Current surgical techniques for the treatment of morbid obesity can lead to major systemic complications. Biliopancreatic bypass surgery is a mixed restrictive-malabsorptive type of bariatric surgery that combines partial gastrectomy with a gastroileal anastomosis, causing the bile and pancreatic secretions to mix with the foods only in the final 50cm of the small bowel. In the long term, this considerably reduces the absorption of vitamins, oligoelements, and essential fatty acids.
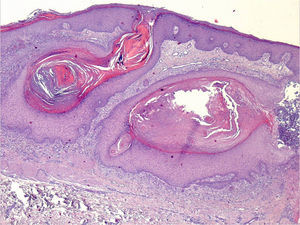
Our patient was a man of 46 years of age, with a history of obesity, hypertension, tuberculous lymphadenitis in 2005, a biliopancreatic bypass operation in 1999, and operations for an anal fistula and to perform dermolipectomy in the hypogastrium and flanks. He was on treatment with valsartan, venotonic agents, ferrous sulfate, and Dayamineral (a vitamin and mineral supplement). He was seen in dermatology in 2012 for suppurating lesions on the lower limbs. The lesions had appeared when he started to lose weight after the bariatric surgery and they had gradually spread to the trunk and upper limbs. The diagnoses from 2 skin biopsies performed in 2003 were folliculitis and furuncle, respectively. Cultures for bacteria, fungi, and mycobacteria were repeatedly negative and various oral antibiotic treatments did not resolve the condition. On physical examination there were violaceous papular and tuberose lesions, some with scabs, situated mainly on the thighs and on the medial aspect of the knees, but with isolated lesions on the abdomen and on the proximal areas of the upper limbs (Fig. 1A). Histopathology revealed the presence of intense hyperkeratosis in the pilosebaceous follicles, giving rise to the formation of keratin cysts. There was also a small abscess with residues of fragmented collagen and the presence of macrophages and neutrophils (Fig. 2). No fragmentation of elastic fibers was detected. Special techniques did not reveal the presence of fungi or of mycobacteria. A provisional diagnosis of phrynoderma was made based on these findings. Blood tests confirmed the deficit of vitamin A (0.15mg/L [normal range, 0.30-1mg/L]), as well as of vitamin E (4.9μg/mL [normal range, 5-20μg/mL]), Vitamin D3 (14.18ng/mL [normal range, 20-32ng/mL]), and zinc (43μg/dL), as well as a low hemoglobin level (11.4g/dL) and low hematocrit 34%. Oral treatment was therefore prescribed as follows: vitamin A (1000IU/d); vitamin E (20mg/d); calcifediol (1 ampoule of 3mg/1.5mL per week); Hidroxil-B12-B6-B1; Dayamineral, 1 tablet once a day; ferrous iron (80mg/d); and oil rich in medium-chain triglycerides. After 7 months of treatment the skin lesions had not improved and the serum levels of vitamin A (0.11mg/L) and vitamin E (5.1μg/mL), Zn (52μg/dL), the hemoglobin level (11.0g/dL), and the hematocrit 33% were still low. Intravenous iron (500mg of iron), intramuscular vitamin A (100 000IU/mo) and zinc sulfate (22.5mg/d) were therefore added to the patient's treatment. Three months later the vitamin levels were normal (vitamin A, 0.38mg/L), the anemia had resolved, and only residual areas of hyperpigmentation were present on the skin (Fig. 1B).
Phrynoderma is the characteristic dermatosis associated with a deficiency of vitamin A, a fat-soluble vitamin involved in numerous body functions. Although this vitamin deficiency is common in Africa and southeast Asia, phrynoderma is rare in Spain, where it is associated with malabsorptive states, such as pancreatic insufficiency, colectomy, and chronic giardiasis, or arises as a complication of bariatric surgery.1
Vitamin A deficiency is very common among patients who have undergone bariatric surgery and it has been associated with low prealbumin levels, leading to a suggestion to use vitamin A levels as a marker of protein-energy malnutrition in these patients.2
Phrynoderma is characterized by the presence of follicular hyperkeratosis, mainly affecting the extensor surfaces of the limbs, the abdomen, and back. It is often associated with xerosis and hyperpigmentation, as well as extracutaneous manifestations such as night blindness. The majority of reports of phrynoderma secondary to biliopancreatic bypass surgery describe atypical lesions that are larger and more inflammatory and tend to arise in atypical sites, as occurred in our patient.3 Deficits of many other essential oligoelements and vitamins observed in these patients may contribute to this atypical presentation, particularly if we consider that phrynoderma does not appear to have a single etiology.1 For example, furunculosis has been described in association with iron deficiency and has improved after restoring normal iron levels4; this diagnosis had to be considered in our patient as the first biopsies were compatible with this skin disorder.
From a clinical point of view, the differential diagnosis must include other skin conditions that have been described in association with bariatric surgery, such as dermatosis-arthritis syndrome, neutrophilic dermatosis attributed to the formation of circulating immune complexes produced in the blind loop of bowel,5 and acrodermatitis related to zinc deficiency.6 We also considered the perforating dermatoses, although no association with bariatric surgery has been reported.
The increase in obesity in western society means that bariatric surgery will become more common. The conclusion from the present case is that patients undergoing bariatric surgery must be followed up closely by a multidisciplinary team that is aware of the nutritional risks and complications, as well as the appropriate therapeutic strategies that patients must follow for life.
Please cite this article as: Abad L, Omiste T, Vera J, Gilaberte Y. Frinoderma asociado a derivación biliopancreática. Actas Dermosifiliogr. 2015;106:327–329.