.4 |
| Congenital hemangiomas | 2 (0.1) | 0.02–0.3 |
| Pigmented lesions | 1432 (50.9) | 49.1–52.8 |
| Dermal melanocytosis | 112 (40.1) | 38.9 –41.9 |
| Transient neonatal hyperpigmentation | 675 (24.0) | 22.5–25.6 |
| Congenital melanocytic nevus | 48 (1.7) | 1.3–2.3 |
| Café au lait macules | 39 (1.4) | 1.0–1.9 |
| Traumatic lesions | 361 (12.8) | 11.7–14.1 |
| Ecchymotic mask | 194 (6.9) | 6.0–7.9 |
| Cephalohematoma | 50 (1.8) | 1.4 –2.3 |
| Erosion | 42 (1.5) | 1.1–2.0 |
| Ecchymosis | 42 (1.5) | 1.1–2.0 |
| Petechiae | 42 (1.5) | 1.1–2.0 |
| Serous/blood-filled sac | 20 (0.7) | 0.5–1.1 |
| Cut | 6 (0.3) | 0.1–0.5 |
| Congenital defects | 99 (3.5) | 2.9–4.3 |
| Sacral region abnormality | 50 (1.8) | 1.4–2.3 |
| Ear abnormality | 31 (1.1) | 0.8–1.6 |
| Digital abnormality | 5 (0.2) | 0.1–0.4 |
| Supernumerary nipple | 5 (0.2) | 0.1–0.4 |
| Mouth and palate abnormalities | 5 (0.2) | 0.1–0.4 |
| Hypospadias | 3 (0.1 | 0.0–0.3 |
| Epidermal nevi | 14 (0.5) | 0.3–0.8 |
| Sebaceous nevus | 14 (0.5) | 0.3–0.8 |
All of the neonates presented at least 1 condition on examination. In 2795 (99.8%) more than a single type of finding was present. The median number was 8 per neonate (IQR, 6–9; range, 1–16).
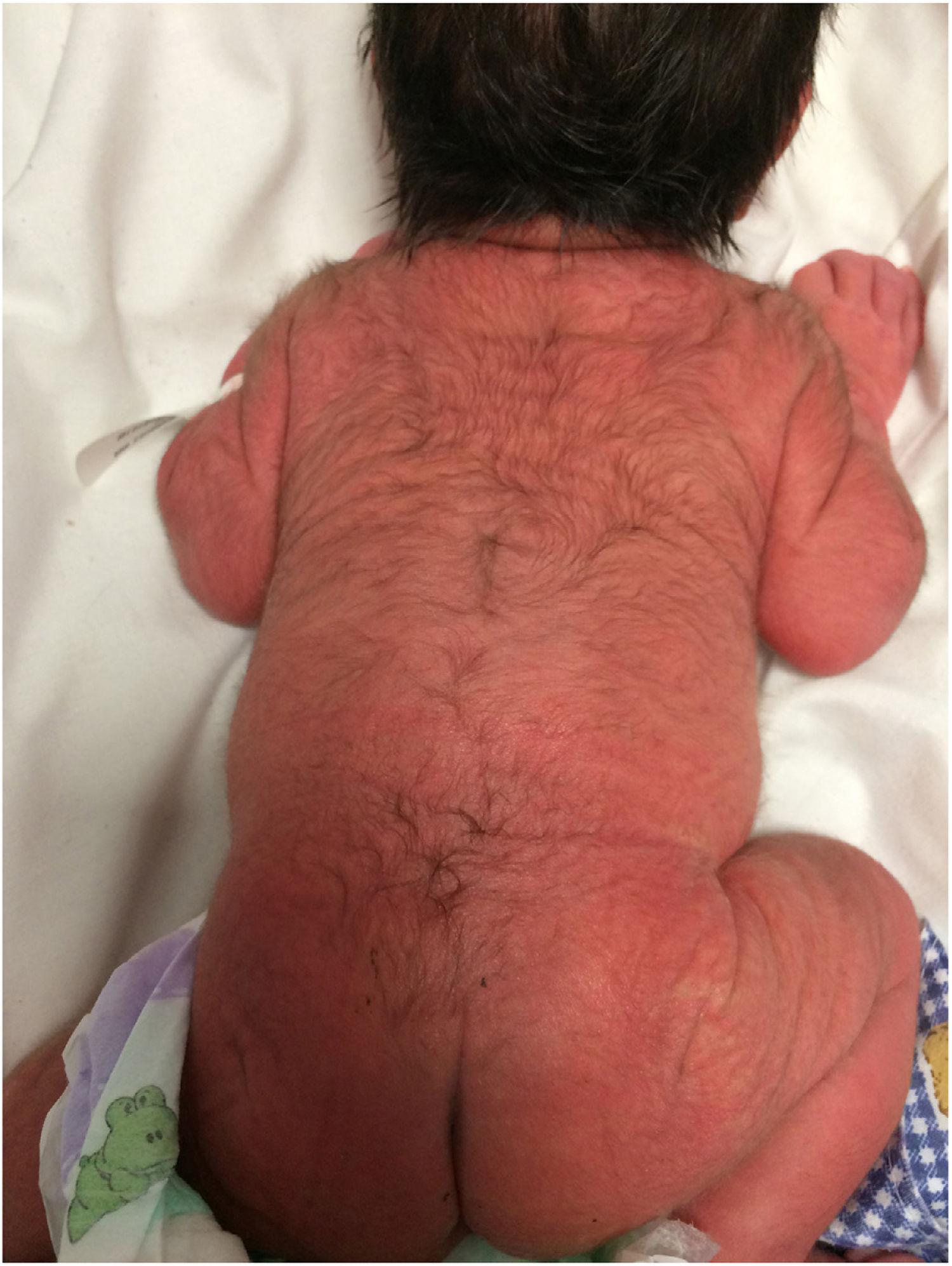
The majority of findings were categorized as benign or transient (99.9%; 95% CI, 99.8%–100%), and 2810 had at least 1 finding of this type. The most common one, lanugo (Fig. 2), was observed in 2763 neonates (98.3%; 95% CI, 97.7%–98.7%), followed in order of frequency by physiological scaling in 2240 (79.7%; 95% CI, 78.2%–81.1%), sebaceous hyperplasia (Fig. 3) in 2080 (73.3%; 95% CI, 71.6%–74.9%), and Epstein pearls (Fig. 4) in 1864 (66.3%; 95% CI, 64.5%–68.0%). Fig. 5 shows ETN lesions, a finding in 1554 neonates (55.3%; 95% CI, 53.4%–57%). Among the less frequently observed dermatoses, transient neonatal pustular melanosis (0.9%; 95% CI, 0.6%–1.3%) was noteworthy.
Vascular lesions were observed in 55.8% of the neonates (95% CI, 54.0–57.6). Salmon patches (Fig. 6) accounted for most of the vascular lesions; they were present in 1563 infants (55.6%; 95% CI, 53.8%–57.4%) and were observed on the nape of the neck, the eyelids, glabella, nose, philtrum, and in the sacral region. Less common lesions in this group were hemangioma precursors (0.5%; 95% CI, 0.3%–0.8%) and congenital hemangiomas (0.1%; 95% CI, 0.02%–0.3%) (Fig. 7).
Pigmented lesions accounted for 50.9% of the observations (95% CI, 49.1%–52.8%). They were mainly dermal melanocytosis, observed in 1127 neonates (40.1%; 95% CI, 38.9%–41.9%) and located in the sacral region and on buttocks and limbs. One infant had an atypical form of dermal melanocytosis (Fig. 8). Transient neonatal hyperpigmentation (24%; 95% CI, 22.5%–25.6%) was found on genitals, in axillas, at the base of the umbilical cord, and on the proximal nail fold. Less common lesions in this category, such as congenital melanocytic nevi, were seen in 1.7% (95% CI, 1.3%–2.3%); 92% of these nevi were small. No giant congenital melanocytic nevi were found during the study. Café au lait macules, seen in 1.4% of the population (95% CI, 1%–1.9%), were usually solitary, but 5 of the infants had more than 1 macule (1 had 3 macules and 4 had 2).
Less common categories were traumatic lesions (in 12.8%; 95% CI, 11.7%–14.1%) and congenital anomaliies (in 3.5%, 95% CI, 2.9%–4.3%).
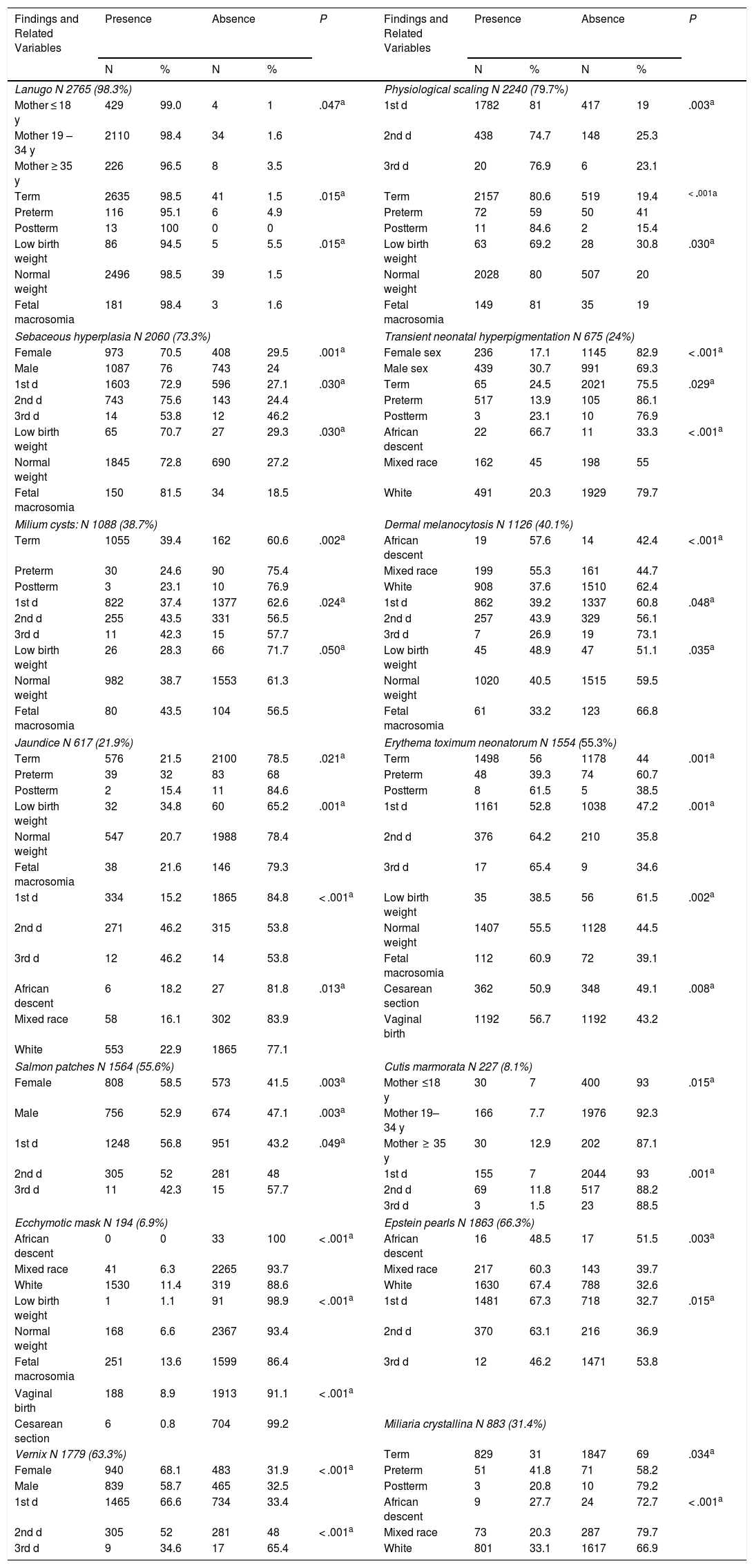
Table 3 shows the statistically significant associations between dermatologic findings and patient factors. (See the supplementary material for a table with all data for conditions with a frequency greater than 5% and their relationships with the analyzed variables.) Lanugo (P = .015), physiological scaling (P < .001), ETN (P = .001), transient neonatal hyperpigmentation (P = .029), and milium cysts (P = 0,002) were found more often in full-term and postterm neonates. However, jaundice (P = .021) and miliaria crystallina (P = .034) were found more often in preterm infants.
Dermatologic Findings and Significantly Associated Variables
| Findings and Related Variables | Presence | Absence | P | Findings and Related Variables | Presence | Absence | P | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | N | % | ||||
| Lanugo N 2765 (98.3%) | Physiological scaling N 2240 (79.7%) | ||||||||||
| Mother ≤ 18 y | 429 | 99.0 | 4 | 1 | .047a | 1st d | 1782 | 81 | 417 | 19 | .003a |
| Mother 19 – 34 y | 2110 | 98.4 | 34 | 1.6 | 2nd d | 438 | 74.7 | 148 | 25.3 | ||
| Mother ≥ 35 y | 226 | 96.5 | 8 | 3.5 | 3rd d | 20 | 76.9 | 6 | 23.1 | ||
| Term | 2635 | 98.5 | 41 | 1.5 | .015a | Term | 2157 | 80.6 | 519 | 19.4 | < ·001a |
| Preterm | 116 | 95.1 | 6 | 4.9 | Preterm | 72 | 59 | 50 | 41 | ||
| Postterm | 13 | 100 | 0 | 0 | Postterm | 11 | 84.6 | 2 | 15.4 | ||
| Low birth weight | 86 | 94.5 | 5 | 5.5 | .015a | Low birth weight | 63 | 69.2 | 28 | 30.8 | .030a |
| Normal weight | 2496 | 98.5 | 39 | 1.5 | Normal weight | 2028 | 80 | 507 | 20 | ||
| Fetal macrosomia | 181 | 98.4 | 3 | 1.6 | Fetal macrosomia | 149 | 81 | 35 | 19 | ||
| Sebaceous hyperplasia N 2060 (73.3%) | Transient neonatal hyperpigmentation N 675 (24%) | ||||||||||
| Female | 973 | 70.5 | 408 | 29.5 | .001a | Female sex | 236 | 17.1 | 1145 | 82.9 | < .001a |
| Male | 1087 | 76 | 743 | 24 | Male sex | 439 | 30.7 | 991 | 69.3 | ||
| 1st d | 1603 | 72.9 | 596 | 27.1 | .030a | Term | 65 | 24.5 | 2021 | 75.5 | .029a |
| 2nd d | 743 | 75.6 | 143 | 24.4 | Preterm | 517 | 13.9 | 105 | 86.1 | ||
| 3rd d | 14 | 53.8 | 12 | 46.2 | Postterm | 3 | 23.1 | 10 | 76.9 | ||
| Low birth weight | 65 | 70.7 | 27 | 29.3 | .030a | African descent | 22 | 66.7 | 11 | 33.3 | < .001a |
| Normal weight | 1845 | 72.8 | 690 | 27.2 | Mixed race | 162 | 45 | 198 | 55 | ||
| Fetal macrosomia | 150 | 81.5 | 34 | 18.5 | White | 491 | 20.3 | 1929 | 79.7 | ||
| Milium cysts: N 1088 (38.7%) | Dermal melanocytosis N 1126 (40.1%) | ||||||||||
| Term | 1055 | 39.4 | 162 | 60.6 | .002a | African descent | 19 | 57.6 | 14 | 42.4 | < .001a |
| Preterm | 30 | 24.6 | 90 | 75.4 | Mixed race | 199 | 55.3 | 161 | 44.7 | ||
| Postterm | 3 | 23.1 | 10 | 76.9 | White | 908 | 37.6 | 1510 | 62.4 | ||
| 1st d | 822 | 37.4 | 1377 | 62.6 | .024a | 1st d | 862 | 39.2 | 1337 | 60.8 | .048a |
| 2nd d | 255 | 43.5 | 331 | 56.5 | 2nd d | 257 | 43.9 | 329 | 56.1 | ||
| 3rd d | 11 | 42.3 | 15 | 57.7 | 3rd d | 7 | 26.9 | 19 | 73.1 | ||
| Low birth weight | 26 | 28.3 | 66 | 71.7 | .050a | Low birth weight | 45 | 48.9 | 47 | 51.1 | .035a |
| Normal weight | 982 | 38.7 | 1553 | 61.3 | Normal weight | 1020 | 40.5 | 1515 | 59.5 | ||
| Fetal macrosomia | 80 | 43.5 | 104 | 56.5 | Fetal macrosomia | 61 | 33.2 | 123 | 66.8 | ||
| Jaundice N 617 (21.9%) | Erythema toximum neonatorum N 1554 (55.3%) | ||||||||||
| Term | 576 | 21.5 | 2100 | 78.5 | .021a | Term | 1498 | 56 | 1178 | 44 | .001a |
| Preterm | 39 | 32 | 83 | 68 | Preterm | 48 | 39.3 | 74 | 60.7 | ||
| Postterm | 2 | 15.4 | 11 | 84.6 | Postterm | 8 | 61.5 | 5 | 38.5 | ||
| Low birth weight | 32 | 34.8 | 60 | 65.2 | .001a | 1st d | 1161 | 52.8 | 1038 | 47.2 | .001a |
| Normal weight | 547 | 20.7 | 1988 | 78.4 | 2nd d | 376 | 64.2 | 210 | 35.8 | ||
| Fetal macrosomia | 38 | 21.6 | 146 | 79.3 | 3rd d | 17 | 65.4 | 9 | 34.6 | ||
| 1st d | 334 | 15.2 | 1865 | 84.8 | < .001a | Low birth weight | 35 | 38.5 | 56 | 61.5 | .002a |
| 2nd d | 271 | 46.2 | 315 | 53.8 | Normal weight | 1407 | 55.5 | 1128 | 44.5 | ||
| 3rd d | 12 | 46.2 | 14 | 53.8 | Fetal macrosomia | 112 | 60.9 | 72 | 39.1 | ||
| African descent | 6 | 18.2 | 27 | 81.8 | .013a | Cesarean section | 362 | 50.9 | 348 | 49.1 | .008a |
| Mixed race | 58 | 16.1 | 302 | 83.9 | Vaginal birth | 1192 | 56.7 | 1192 | 43.2 | ||
| White | 553 | 22.9 | 1865 | 77.1 | |||||||
| Salmon patches N 1564 (55.6%) | Cutis marmorata N 227 (8.1%) | ||||||||||
| Female | 808 | 58.5 | 573 | 41.5 | .003a | Mother ≤18 y | 30 | 7 | 400 | 93 | .015a |
| Male | 756 | 52.9 | 674 | 47.1 | .003a | Mother 19–34 y | 166 | 7.7 | 1976 | 92.3 | |
| 1st d | 1248 | 56.8 | 951 | 43.2 | .049a | Mother ≥ 35 y | 30 | 12.9 | 202 | 87.1 | |
| 2nd d | 305 | 52 | 281 | 48 | 1st d | 155 | 7 | 2044 | 93 | .001a | |
| 3rd d | 11 | 42.3 | 15 | 57.7 | 2nd d | 69 | 11.8 | 517 | 88.2 | ||
| 3rd d | 3 | 1.5 | 23 | 88.5 | |||||||
| Ecchymotic mask N 194 (6.9%) | Epstein pearls N 1863 (66.3%) | ||||||||||
| African descent | 0 | 0 | 33 | 100 | < .001a | African descent | 16 | 48.5 | 17 | 51.5 | .003a |
| Mixed race | 41 | 6.3 | 2265 | 93.7 | Mixed race | 217 | 60.3 | 143 | 39.7 | ||
| White | 1530 | 11.4 | 319 | 88.6 | White | 1630 | 67.4 | 788 | 32.6 | ||
| Low birth weight | 1 | 1.1 | 91 | 98.9 | < .001a | 1st d | 1481 | 67.3 | 718 | 32.7 | .015a |
| Normal weight | 168 | 6.6 | 2367 | 93.4 | 2nd d | 370 | 63.1 | 216 | 36.9 | ||
| Fetal macrosomia | 251 | 13.6 | 1599 | 86.4 | 3rd d | 12 | 46.2 | 1471 | 53.8 | ||
| Vaginal birth | 188 | 8.9 | 1913 | 91.1 | < .001a | ||||||
| Cesarean section | 6 | 0.8 | 704 | 99.2 | Miliaria crystallina N 883 (31.4%) | ||||||
| Vernix N 1779 (63.3%) | Term | 829 | 31 | 1847 | 69 | .034a | |||||
| Female | 940 | 68.1 | 483 | 31.9 | < .001a | Preterm | 51 | 41.8 | 71 | 58.2 | |
| Male | 839 | 58.7 | 465 | 32.5 | Postterm | 3 | 20.8 | 10 | 79.2 | ||
| 1st d | 1465 | 66.6 | 734 | 33.4 | African descent | 9 | 27.7 | 24 | 72.7 | < .001a | |
| 2nd d | 305 | 52 | 281 | 48 | < .001a | Mixed race | 73 | 20.3 | 287 | 79.7 | |
| 3rd d | 9 | 34.6 | 17 | 65.4 | White | 801 | 33.1 | 1617 | 66.9 | ||
Lanugo (P = .015), physiological scaling, (P = .03), sebaceous hyperplasia (P = .03), ETN (P = .002), and milium cysts (P = .058) were seen more often in normal-weight neonates or those with fetal macrosomia.
Sebaceous hyperplasia (P = .001) and transient neonatal hyperpigmentation (P < .001) were more frequent in male neonates. Vernix caseosa (P < .001) and salmon patches (P = .003), on the other hand, were more often seen in female neonates.
Pigmented lesions such as dermal melanocytosis (P < .001) and transient neonatal hyperpigmentation (P < .001) were more common in neonates of African descent.
Lanugo (P = .047) was associated with infants born of adolescent mothers and cutis marmorata was more common in those born to older mothers (P = .015).
ETN was more frequent after vaginal births (P = .008). Traumatic lesions such as ecchymotic mask also occurred more often during vaginal births (P < .001).
Vernix caseosa was seen most often on the first day of life (P < .001), whereas jaundice (P < .001) and ETN (P < .001) were reported more often in neonates examined on the second or third days.
DiscussionDermatologic conditions in the early days of life are highly prevalent and overlap. Most are benign, transient, and diagnosed clinically. They resolve spontaneously and are part of adaptation to life outside the womb. They are also related to such neonatal factors as gestational age, birth weight, and ethnicity as well as to maternal and gestational factors.1–11 It is important to be able to recognize these conditions and diagnose them clinically in order to avoid unnecessary testing and to reassure the infant’s caregivers.
Studies in various countries have demonstrated the prevalence of dermatoses in neonates and their associations with different factors,3–11,14 but until now data have not been available for Uruguay.
The frequency of neonatal dermatologic conditions varies in the literature. In our study the overall prevalence was similar to the high rates described for Spain (99.2%),4 Brazil (99.2%),5 and Australia (99.3%).8 Several skin conditions may be present at the same time. Reginatto et al5 reported a mean of 3.23 findings per neonate; in our study the median number was 8 per neonate.
Benign, transient lesions were the most common ones in our study, consistent with previous reports.3–11 However, there is no consensus in the literature about which findings predominate in each category: sebaceous hyperplasia has been reported to be the most common in Spain (75%),4 and Hungary (29%),3 whereas lanugo has been reported to be the most common in Brazil (38%)5 and northern Italy (68%).9 Lanugo was by far the most common finding in our study, at a prevalence of 98.3%, a rate that was even higher than reported in the international literature consulted.3–9
Transient neonatal pustular melanosis was among the less frequent of the benign, transient lesions found. It was diagnosed clinically by the presence of pustulous lesions on healthy skin from birth or more advanced lesions such as collarette scaling and residual hyperpigmentation. The global prevalence of this diagnosis is less than 1%, but it is considerably higher in neonates of African descent (5%).2 In our study with few neonates of African extraction, the frequency was 0.9% (95% CI, 0.6%–1.3%).
In the categories of vascular and pigmented lesions, the conditions observed most often were salmon patches and dermal melanocytosis, consistent with reports in the international literature.4,10
The prevalence of salmon patches varies by country and ethnicity, from 20.7% in India7 to 83% in the United States.6 In our study the frequency was 55.3% (95% CI, 53.8%–57.4%). Hemangioma precursors, which may be present at birth as telangiectatic macules surrounded by pale halos, vary in frequency from 1.6% to 3.5% in the literature.2,3,15 The rate was much lower in our study (0.5%; 95% CI, 0.3%–0.8%), probably attributable to the small number of preterm infants we examined, since such infants are at risk for infantile hemangiomas.2,3,15
Dermal melanocytosis, described as a slate-gray macule, also varies in frequency, from 20% of neonates in Egypt16 to 84.7% in India,7 suggesting that ethnicity exercises a significant influence over this condition, which is more prevalent in higher-phototype skin categories.
According to data from the National Statistics Institute of Uruguay and based on self-reported information, our national population is distributed ethnically as follows: 87.4% of the population are White, 2% are of African descent, and 10% are of mixed races (including African/White, Native American/White, and African/White/Native American individuals).17 In our sample of neonates, with a similar ethnic distribution, the frequency of dermal melanocytosis was 40% (95% CI, 38.9%–41.9%).
Lesions such as lanugo, physiological scaling, ETN, and hyperpigmentation do not occur independently of gestational age and birth weight. We observed these findings in postterm, normal weight, and macrosomal neonates. These observations are consistent with reports in the literature1,2,18–21 as well as the fact that longer gestational age is related to greater thickness of the corneal layer and better functioning of the skin barrier and immune system.
Neonates of African descent more often presented pigmented lesions such as transient neonatal hyperpigmentation (P = .001) and dermal melanocytosis (P = .001). This association is consistent with the literature,2,3,16,22,23 but our conclusions are limited by the small number of African-descent infants in this study. A new design to include more such neonates would be required to be sure this observation holds. Higher incidence rates of pigmented lesions in darker-skinned individuals with more and larger melanosomes containing more melanin would explain the association.23
Some skin findings are related to delivery mode. Like Ábrahám et al3 and Monteagudo et al,4 we observed an association between the presence of traumatic lesions (eg, an ecchymotic mask) and vaginal birth (P = .001).
A possible relationship between ETN and delivery mode is still under debate. We saw a higher proportion of ETN in neonates delivered vaginally (P = .008), possibly because of rapid colonization of skin during the passage through the birth canal. Marchini et al21 speculated that as the number of postnatal hours increases so does colonization, triggering an immune-mediated response that manifests as ETN. This explanation could account for our observation of higher rates of ETN in 3-day-old infants (P < .001).
Further studies using logistic regression modeling are required to deepen our understanding of associations between dermatologic findings and the variables analyzed in this study.
A limitation of our study was the low percentage of neonates with gestational ages of less than 37 weeks (4%), which was not representative of the percentage of preterm infants delivered in our hospital (10%). Therefore, dermatologic findings in this group may have been underrepresented.
A strength of the study is the large number of infants examined. This population size allowed us to observe even lesions described as uncommon in the literature.
ConclusionAll neonates have skin characteristics that reflect their adaptation to extrauterine life. Most are benign and transient. Maternal age, delivery mode, and certain neonatal factors such as gestational age, birth weight, sex, and ethnicity are associated with specific conditions. This multidisciplinary study on dermatologic findings in neonates is the first of its kind in Uruguay. The sample was representative of the population born in a national referral hospital.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: De María MK, Borda KM, Arretche VN, Gugelmeier N, Mombelli R, de los Santos AV, et al. Epidemiología y factores predisponentes de los hallazgos dermatológicos en neonatos de Uruguay. Actas Dermosifiliogr. 2020;112:414–424.