The main objective of oncologic dermatologic surgery is the complete excision of skin tumors. During reconstruction of the defect, we must attempt to preserve function and cosmetic appearance. At the labial commissure, fibers from the superior and inferior portions of the orbicularis oris muscle intersect and the vermillion inserts onto the modiolus, a complex, cone-shaped structure at the angle of the mouth. Surgical reconstruction of the labial commissure is challenging because of the need to preserve sphincter function and cosmetic symmetry. We present a number of cases of surgical defects at the labial commissure and describe the reconstruction techniques used. We also propose an algorithm to help determine the most suitable technique for different cases.
La misión principal de la cirugía dermatológica oncológica es la extirpación completa del tumor cutáneo. Tras ello se procederá a la reconstrucción del defecto intentando preservar la funcionalidad y la estética. Al nivel de las comisuras se entrecruzan las fibras del músculo orbicular de los labios superior e inferior, y el bermellón se inserta en el modiolo, una compleja estructura con forma de cono. La reconstrucción de la comisura oral supone un reto quirúrgico, ya que hemos de respetar la función esfinteriana y la simetría. Presentamos varios casos de defectos quirúrgicos situados en la comisura bucal y la solución reconstructiva por la que optamos, así como una propuesta de algoritmo reconstructivo.
The lips, which are formed of 3 layers—mucosa, muscle, and skin—have an important role as a sphincter for the mouth as the entry to the digestive apparatus, with masticatory and swallowing functions, in addition to their role in phonation.
Topographically, the lips are divided into an inferior subunit, the lower lip, and a superior subunit, further divided into 2 lateral subunits and a central subunit or filtrum. At the lateral corners of the lips there is a complex, cone-shaped structure, the modiolus, where muscle fibers from the superior and inferior fascicles of the orbicularis oris muscle interweave with fibers from extrinsic muscles (zygomaticus major and minor, buccinator, risorius, and depressor labii inferioris).1 The orbicularis oris muscle performs the sphincter function, whereas the adjacent muscles are involved in facial expression.2
In dermatologic surgery, reconstruction of defects of the commissure is always secondary to the excision of skin tumors. Reconstruction is complex, as there are few options that will maintain both the function and the cosmetic appearance of the area. In general, we should attempt to adhere to the rule of anatomical subunits, reconstructing each one completely to achieve and optimal cosmetic result.
Case DescriptionsWe present a series of cases in which the labial commissure was affected to a greater or lesser degree by the excision of cutaneous cancers in this area, and we describe the method of reconstruction employed (Table1). In the first case, the tumor was situated on the inferior vermillion border, adjacent to but not actually affecting the labial commissure. We therefore decided to perform a full-thickness wedge excision oriented inferiorly and laterally, coinciding with the melolabiomental skinfold; the defect was then sutured by tissue planes with a 4/0 polyglycolic acid suture and 4/0 silk. This is a simple surgical solution with very good functional and cosmetic results; it could be used in this case as the tumor occupied less than one third of the overall length of the lip.
In the second case the defect involved the lateral third of the lower lip and the whole commissure (Fig. 1A). Surgery left a circular defect affecting the skin and vermillion. We therefore decided to bring in similar tissue by advancing the cutaneous lip, excising 2 small triangles in the labiomental skinfold, 1 mucosal and the other cutaneous, to fit the flap (Fig. 1, B and C). Suture was performed with 4/0 silk and 4/0 polyglactin to form the new commissure. The functional and cosmetic results were highly satisfactory (Fig. 1D).
A, Partial thickness defect after 2 stages of Mohs micrographic surgery. B, After preanesthetic marking of the Klein line, essential to avoid subsequent distortion, the cutaneous lip was dissected, and the original defect was modified using an inferior triangle in order to adapt it to the lines of expression. C, Immediate postoperative appearance. D, Nine months after surgery.
Another type of advancement flap for use in the lip is the full-thickness flap, as in our third case. Slightly less than half of right side of the lower lip was excised in a full-thickness quadrangular excision, including the commissure. From its medial border, we performed a full-thickness incision in the labiomental fold to approximately 2cm lateral to the contralateral commissure. Here, a tension-releasing triangle was excised to allow the flap to be advanced to the neomodiolus. Suture was performed with 4/0 polyglycolic acid and 4/0 silk. An acceptable functional and cosmetic result was achieved, as the scars were hidden in the submental fold.
The Abbé-Estlander flap, or Estlander flap, is the same as the Abbé flap, or labial transposition flap, adapted to the area of the commissure. After excision of the tumor using a full-thickness W-shaped wedge, a triangular wedge of equal thickness and of a slightly smaller size was incised and dissected in the upper lip, preserving the orbicular artery medially in the pedicle. The flap was transposed and sutured by tissue planes (4/0 polyglycolic acid and silk) to the borders of the initial defect. The secondary defect was then closed directly by tissue planes.
Transposition flaps were used in patients 5 and 6 (Table 1). In patient 5, the partial thickness defect included the skin and subcutaneous tissue of the melolabiomental skinfold, as well as the vermillion surface of the commissures of both lips (Fig. 2, A-C). In our opinion, the best donor site was the submental skin, which also enabled us to hide the scar in the fold; we therefore chose to perform a transposition flap with an inferior base (Fig. 2, D-F). The vermillion was reconstructed using a small advancement flap of oral mucosa. The texture and color of the skin and the presence of beard hair, in the case of men, makes this region a good candidate as a donor site.
Case Series of Surgical Patients With Defects at the Labial Commissure.
| Age | Sex | Tumor | Surgery | Anesthesia | Characteristics of the Defect | Reconstruction Technique | Postoperative Complications | |
|---|---|---|---|---|---|---|---|---|
| Patient 1 | 88 | M | SCC | Conventional | L | Full-thickness, 1.5x0.8cm | Full-thickness wedge | None |
| Patient 2 | 77 | F | BCC | Mohs | L | Partial thickness, 1.2x1.5cm | Advancement of the cutaneous lip+modified direct suture | None |
| Patient 3 | 74 | F | SCC | Conventional | L | Full-thickness, 4x2cm | En bloc advancement of the lower lip | Slight microstomia, full functionality |
| Patient 4 | 90 | M | SCC | Conventional | L | Full-thickness, 5x2cm | Estlander flap | Noticeable microstomia, full functionality |
| Patient 5 | 68 | F | BCC | Conventional | L | Partial thickness, 6x4cm | Transposition flap from the chin | Surgical drainage for 48hNone |
| Patient 6 | 79 | M | BCC | Mohs | L+G | Full-thickness, 5.5x5cm | Melolabial transposition flap | Trap-door effect, asymmetry of the commissure. Full functionality |
| Patient 7 | 74 | F | SCC | Mohs | L+G | Full-thickness, 5x4cm | Double rhomboidal rotation flap | Minimum defect of oral sphincter competence, noticeable with fluids. Altered functionality not affecting vital functions |
Abbreviations: BCC, basal cell carcinoma; F, female; G, general anesthesia; L, local anesthesia/nerve block; M, male; SCC, squamous cell carcinoma.
A, Basal cell carcinoma that affected the melolabiomental skinfold and the vermillion at the labial commissure. B, Design of the transposition flap with an inferior base. C, Partial thickness skin and mucosal defect created by excision of the tumor with a surgical margin. D, Incision of the flap in the same plane and transposition. E, Suture and excision of the excess skin. The mucosa was advanced (not visible in the image) in order to reconstruct the vermillion. F, Immediate postoperative appearance.
A transposition flap with a superior base was used to close a full-thickness defect that widely surpassed the melolabiomental skinfold and exposed the alveolar tissue from the first molar to the canine, but only affected the vermillion at the commissure. Under general anesthesia, we performed a full-thickness melolabial transposition flap with an inferior vertex, transposed and fitted to the defect, suturing its superior margin to the healthy vermillion and, from there, completing the suture by tissue planes with 4/0 polyglycolic acid and 4/0 silk.3 Reconstruction of the mucosal defect was performed by advancing healthy mucosa from the lower lip, which was fixed to the mucosa of the melolabial flap with interrupted 4/0 polyglycolic acid sutures.
Finally, a double rhomboidal flap was used for reconstruction in the seventh patient. In this case, a large round defect was created that affected the mucosa, muscle, and skin and exposed part of the upper and lower dental arches (Fig. 3A). This defect compromised overall sphincteric function by completely destroying the commissure and the lateral third of the orbicularis oris muscle. We performed a partial thickness double rhomboidal flap, superiorly from the melolabial region and inferiorly from the area of the chin, and bilateral advancement of the mucosa to reconstruct the superior and inferior vermillion (Fig. 3, B and C). The mucosal defect was small compared with the myocutaneous defect, and it could therefore be reconstructed with a bilateral advancement flap from the upper and lower oral mucosa. Excessive cicatricial tissue retraction occurred in our patient, leading to slight failure of oral competence, though this did not interfere with basic functions (Fig. 3D).
A, Full-thickness defect after Mohs micrographic surgery. Design of a double rhomboidal flap. B, Incision of both flaps in the subcutaneous plane. C, Immediate postoperative appearance; it can be seen that the mucosal advancement was insufficient. D, Twenty-four months after surgery. Mild labial incompetence.
The fundamental objectives during reconstruction of the labial commissure are maintenance of function and, secondarily, the preservation of local symmetry and cosmetic appearance. Knowledge of the anatomy of the lip and, in particular, of the modiolus and of the muscles that insert at this site, will ensure an adequate reconstruction technique. In addition, detailed presurgical examination of the defect and of the adjacent subunits is essential. The thickness of the defect, its orientation, elasticity of the tissues, and loss of function are the main factors that will determine the best individual reconstruction option in each case. However, age, comorbid conditions, and the cosmetic expectations of the patient must be taken into account.
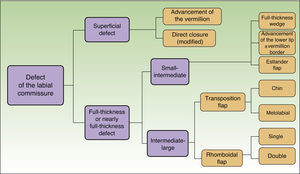
Based on the cases presented, we propose a reconstruction algorithm for defects that affect the labial commissure, depending on the thickness and size of the defect (Fig. 4).
It should be noted that, regarding en bloc advancement flaps of the lower lip, it is important to use careful blunt dissection so as not to damage the mental nerve, the branch of the maxillary nerve that emerges through the foramen of the same name to innervate the lower lip and chin. This flap is very useful and is simple to perform; it carries a minimal morbidity and mortality and a low risk of microstomia. Many authors have demonstrated its suitability for use in defects of the labial commissure and in defects that involve up to two thirds of the overall length of the lower lip.4
The Estlander flap is a well-vascularized flap thanks to the superior labial artery,5 which supplies both the cutaneous lip and the vermillion. The main disadvantage of this flap is microstomia and disappearance of the labial commissure, though this can be reconstructed in a second operation.
Nasolabial flaps with an inferior base receive their blood supply from the facial artery or its main branches, whereas those with a superior base are supplied by the infraorbital or transverse facial arteries.6 Numerous authors have proposed the use of Z-plasties at the flap donor site in order to avoid secondary contractures,7,8 but this was not necessary in our patients as the submental fold was not crossed.
The rhomboidal flap can be used to repair large defects in a single operation, as it provides ample tissue and can thus reduce tension in the scar.9 However, it does not ensure complete sphincteric competence as it does not substitute the orbicularis oris muscle at the labial commissure.
In conclusion, we would like to draw attention to 2 fundamental points in the reconstruction of the labial commissure: the need for good anatomical knowledge of the area when designing options for reconstruction that maintain adequate oral sphincter function, and the need for presurgical examination to find the most suitable donor area.
The aim of our proposed treatment algorithm is to provide the dermatologic surgeon with a clear plan, with an eminently practical approach that will prove useful in daily surgical practice.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this research.
Confidentiality of dataThe authors declare that they followed their hospital's regulations regarding the publication of patient information.
Right to privacy and informed consentThe authors obtained informed consent from the patients and/or subjects referred to in this article. This document is held by the corresponding author.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Otero-Rivas MM, Alonso-Alonso T, Pérez-Bustillo A, Rodríguez-Prieto MÁ. Reconstrucción de defectos quirúrgicos en la comisura oral. Actas Dermosifiliogr. 2015;106:e49–e54.