Retronychia is a recently described disorder caused by ingrowth of the proximal nail plate into the proximal nail fold. This situation provokes chronic paronychia refractory to antimicrobial therapy. Ultrasound has been proposed as the noninvasive method of choice to confirm the diagnosis and rule out other differential diagnoses, particularly local tumors and arthritic disease. The presence of 2 or more overlapping nail plates and a reduced distance between the root of the nail plate and the base of the distal phalanx could be the ultrasound hallmarks of this condition. Nail plate avulsion is the treatment of choice and is curative. Knowledge of retronychia is still limited among dermatologists, which can lead to diagnostic and therapeutic errors and delay. This has prompted us to present this new case.
La retroniquia es un proceso emergente en el que la parte proximal de la lámina ungueal se encarna en el pliegue ungueal proximal, produciendo una paroniquia crónica refractaria a terapias antimicrobianas. La ecografía se ha postulado como la prueba no invasiva de confirmación y para diagnóstico diferencial, sobre todo con afecciones tumorales y artríticas locales. La presencia de dos o más láminas ungueales superpuestas y la disminución de la distancia entre el origen de la lámina ungueal y la base de la falange distal podrían ser los criterios ecográficos distintivos de esta entidad. La avulsión quirúrgica de la lámina ungueal es la terapia de elección y curativa de la misma. Su conocimiento todavía está poco difundido entre los dermatólogos, ocasionando errores y demoras diagnósticas y terapéuticas, lo que nos ha motivado a la presentación de un nuevo caso.
The term retronychia (proximal ingrowing nail), was coined by Berker and Rendall1 in 1999. The condition emerged as a distinct entity in 2008, after the presentation of a cases series by members of the European Nail Society (ENS). Retronychia progresses with ingrowth of the proximal nail plate into the proximal nail fold (PNF), the presence of 2 or more overlapping generations of nail plate under the PNF, clinical signs of chronic proximal paronychia, and a yellowish nail that does not grow.2,3
The pathogenesis of retronychia is not well known, although the condition is thought to be a complication of onychomadesis.3 Thus, repeated injury to the distal end of the nail triggers onycholysis that would first break the continuity and then the alignment between the nail matrix and the nail plate. By losing its proximal attachment to the nail bed and being subject to repeat injury, the nail plate gradually moves backward until it embeds itself in the cul-de-sac of the PNF. An inflammatory process with formation of granulation tissue is triggered in the cul-de-sac and nail bed, thus accounting for the clinical signs of paronychia. In addition, the presence of inflammatory phenomena would prevent the attachment of the new growing nail plate to the proximal part of the nail bed, thus leading again to onychomadesis, backward movement, and ingrowth into the PNF. This process can thus generate a vicious cycle in which up to 4 generations of nail plate overlap under the PNF.4
Case DescriptionThe patient was a 22-year-old man who practiced mountaineering, for which he used tight boots. He came to the clinic with a 1-year history of absent nail growth on the great toe of the right foot and episodes of proximal exudative paronychia. Although the inflammatory signs improved to some extent with oral antibiotics, the patient continued to complain of pain in the PNF. He had taken ciprofloxacin during the previous 2 weeks because of growth of a culture of exudate of Escherichia coli that was sensitive to the antibiotic. He also reported what appeared to be a cut in the proximal part of the nail plate.
Examination revealed erythema and pain in the PNF on palpation, as well as proximal onychomadesis with a thick yellowish nail plate (Fig. 1A). Slight lateral deviation was observed in both great toes. No abnormal results were reported for the bacterial and fungal cultures or radiology examination of the toe.
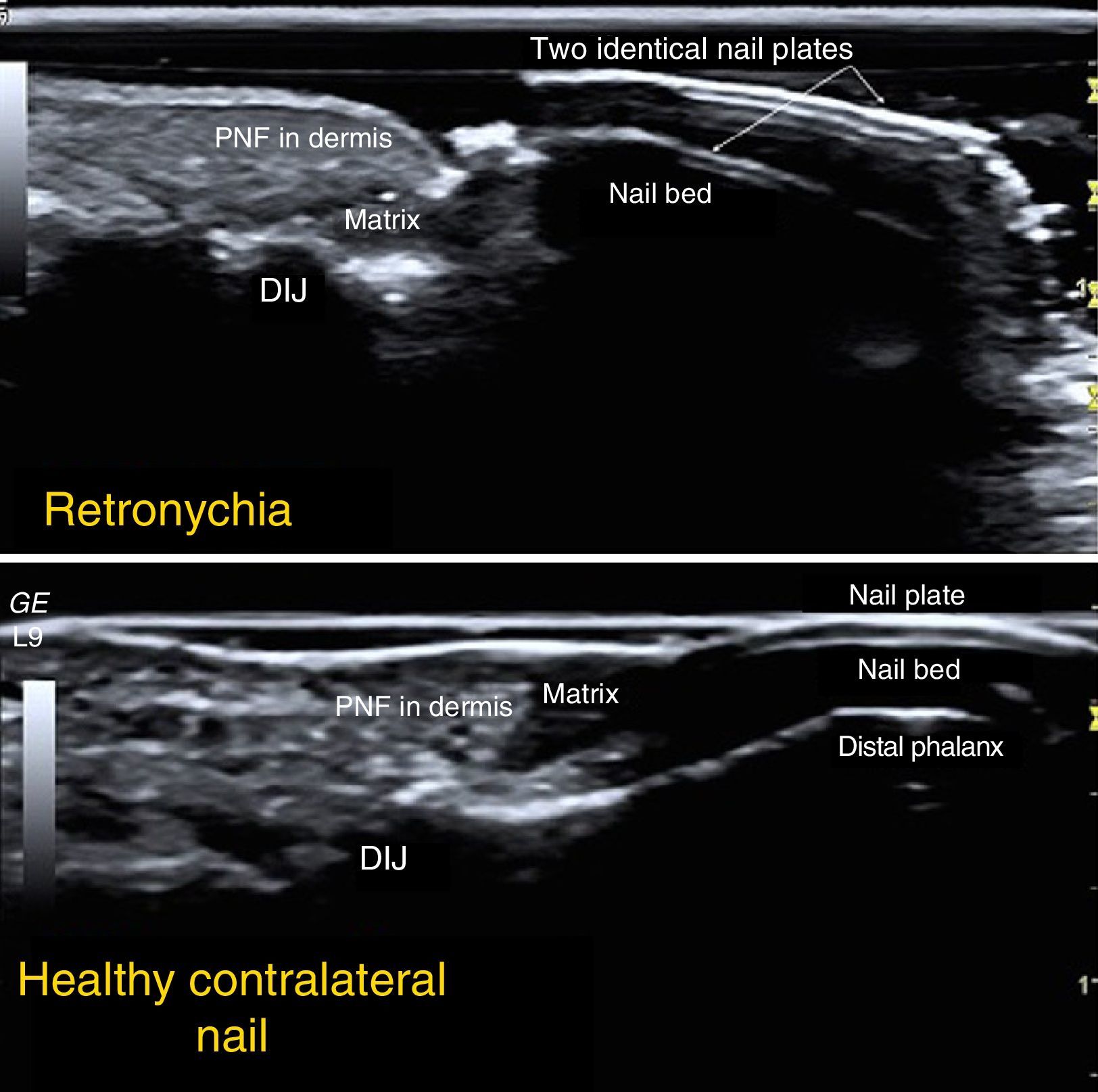
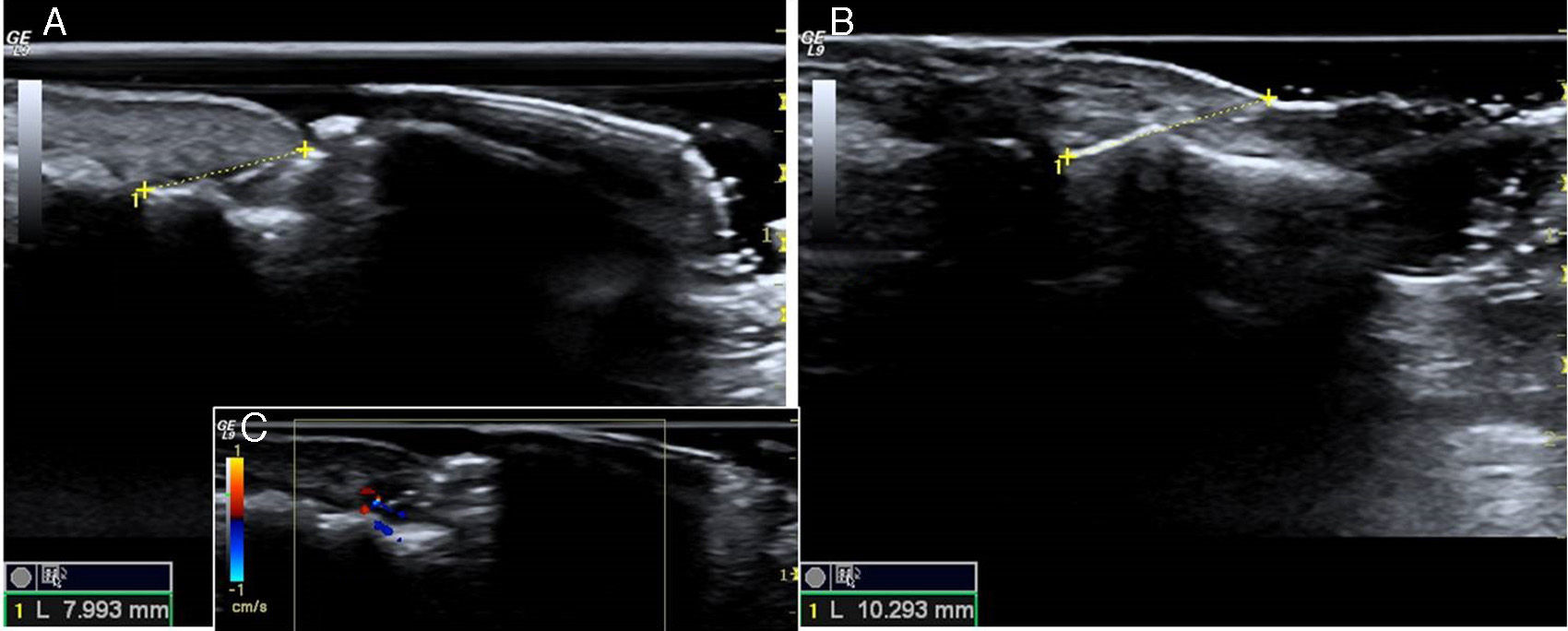
Ultrasound study with a multifrequency linear probe (9-14MHz) and high-resolution device (GE Medical Systems) revealed overlapping nail plates with a hypoechoic space between them, reduction of the distance between the root of the nail plate and the base of the distal phalanx at the level of the distal interphalangeal joint, as well as posterior acoustic shadowing deep under the nail plate. The PNF was thicker in the affected nail than in the healthy contralateral nail. The Doppler signal was slightly enhanced in the proximal part of the nail bed at the root of the matrix (Figs. 2 and 3).
Ultrasound study: longitudinal image characteristic of retronychia, with 2 overlapping nail plates and a hypoechoic space between them, together with posterior acoustic shadowing under the lower nail plate. Lower panel, healthy contralateral nail. DIJ indicates distal interphalangeal joint; PNF, proximal nail fold.
A and B, Ultrasound-based comparison between images from the great toes. In the nail affected by retronychia (A), the distance between the root of the nail plate and the base of the distal phalanx (at the level of the distal interphalangeal joint) is reduced. C, Enhanced Doppler signal in the proximal part of the nail bed.
Once the diagnosis of retronychia was confirmed, surgical avulsion of the nail was performed using an anterior approach, and the 2 nail plates were found to be overlapping at the proximal end, with granulation tissue and keratotic material between them (Fig. 4). Histopathology confirmed these findings. A new nail plate grew over the following 12 months, with slight distal thickening and yellowing (Fig. 1B).
Surgical avulsion. A, Appearance of both nails before surgery. B, Affected nail higher proximally than distally. C, Proximal detachment with a Freer elevator. D, Removal of the nail plates using Radolf nail pulling forceps. E, Appearance of the nail bed after avulsion. F, Overlapping nail plates forming a “sandwich,” with granulation tissue between them at the proximal end.
A total of 64 cases of retronychia have been reported, and most were included in multicenter studies carried out by experts from the ENS.2,4–15 Despite the wide age range reported (10-71 years), the mean age is 25 years. The condition mainly affects women (81%).
Retronychia affects the great toe unilaterally, although at least 7 cases of bilateral involvement1,2,4,10,13 and 9 cases of retronychia affecting the nails of the hands1,2,7,8 have been reported.
The most common triggers are repeated minor injuries, such as those that occur while jogging, walking, and dancing and those that result from having long nails or wearing heels or uncomfortable footwear. However, most patients do not associate their disease with these injuries. There have been at least 10 cases in which no trigger was identified2,4,11,12,14; in a further 8 cases, the cause was acute injury such as crushing, burns, and previous nail surgery.2,4,5,7,8,10 In a small number of cases, the condition developed in the setting of a systemic disease (eg arthritis), anorexia nervosa,2 and admission to the intensive care unit.7 Lateral deviation of the great toe has been considered a potential predisposing factor.4,6
Retronychia manifests with local pain and difficulty walking (in cases where the nails of the feet are affected), and as erythema, edema, and exudation in the PNF and a dull, thick, yellowish nail plate that does not grow. Also characteristic of this condition is the finding of a nail that is higher proximally than distally.2,4,6,12,14 Granulation tissue can sometimes be observed under the cuticle, as can the sharp proximal edge of the nail plate (see present case).4,10,11,13,14 In 1 case, retronychia has also presented as paronychia that was culture-positive for gram-negative pathogens, yet resistant to antibiotics.4
Diagnosis of retronychia is based on clinical findings, although ultrasound can be used as a noninvasive confirmatory test and in presurgical differential diagnosis. The ultrasound criteria for confirmation of diagnosis are presence of ≥2 overlapping nail plates, shortening of the distance between the root of the nail plate and the base of the distal phalanx (at the level of the distal interphalangeal joint, thus indicating the posterior shift of the nail), and diminished echogenicity in the dermis of the PNF and proximal nail bed owing to the presence of inflammation and onycholysis.7,8 In the present case, we also observed absence of signal deeper under the nail plate, which was attributed to posterior acoustic shadowing. In 1 case, Doppler ultrasound revealed a slight increase in blood flow in the proximal nail bed.7
The differential diagnosis of retronychia should include diseases with the appearance of chronic paronychia, namely, candidal or bacterial infection, subungual cysts or tumors (eg, squamous cell carcinoma, melanoma, glomus tumor, and enchondroma), arthritic processes (eg, psoriasis), and processes associated with medication (eg, retinoids, ciclosporin, protease inhibitors, and epidermal growth factor receptor inhibitors).5,6,9,11,12
Surgical avulsion of the old nail plate and the subsequent ingrowing nail plate(s) with a proximal approach confirms the diagnosis, leads to rapid pain relief, and is the curative treatment of choice for this process.2,4,6 Avulsion of the most superficial nail plate alone is not sufficient and leads to relapse.5,11,14 However, relapse is unusual, as is permanent postsurgical nail dystrophy. In a series of young and adolescent patients, the new nail was thick and yellowish and grew very slowly in 33% of patients after successful surgical avulsion. Medical treatment with potent topical corticosteroids was associated with a high relapse rate in the series.12
In conclusion, we report a new case of retronychia that was probably triggered during the practice of mountaineering. The condition was repeatedly confused with infectious paronychia, and it took more than 1 year to confirm the diagnosis and provide adequate treatment. These observations are consistent with reports on patients with retronychia in the literature.4,9,11,13 In addition, even though retronychia may not be as uncommon as previously thought,12 only 1 case has been reported in the Spanish medical literature.15
Ethical DisclosuresProtection of humans and animalsThe authors declare that no tests were carried out in humans or animals for the purpose of this study.
Confidentiality of dataThe authors declare that no private patient data appear in this article.
Right to privacy and informed consentThe authors obtained informed consent from the patients and/or subjects referred to in this article. This document is held by the corresponding author.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Alonso-Pacheco ML, de Miguel-Mendieta E, Maseda-Pedrero R, Mayor-Arenal M. Retroniquia: estudio ecográfico y tratamiento quirúrgico de un caso. Actas Dermosifiliogr. 2016;107:e33–e37.