An 8-year-old girl with no relevant past history presented with asymptomatic lesions on the right axilla that had remained stable since they first appeared 2 years earlier. The patient was asymptomatic.
Physical ExaminationPhysical examination revealed several pink and brown papules arranged linearly on the floor of the right axilla (Fig. 1).
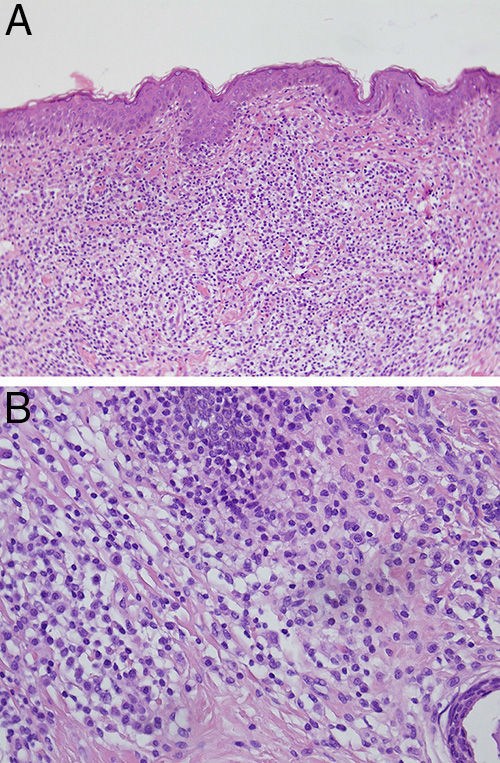
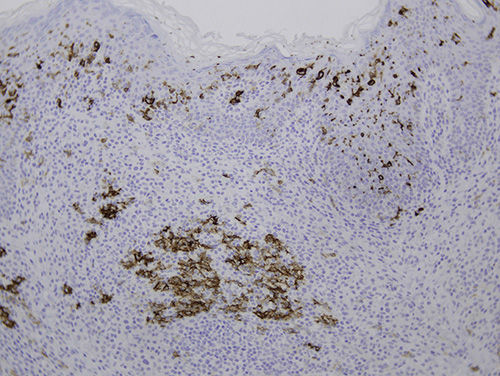
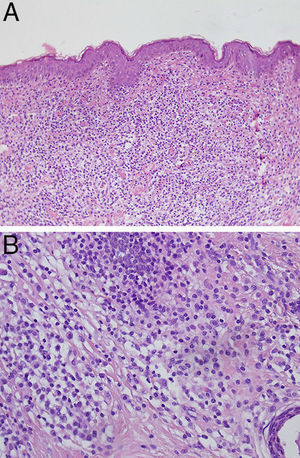
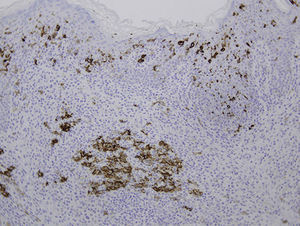
HistopathologyHistopathologic findings showed a dense dermal infiltrate composed of eosinophils, lymphocytes, and cells with abundant cytoplasm and reniform nuclei (Fig. 2), which were positive for S-100 and CD1a (Fig. 3).
The following tests were carried out: complete blood count, biochemistry profile, skeletal survey, chest radiograph, abdominal ultrasound, and full physical examination. All results were normal.
What Is Your Diagnosis?
DiagnosisUnifocal Langerhans cell histiocytosis (LCH) of the skin (cutaneous eosinophilic granuloma).
Clinical Course and TreatmentThe lesion was surgically excised and the patient has been followed up for 18 months with no local or systemic recurrence.
DiscussionLCH is characterized by an infiltrate of cells with Langerhans cell phenotype and can affect various organs, including the skin, mucosas, lymph nodes, liver, spleen, bone, digestive tract, thymus, and pituitary gland.1 According to some studies, skin lesions are present in up to 50% of patients in the initial stages of LCH and can therefore be decisive in establishing a diagnosis; however, because clinical presentation varies so widely, LCH is often not suspected.2
LCH has traditionally been classified as follows: eosinophilic granuloma (single-site disease), Hand-Schüller-Christian disease (chronic, progressive, multifocal disease), and Letterer-Siwe disease (acute, diffuse disease with a poor prognosis). In recent years, however, the Histiocyte Society has recommended classifying LCH by site and extent, as follows: type 1, unifocal; type 2, multifocal without involvement of the liver, spleen, lungs, or bone marrow; type 3, multifocal with involvement of the liver, spleen, lungs, and/or bone marrow, or age less than 2 years.
The typical, classical LCH skin lesions are described as small, purpuric, infiltrated papules with a crusted or scaly surface on the scalp, face, flexures, genital region, and trunk. However, it should be noted that a wide variety of skin lesions of various morphologies can be found in LCH,3 including the following: blisters; vesicles; pustules; single or multiple papules that can be skin-colored, pink, xanthomatous, or purpuric; tumors; nail dystrophy;4 and mucosal ulcerations.4 As a result, the differential diagnosis is very extensive and includes Darier disease, cutaneous candidiasis, non-Langerhans cell histiocytosis, intertrigo, vasculitis, urticaria pigmentosa, sarcoidosis, mycosis fungoides, impetigo, folliculitis, herpes simplex, and chickenpox.
LCH is diagnosed histologically. Skin lesions, because of their accessibility, are often the key to diagnosis. Histologic examination reveals an infiltrate of histiocytoid cells with reniform nuclei that express CD1a and S-100. Intracytoplasmic Birbeck granules are visible with electron microscopy. In the case of our patient, the late presentation of a supposed epidermal nevus at age 8 years prompted us to order the histologic study, which led us to the correct diagnosis.
Unifocal forms of LCH are usually found on bone, most frequently the cranium and long bones. Unifocal manifestation on the skin—as in the reported case—is rare. These localized cases can be treated with nitrogen mustard, psoralen–UV-A therapy, surgery, intralesional corticosteroids, radiation therapy, or thalidomide.5
Prognosis is determined by the number of organs involved and will be worse if the liver, lungs, or bone marrow are affected. Localized cutaneous forms of LCH have a good prognosis and rarely progress to multisystem disease.6
Please cite this article as: Campos-Muñoz L, Ramírez-Mora R, López-Bran E. Pápulas rosadas de distribución lineal. Actas Dermosifiliogr. 2015;106:755–756.