A 77-year-old man with a history of high blood pressure and ischemic heart disease was seen for a tumor located in the upper third of the back (Fig. 1).
Physical ExaminationPhysical examination revealed a tumor (1.2cm in diameter) consisting of 2 well-differentiated elements: a tumor nodule with a pearly sheen and telangiectasias; and a dark brown pigmented macule. Dermoscopy showed arborescent telangiectasias, gray-brown globules, and crystalline structures in the nodule, and an atypical reticular pattern with thick lines in the macule (Fig. 2). The lesion was situated on intensely photodamaged skin, on which solar lentigines, actinic keratoses, and solar elastosis were evident. The clinical differential diagnosis included basal cell carcinoma (BCC) and melanoma. The lesion was resected.
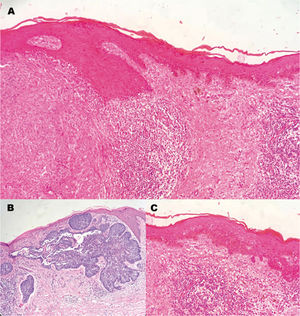
HistopathologyHistopathology revealed 2 contiguous, non-overlapping lesions (Fig. 3A).
The first was a basophilic dermal tumor lesion continuous with the epithelium, compromising the upper dermis, consisting of nodular nests of cells with a high nucleus to cytoplasm ratio, forming peripheral palisades and retraction clefts in the stroma (Fig. 3B).
The second was an atypical, intraepidermal, irregular melanocytic lesion, with melanocytes grouped into thecae of varying sizes. Anisocytosis and anisokaryosis, large hyperchromatic nuclei, and irregularly distributed melanin pigment were also observed. In addition, isolated melanocytes had migrated into the upper layers of the epidermis. Neither atypical mitoses nor skin invasion were observed (Fig. 3C).
What is Your Diagnosis?
DiagnosisCollision tumor consisting of a nodular BCC and a lentigo maligna (LM).
Clinical Course and TreatmentResection margins were extended to 5mm, and no residual tumor was detected in the analyzed sample.
CommentsBCC can coexist with other skin lesions, but collision of BCC with melanoma is rare. BCC most commonly co-occurs with benign melanocytic lesions, seborrheic keratosis, and neurofibroma, and a few cases of BCC colliding with melanoma have been reported.1
LM melanoma and BCC are 2 distinct tumors that classically develop in the elderly and on sun-exposed skin. Since the formation of both tumors is promoted by changes caused by sun damage, their development in the same site, although unusual, can be easily explained.2
Dermoscopic diagnosis of BCC is based on specific, well-described criteria. These include arborescent vessels, superficial fine telangiectasias, blue-gray nests, blue-gray dots and globules, focused dots, maple leaf-like areas, cart wheel structures, concentric structures, ulceration, multiple small erosions, bright red unstructured areas, and whitish structures.3 In our patient we observed thick arborescent telangiectasias and gray-brown globules.
LM manifests as a slow-growing pigmented macule in areas of chronic sun exposure, as in the present case. It is characterized by morphological asymmetry and pigmentation. Dermoscopy of extrafacial LM reveals superficial spreading melanoma patterns, including asymmetric structures, dots/globules, and pseudopods, combined with LM dermoscopic findings such as rhomboid structures and asymmetric perifollicular pigmentation.4
Treatment of mixed tumors is carried out according to the guidelines recommended for individual tumors, depending on which tumor has the worst prognosis.5
Conflicts of InterestThe authors declare that they have no conflicts of interest.