Reconstruction of a full-thickness nasal alar defect may be complex because of the need to repair all involved structures (nasal mucosa, cartilage, and skin)1–3 and preserve function while aiming for a good esthetic outcome.
The endonasal mucosa can be repaired by using inverted or folded flaps.1 The melolabial region is the most common donor site although septal mucoperichondrial flaps can also be used.
Providing structural support is usually the most complicated aspect of the technique. Alternative techniques include the use of bone or autologous cartilage (from the septal, atrial, or costal region), or alloplastic material, using biocompatible materials such as titanium1–4 or polyethylene.5 With biocompatible materials, morbidity at the donor site is avoided,2 and the risk of necrosis is decreased given that neovascularization is not required.1–3 However, unlike autologous tissue, prosthetic material can be extruded, and there is a greater risk of infection given that it is a foreign body; the material may also interfere in future imaging studies.1,2 Nevertheless, in the case of titanium mesh, integration of the prosthetic material with the surrounding tissue has been reported,1,4 thus minimizing the risk of extrusion if the alloplastic material is adequately covered.1–3
Finally, skin reconstruction is usually performed with free or pedicled flaps usually taken from the nasal, melolabial, or frontal region.
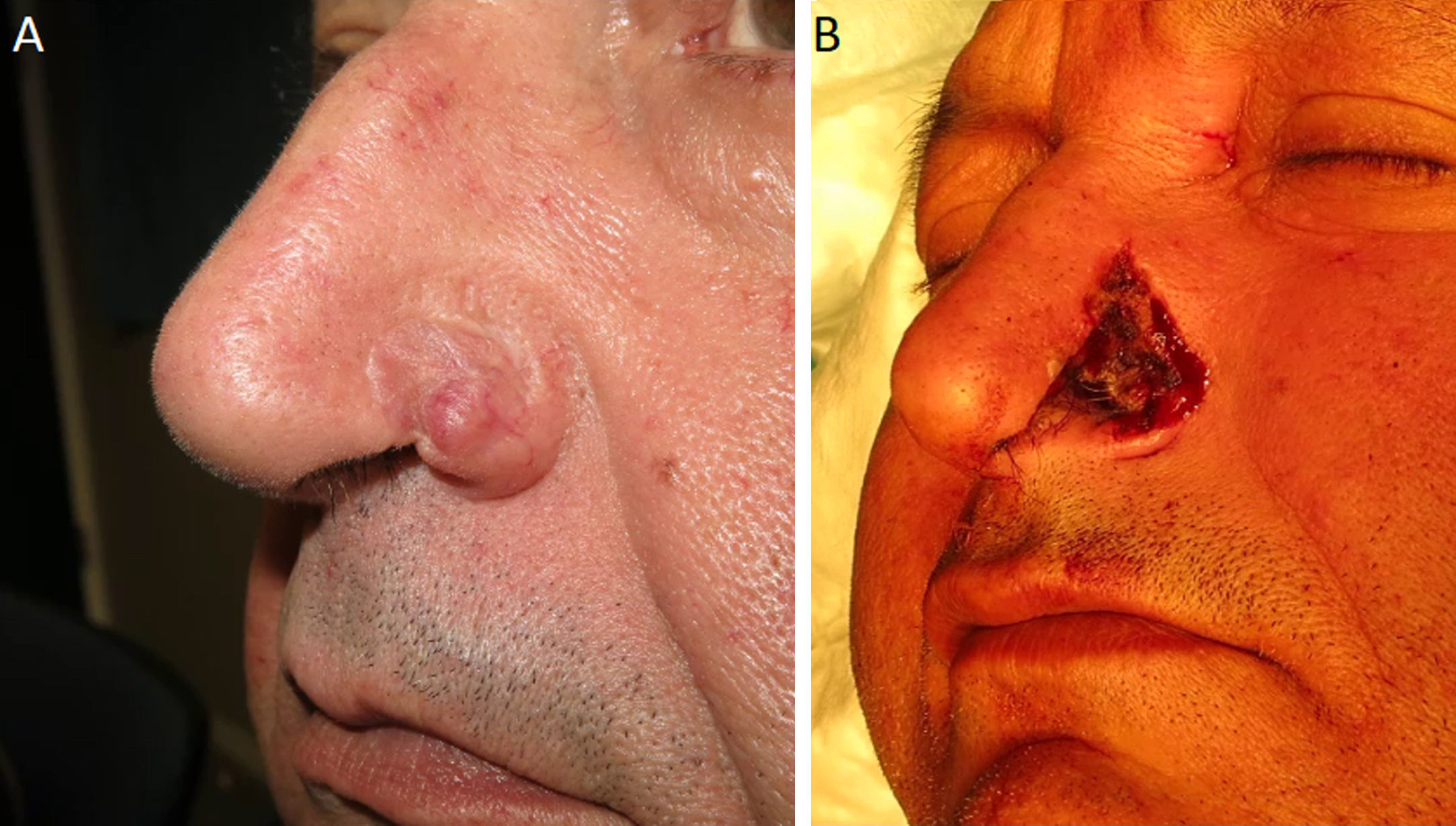
In a surgical video, we present the reconstruction of a full-thickness alar nasal defect with titanium mesh after Mohs surgery for basal cell carcinoma (Fig. 1) (video in supplementary material).
Description of the TechniqueTo reconstruct the full-thickness defect of the left nasal ala (Fig. 1B), a melolabial flap was folded over a 2-mm thick titanium mesh (Synthes-Statec, Medican FA, Madrid) as the supporting structure.
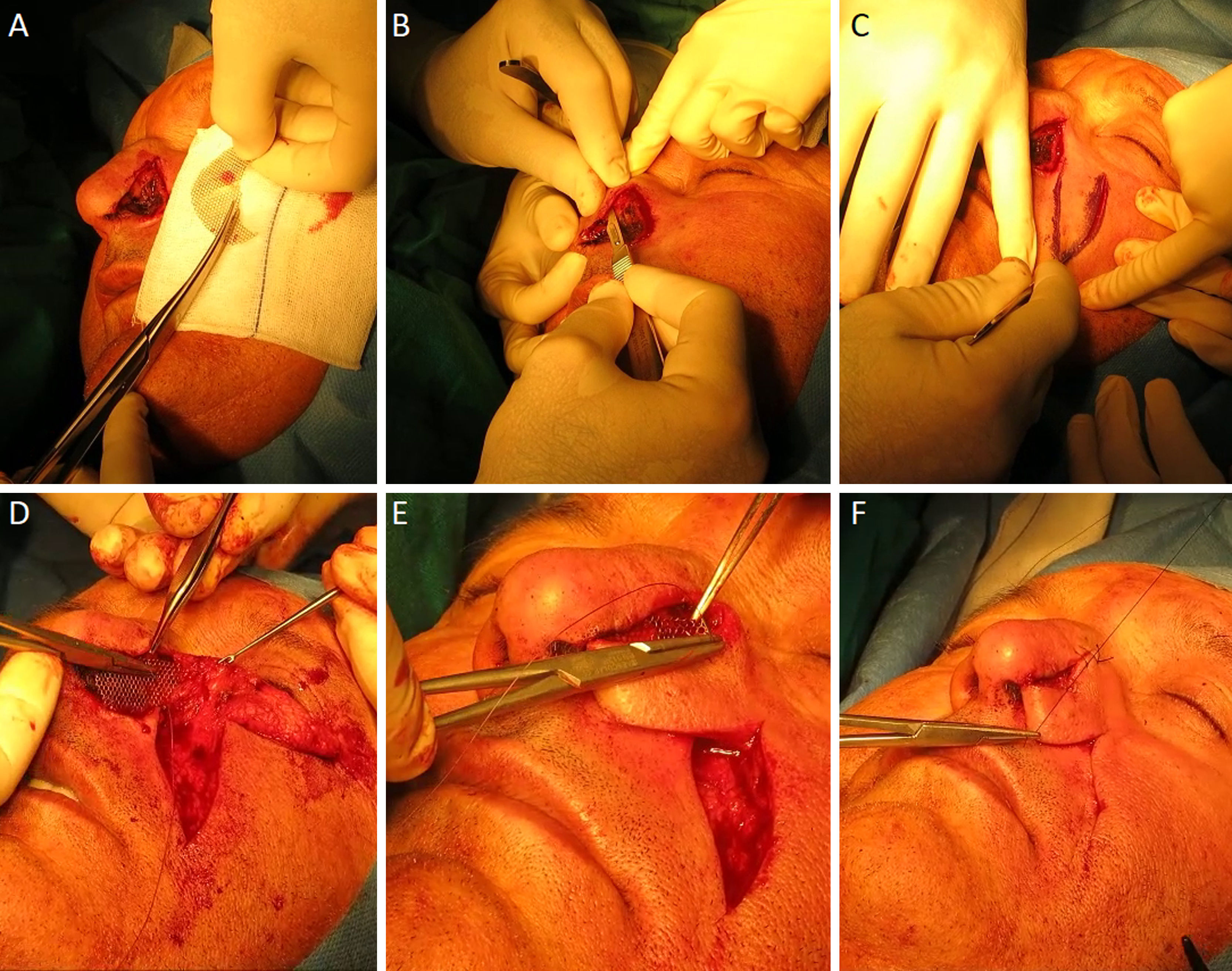
Under local anesthetic, the procedure began by freshening the borders of the defect following Mohs surgery to remove a basal cell carcinoma. The titanium mesh was designed, cut, and molded to the final size of the defect (Fig. 2A). To guarantee that the mesh was suitably anchored, an incision of several millimeters was made into the perilesional skin to form a pocket (Fig. 2B).
A, Design and cutting of titanium mesh according to the size of the final defect. B, Incision parallel to the skin in the subcutaneous cell tissue in healthy skin surrounding the defect, forming a pocket to subsequently hold the titanium mesh in place. C, Incision of melolabial flap. D, Anchoring the titanium mesh with absorbable 4/0 suture. E, Start of the melolabial flap suture folded over the titanium mesh by its distal end (forming the internal face of the nasal wall). F, External suture of the flap with 4/0 silk thread.
Then, incision of the melolabial flap (Fig. 2C) (with the same width as the defect) and dissection of the subcutaneous plane were performed. Once finished, mobility and final positioning were checked.
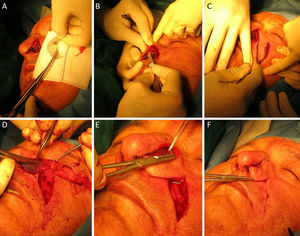
The titanium mesh was introduced into the incisions made at the edges of the defect and it was held in place with an absorbable 4/0 braided suture (Vicryl) (Fig. 2D). Before starting to fold the flap over the titanium mesh and suturing, careful hemostasis was performed and the most distal part of the flap was narrowed so that it would fit as closely as possible the endonasal mucosa. Once folded, the internal face of the distal end of the flat was sutured to the titanium mesh and to the healthy surrounding skin, starting from the tip, using a strand of absorbable 4/0 braided suture (Vicryl) (Fig. 2E), thus reconstructing the internal face of the alar wall. Finally, the rest of the flap was sutured (to contour the external face of the ala) with 4/0 silk thread (Fig. 2F) and the secondary defect was closed directly from the donor area with a continuous blocked suture using 4/0 silk thread (Fig. 3A-C).
IndicationsFull-thickness skin defects at the nasal site, in which the use of other, simpler, reconstructive techniques will likely lead to collapse of the nasal fossa or a poor esthetic outcome or, in view of the size, the use of autologous cartilage as support material may have a high risk of necrosis or distortion of the donor region.
ContraindicationsThere is no absolute contraindication. Relative contraindications include coagulation disorders and risk factors for skin ischemia (smoking habit, prior radiotherapy, diabetic foot, etc.) that would compromise the viability of the flap, and the indication of adjuvant radiotherapy.
Complications- •
Infection
- •
Hemorrhage, hematoma, and skin necrosis
- •
Extrusion of prosthetic material
- •
Temporary or permanent sensory alterations due to lesions to nerve structures
- •
Increased risk of radionecrosis
- •
Excessive thickness of the nasal ala that could lead to a poor esthetic outcome and even obstruction of the nasal fossa
Nasal reconstruction with a titanium mesh is a good reconstructive option in large full-thickness, nasal defects in which there is a risk of collapse of the nasal fossa and where the use of other flaps is not a viable alternative and the use of cartilage grafts could be compromising. The intervention is laborious and presents a certain technical complexity, but as shown, good functional and esthetic outcomes can be achieved (Fig. 3D-F).
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Fernández Canga P, Castiñeiras González J, Rodríguez Prieto MA. Reconstrucción de un defecto de espesor total en ala nasal con malla de titanio. Actas Dermosifiliogr. 2020;111:265–268.