A 16-year-old boy with Down syndrome presented with large, asymptomatic, erythematous plaques on both lower limbs that had first appeared several months earlier.
Physical ExaminationPhysical examination revealed papules coalescing into annular plaques with hyperkeratotic borders and central depression on the anterior aspect of both thighs. The lesions left residual hyperpigmentation (Fig. 1). No other relevant lesions were found.
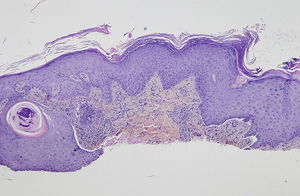
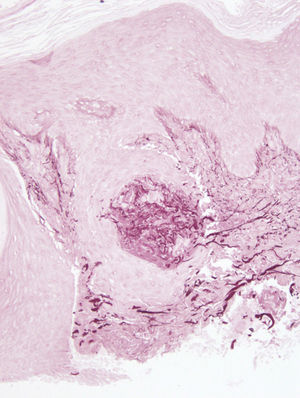
HistopathologyAnalysis of a skin biopsy specimen from the edge of a plaque revealed an acanthotic epidermis with hyperkeratosis, without the presence of intraepidermal neutrophils. Transepidermal elimination of dermal basophilic material was also observed (Fig. 2); orcein staining revealed that the material consisted of elastic fibers (Fig. 3).
What Is Your Diagnosis?
DiagnosisElastosis perforans serpiginosa.
Clinical Course and TreatmentThe patient received treatment with topical betamethasone and calcipotriol, to which the response was poor. Because the lesions were asymptomatic, we decided not to initiate more aggressive treatment.
CommentElastosis perforans serpiginosa (EPS) is a rare perforating dermatosis that usually appears in the first decades of life, normally before age 30 years, in the form of keratotic papules 2 to 5mm in diameter on the face, neck, trunk, and upper limbs with a symmetrical distribution. The lesions tend to be asymptomatic or mildly pruritic. Although EPS is classically described as affecting the head, neck, and arms, there have been reports of cases affecting the lower limbs, especially the thighs.1–3
Histologic examination of the lesions shows hyperkeratosis with or without parakeratosis, as well as the characteristic transepidermal elimination of material that can be identified by orcein staining as elastic fibers.
There are 3 types of EPS: idiopathic, reactive, and drug-induced. Reactive forms account for around 40% of cases and are associated with other diseases involving connective tissue alterations, such as Down syndrome,1,3 Ehlers-Danlos syndrome, Marfan syndrome, Rothmund-Thomson syndrome, and pseudoxanthoma elasticum.4
The fact that the incidence of connective tissue alterations such as joint hypermobility and premature skin aging is higher in patients with Down syndrome could explain why EPS lesions are more common in these patients than in the general population. Drug-induced forms of EPS are observed in approximately 1% of patients treated with D-penicillamine,5 a drug used in the treatment of Wilson disease and homocystinuria.
Many treatments have been used in EPS, with variable responses. Topical treatments such as corticosteroids,6 retinoids, and calcineurin inhibitors can be used. Various more aggressive ablative treatments have also been used, including laser therapy, cryotherapy, and tangential excision of some lesions, as well as simple destruction of the lesions by electrocautery.
We have presented a case of EPS that is atypical because of the site—the lower limbs—and because of the size of the lesions. Reports of similar cases in patients with Down syndrome lead us to believe that lesions on the lower limbs may be a common clinical presentation of EPS in this subgroup of patients.
Please cite this article as: Hernández-Ruiz E, García-Herrera A, Ferrando J. Placas eritematodescamativas en paciente con síndrome de Down. Actas Dermosifiliogr. 2015;106:753–754.