We find ourselves in a socially atypical situation owing to the sudden change in our once normal living patterns. Our relationship with the environment has been affected by the COVID-19 pandemic, especially in terms of spending time outdoors.
Lockdown has created a situation in which most people have had less exposure to sunlight than usual, and this in turn has led to a springtime where degrees of exposure are similar to, or even lower than, those of winter. In terms of exposure, therefore, we might say that we have had a longer winter. This in turn leads us to believe that as the positive effects of naturally progressive exposure to sunlight on the skin have diminished, the natural biological response in the skin has also been altered. Hence, cutaneous synthesis of vitamin D, which is our greatest source of vitamin D, has been hampered by the lockdown, during which many people have not been exposed to sunlight in several weeks. Blood vitamin D levels vary according to the season, with lower values in winter than in summer1; however, during the COVID-19 lockdown, the winter low-exposure period has been extended by more than 3 months. Low vitamin D levels have pathophysiological consequences, and given that vitamin D can reduce the risk of infection through various mechanisms, the possibility that a deficiency could render us more susceptible to infection by coronavirus is somewhat alarming.2 Consequently, various sectors, including health care, have recommended direct—albeit brief—exposure to sunlight in order to increase serum vitamin D levels.3 Similarly, we should not forget the benefits of exposure to sunlight for our state of mind, which is considerably affected by the current situation, through stimulation of the neurotransmitters involved in the mechanisms underlying emotional well-being.
Easing of the lockdown has been planned in phases by government bodies as a gradual, responsible, and considerate “return to normal”. However, as far as our skin is concerned, the risk of direct exposure resulting in sunburn is greater, because the usual change from winter to spring at the latitude of Spain coincides with a gradual change in the incidence of solar radiation, thus enabling an acclimatization that is also gradual. Our pigmentation system is still in the winter period, with melanin levels that are lower than usual for the different skin phototypes. Therefore, the protection provided by progressive melanogenesis is very limited, since it depends directly on the impact of UV radiation on the skin.4 Lockdown has curbed the processes of melanogenesis, hyperkeratosis, and epidermal hyperplasia in response to the gradual acclimatization of the skin to sunlight, thus making the skin more sensitive to more aggressive and energetic solar irradiation (UV).5 In addition, the photoimmune response may be affected by the lack of exposure to sunlight, thus favoring an increase in the incidence of photosensitivity disorders resulting from the absence of a process of vaccination or hardening.6
Solar irradiation values with the potential to cause erythema are expressed as the ultraviolet index (UVI). Normal maximum UVI values in our region at the start of spring are 3-4. In this case, easing of lockdown coincided with a summertime outside temperature and a maximum daily UVI of 9 or 10.7 At such values, persons with low skin phototypes are exposed to the minimal erythema dose in less than 20 minutes and therefore experience sunburn.
Furthermore, heat plays a double-negative role in the skin. On the one hand, during the early months of spring, the moderate temperature means that we are exposed to sunlight while fully clothed (as on cloudy days), whereas, from May onward, the increase in temperatures means that we are exposed to sunlight with less clothing, when the UVI is at yearly maximum values. On the other, this period of the year is characterized by very high temperature peaks that can worsen lesions caused by UV radiation.
Therefore, when people are keen to be outdoors after the long lockdown period, there is clearly an increased risk of sunburn. The skin has had no time to adapt, and this could have long-term repercussions in the form of an increased incidence of skin cancer.
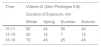
Healthy exposure is achieved by ensuring that the dose of UV radiation is sufficient to achieve the positive effects of sunlight on our body and to minimize the risk of damage resulting from overexposure. UVI values can be used to calculate the minutes of exposure taken to reach the minimal erythema dose. Table 1 shows the minutes of exposure to sunlight at midday in summer and winter, by skin phototype, that would be necessary to develop erythema (sunburn) and to produce a healthy dose of vitamin D.
Minimum Dose of UV Radiation Necessary to Produce Erythema and Synthesis of Vitamin D Corresponding to an Intake of 1000 IU and Minutes of Exposure Necessary to Produce These Doses During the Middle of the Day by Season.
| Skin Phototype | Minimal Erythema Dose, | Erythema | Minimal Dose of Vitamin D, | Vitamin D | ||
|---|---|---|---|---|---|---|
| mJ/cm2 | Duration of Exposure, | mJ/cm2 | Duration of Exposure, | |||
| min | min | |||||
| Summer | Winter | Summer | Winter | |||
| I | 20 | 21 | 64 | 3.7 | 6 | 17 |
| II | 25 | 26 | 80 | 4.7 | 7 | 21 |
| III | 30 | 32 | 96 | 5.6 | 8 | 25 |
| IV | 45 | 48 | 144 | 8.4 | 13 | 38 |
| V-VI | > 60 | 64 | 192 | > 11 | 17 | 51 |
Furthermore, the duration of exposure necessary to produce erythema and for synthesis of vitamin D differs with the time of day. Thus, this is longer in the morning and the evening because of the daily cycle of sunlight, where maximum radiation is around midday (Table 2). Photoprotective measures are recommended when the incidence of solar UV is high, since the doses of UV necessary to produce vitamin D are low and can be reached with a simple walk and exposure of small areas of the body, such as the face and hands. Table 3 summarizes the recommendations for the general public so that the benefits of the sun can be obtained without health risks.
General Recommendations on Exposure to Sunlight and Photoprotective Measures for the General Population and Specific Groups.
| • Consult the local UV index via the media or using specific applications (e.g., UV-Derma, which is the app of the AEDV). |
| • Gradual exposure to sunlight in order to facilitate adaptation of the skin and favor natural defense mechanisms (melanogenesis, epidermal thickening). Above all, exposure should be avoided during the middle of the day. |
| • Taking advantage of shade. Staying in the shade can minimize direct exposure to sunlight. In fact, using one’s own shadow as an indicator of the incidence of solar radiation is easy: if the shadow is shorter than one’s height, then it is time to look for shade. |
| • Physical measures. Use materials that minimize the “hole” effect, such as knitted fabrics, and dark colors, technical sports fabrics, and products labeled with a high UV protection factor that cover most of the body surface. |
| Use wide-brimmed caps and hats |
| Use approved sunglasses (UV > 400 and categories 2, 3, and 4) |
| Use beach umbrellas |
| • Topical sunscreens whose SPF is high (SPF 30-50) or very high (SPF 50+). These should be applied generously some minutes before exposure and renewed as necessary. It is important not to forget to apply photoprotection on cloudy days. |
| • Hydration. Good hydration is essential during periods of high solar radiation and temperatures, since more liquids are lost. |
| • Special population groups: |
| - Children. Babies aged less than 12 months should not be directly exposed to sunlight. |
| Use sunscreen with very high SPF values and safe organic filters on areas that are not covered by clothing. |
| - Sports and work outdoors. In addition to clothing and caps, topical sunscreen should be applied before beginning the activity and renewed often because of the effects of sweating and friction. Special care should be taken when engaging in watersports and sporting activity in mountains and snow. |
| - Patients at risk of photosensitivity. Exposure should be gradual, and photoprotective measures should be maximized. In severe cases, sunscreen should be combined with oral protective measures. |
| - Polymedicated patients. Persons receiving medication should take special care and ask about the potential risk of photosensitivity. |
| - Patients with a history of skin cancer. Minimize exposure to sunlight and integrated photoprotection. Patients should use DNA-repairing sunscreens with a very high SPF, especially patients with actinic keratosis. |
Abbreviation: AEDV, Spanish Academy of Dermatology and Venereology; SPF, sun protection factor.
In conclusion, the COVID-19 lockdown has led to an unprecedented alteration of our physiological mechanisms for adapting to sunlight. Standard photoprotective measures are of particular importance under these circumstances.
Conflicts of interestThe authors declare that they have no conflicts of interest.
AcknowledgementsThis work is part of the research of the Institute of Biomedicine of Málaga (IBIMA) and the Junta de Andalucía working group CTS-162.
Please cite this article as: Aguilera J, de Gálvez MV, Aguilera P, de Troya-Martín M, Gilaberte Y. Recomendaciones sobre exposición solar y fotoprotección del Grupo Español de Fotobiología de la AEDV adecuadas al periodo de desconfinamiento durante la pandemia por SARS-CoV-2. Actas Dermosifiliogr. 2020. https://doi.org/10.1016/j.ad.2020.06.001