Infection by the coronavirus SARS-CoV-2 and the associated disease, COVID-19, constitute a serious public health problem. Considerable uncertainty surrounds the way in which this problem will affect inflammatory diseases such as psoriasis and, in particular, patients treated with selective immunomodulators and immunosuppressants. Based on the scarce scientific evidence available and consistent with the position of other national and international scientific societies (European Academy of Dermatology and Venereology-Skin Inflammation and Psoriasis International Network, International Psoriasis Council, American Academy of Dermatology),1–3 the Psoriasis Group of the Spanish Academy of Dermatology and Venereology (AEDV) issued a statement through the AEDV (GPs-COVID-19)4 with the aim of guiding dermatologists who treat psoriasis, especially in cases where patients are receiving treatment or are about to initiate treatment with selective immunomodulators or immunosuppressants.1,2
The SARS-CoV-2 pandemic has affected, and will continue to affect, at least for some time, the management of patients with psoriasis and the functioning of specialist psoriasis clinics. Given that the situation is gradually coming under control, it is worth considering the conditions for and limitations to resuming care services in these clinics in a scenario where the virus continues to circulate, with occasional or seasonal exacerbations.
In order to minimize risk for and maximize benefits to patients and optimize the functioning of psoriasis clinics, the Psoriasis Group has developed a series of recommendations based on scientific evidence and on recommendations from other scientific societies.
In any case, whether or not these recommendations are applied will depend on scientific evidence and the progress of the pandemic.
RecommendationsPatient ManagementData available on previous and current outbreaks of coronavirus infection (severe acute respiratory syndrome, Middle East respiratory syndrome, COVID-19) enable us to suggest that the risk of severe manifestations and complications of COVID-19 is no greater in immunodepressed patients than in the general population.
The main interleukins (IL) involved in the pathogenesis of psoriasis (tumor necrosis factor [TNF] alfa, IL-17, and IL-23) have not been proven to affect the course of the viral infection, although they could be involved in the onset of the cytokine storm, which is associated with the severity of the infection. Therefore, at least in terms of pathogenesis, specific inhibition of these proteins does not seem to imply a risk with respect to the clinical course of patients taking specific immunomodulators. The impact of broad-spectrum immunomodulators (methotrexate, ciclosporin) and their inhibition is less well-known.5 Proposals for the management of patients with psoriasis are shown in Table 1.
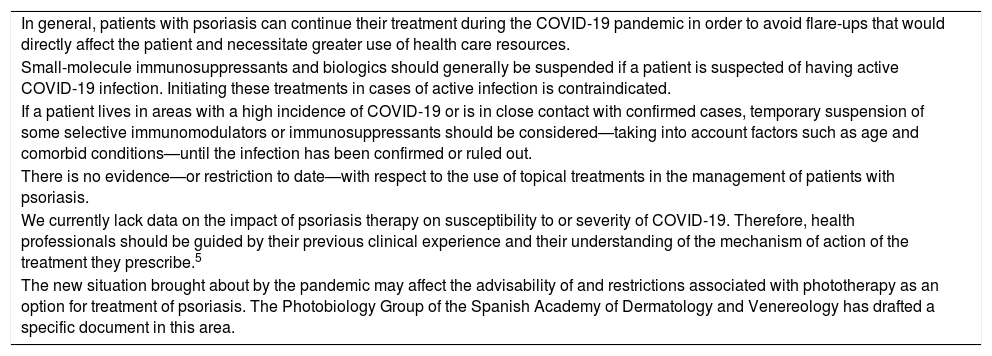
Recommendations for Patients With Psoriasis During the COVID-19 Era.
| In general, patients with psoriasis can continue their treatment during the COVID-19 pandemic in order to avoid flare-ups that would directly affect the patient and necessitate greater use of health care resources. |
| Small-molecule immunosuppressants and biologics should generally be suspended if a patient is suspected of having active COVID-19 infection. Initiating these treatments in cases of active infection is contraindicated. |
| If a patient lives in areas with a high incidence of COVID-19 or is in close contact with confirmed cases, temporary suspension of some selective immunomodulators or immunosuppressants should be considered—taking into account factors such as age and comorbid conditions—until the infection has been confirmed or ruled out. |
| There is no evidence—or restriction to date—with respect to the use of topical treatments in the management of patients with psoriasis. |
| We currently lack data on the impact of psoriasis therapy on susceptibility to or severity of COVID-19. Therefore, health professionals should be guided by their previous clinical experience and their understanding of the mechanism of action of the treatment they prescribe.5 |
| The new situation brought about by the pandemic may affect the advisability of and restrictions associated with phototherapy as an option for treatment of psoriasis. The Photobiology Group of the Spanish Academy of Dermatology and Venereology has drafted a specific document in this area. |
The conditioning factors and restrictions affecting in-person visits to the specialist psoriasis clinic will be those that are appropriate and acknowledged for any in-person visit to the dermatology clinic while the pandemic lasts (recommendations of the institutions themselves and of the AEDV).
Specialist psoriasis clinic onlineThe new situation brought about by the COVID-19 pandemic, where in-person visits are expected to be restricted, could provide an opportunity for the development and appropriate adaptation of complementary strategies (e.g., telemedicine, in the screening, management, and follow-up of psoriasis).
The activities that each unit will now address online should preferably be supervised by the professionals who see patients at the in-person visits and have appropriate knowledge and experience in the management of these patients.
An in-person approach should continue to be used, at least for the initial visits or until the skin disease is well-controlled.
Online visits could be alternated with in-person visits for the follow-up of well-managed patients whose disease is controlled with the treatment prescribed at the in-person visits.
Therefore, we believe that it would be of interest to set out the main uses of teledermatology in the specialist psoriasis clinic (Table 2).
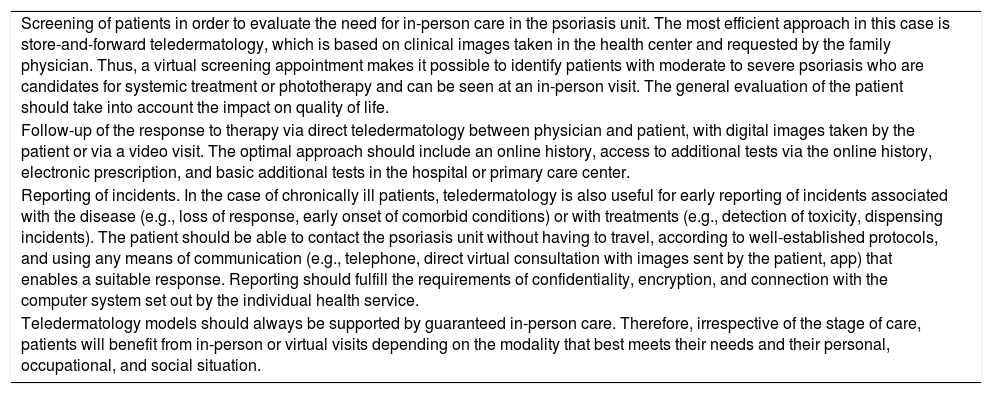
Main Uses of Teledermatology in a Specialist Psoriasis Unit.
| Screening of patients in order to evaluate the need for in-person care in the psoriasis unit. The most efficient approach in this case is store-and-forward teledermatology, which is based on clinical images taken in the health center and requested by the family physician. Thus, a virtual screening appointment makes it possible to identify patients with moderate to severe psoriasis who are candidates for systemic treatment or phototherapy and can be seen at an in-person visit. The general evaluation of the patient should take into account the impact on quality of life. |
| Follow-up of the response to therapy via direct teledermatology between physician and patient, with digital images taken by the patient or via a video visit. The optimal approach should include an online history, access to additional tests via the online history, electronic prescription, and basic additional tests in the hospital or primary care center. |
| Reporting of incidents. In the case of chronically ill patients, teledermatology is also useful for early reporting of incidents associated with the disease (e.g., loss of response, early onset of comorbid conditions) or with treatments (e.g., detection of toxicity, dispensing incidents). The patient should be able to contact the psoriasis unit without having to travel, according to well-established protocols, and using any means of communication (e.g., telephone, direct virtual consultation with images sent by the patient, app) that enables a suitable response. Reporting should fulfill the requirements of confidentiality, encryption, and connection with the computer system set out by the individual health service. |
| Teledermatology models should always be supported by guaranteed in-person care. Therefore, irrespective of the stage of care, patients will benefit from in-person or virtual visits depending on the modality that best meets their needs and their personal, occupational, and social situation. |
Dr. I. Belinchón has acted as a consultant and/or speaker for and/or has participated in clinical trials sponsored by the following companies: Janssen Pharmaceuticals Inc., Almirall SA, Lilly, AbbVie, Novartis, Celgene, Amgen, LEO Pharma, Pfizer-Wyeth, UCB, and MSD.
Dr. Ll. Puig has acted as a consultant and/or speaker for and/or has participated in clinical trials sponsored by the following companies: AbbVie, Almirall, Amgen, Baxalta, Biogen, Boehringer Ingelheim, Celgene, Gebro, Janssen, JS BIOCAD, LEO Pharma, Lilly, Merck-Serono, MSD, Mylan, Novartis, Pfizer, Regeneron, Roche, Sandoz, Samsung-Bioepis, Sanofi, and UCB.
Dr. L. Ferrándiz has acted as a consultant and/or speaker for and/or has participated in clinical trials sponsored by the following companies: Janssen Pharmaceuticals Inc., Almirall SA, Lilly, AbbVie, Novartis, Amgen, LEO Pharma, UCB, and Gebro Pharma.
Dr. P. de la Cueva has acted as a consultant and/or researcher for the following companies: AbbVie, Almirall, Astellas, Biogen, Boehringer, Celgene, Janssen, LEO Pharma, Lilly, MSD, Novartis, Pfizer, Roche, Sanofi, and UCB.
Dr. J.M. Carrascosa has acted as a consultant and/or speaker for and/or has participated in clinical trials sponsored by the following companies: Janssen Pharmaceuticals Inc., Almirall SA, Lilly, AbbVie, Novartis, Celgene, Amgen, LEO Pharma, Pfizer-Wyeth, Sandoz, Amgen, Biogen, and Mylan.
Please cite this article as: Belinchón I, Puig L, Ferrándiz L, de la Cueva P, Carrascosa JM. Recomendaciones del Grupo de Psoriasis de la AEDV sobre el manejo de la consulta de psoriasis durante la pandemia por COVID-19. Actas Dermosifiliogr. 2020. https://doi.org/10.1016/j.ad.2020.05.004