Ustekinumab is a human monoclonal antibody directed against interleukins (IL) 12 and 23, which are involved in the control of infections and tumors and the pathogenesis of psoriasis. Animal model studies have shown that inhibition of IL-12 and IL-23 might promote carcinogenesis.1
Biologic therapies are considered to be both safe and well tolerated, but there is concern about their carcinogenic potential. There have been several reports of lymphoproliferative disorders developing in patients under treatment with tumor necrosis factor (TNF) inhibitors.2–4 We present the case of a 68-year-old man with a history of hypertension, type 2 diabetes mellitus, hypertriglyceridemia, overweight, and ischemic heart disease diagnosed with plaque psoriasis 13 years earlier. Given the severity of his psoriasis, the patient was administered psoralen plus UV-A therapy and methotrexate 15mg/wk for a year; the treatment showed moderate effectiveness, and rapid recurrence was observed following discontinuation of treatment. In May 2008, the patient was started on concomitant efalizumab and methotrexate (7.5mg/wk) therapy, which was continued with satisfactory results until efalizumab was withdrawn from the market in 2009. In March 2010, the patient experienced a relapse and was administered ustekinumab, which achieved adequate control of his psoriasis.
In November 2012, the patient was seen at the emergency department of our hospital with complaints of melena and upper abdominal pain. A gastroscopy revealed a gastric tumor with signs of malignancy. The tumor, however, was studied and monitored at another hospital “resultando infructuoso el intento de recuperar las muestras histologicas”. The results showed a dense infiltrate composed of atypical lymphocytes without identifiable clusters of nodes. In the immunohistochemical study, the cells were positive for CD20 and BCL2, and negative for CD10, CD30, cyclin D1, and CD5. The use of appropriate histological stains did not identify Helicobacter pylori or other microorganisms. A diagnosis of low-grade gastric mucosa-associated lymphoid tissue (MALT) lymphoma was established, with no metastases identified by positron electron tomography/computed tomography. The patient underwent 19 sessions of radiation therapy, which resulted in complete remission according to a report dated April 2013, which is when he came for a follow-up visit at our hospital. On examination of this and other reports on the tumor, it was decided to discontinue treatment with ustekinumab. The patient's psoriasis, however, was kept under control with topical treatment, which resulted in almost complete whitening of the lesions. Nevertheless, in August 2013, the patient died suddenly of cerebral infarction.
The risk of malignancy in patients with psoriasis is a hotly debated topic. Some authors have postulated that the risk might be higher than in the general population, even in the absence of treatment, due to the underlying chronic inflammation associated with psoriasis, particularly in patients with comorbidities.5
There is also controversy surrounding the risk of lymphomas in patients with psoriasis. It has been postulated that this potentially increased risk might be related to both the pathophysiology of psoriasis and the use of immunosuppressant therapy in this setting.6
There have been isolated reports of lymphomas developing in patients treated with a biologic,3 and even of regression following withdrawal of the drug, pointing to a possible causal relationship.4
The development of lymphomas in patients treated with ustekinumab is rare. Data from landmark trials and a recent study of the safety of ustekinumab in psoriasis over a 5-year follow-up period showed that the risk of malignancy per 9000 patient-years was similar to that seen in the general population, with just 1 patient presenting a possible Hodgkin lymphoma.7
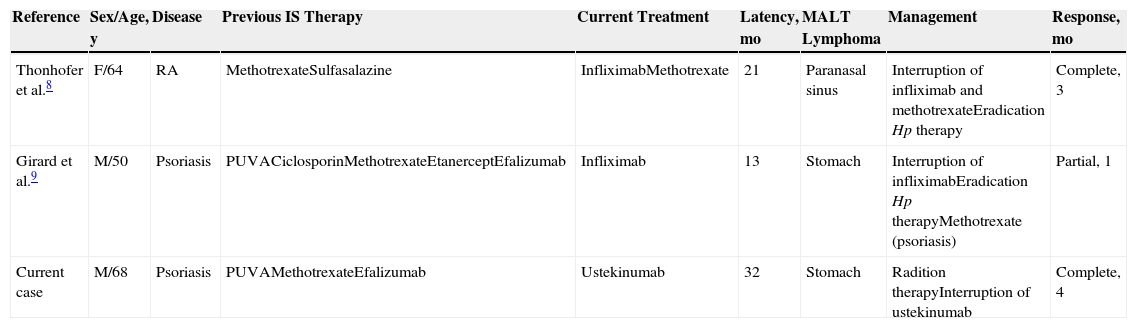
In our review of the literature, we found just 2 cases of MALT lymphoma that developed during infliximab therapy.8,9 Both patients had H pylori infection. Lymphoma remission was observed in the 2 cases following interruption of the biologic and administration of H pylori eradication therapy (Table 1). The authors of both reports speculated that the TNF inhibitor might have acted by promoting H pylori infection and/or by directly inducing the lymphoproliferative process. They also did not rule out that previous immunosuppressant therapy or the patients’ underlying diseases may have had a carcinogenic role.
Mucosa-Associated Lymphoid Tissue (MALT) Lymphoma in Patients Receiving Biologic Therapy.
| Reference | Sex/Age, y | Disease | Previous IS Therapy | Current Treatment | Latency, mo | MALT Lymphoma | Management | Response, mo |
|---|---|---|---|---|---|---|---|---|
| Thonhofer et al.8 | F/64 | RA | MethotrexateSulfasalazine | InfliximabMethotrexate | 21 | Paranasal sinus | Interruption of infliximab and methotrexateEradication Hp therapy | Complete, 3 |
| Girard et al.9 | M/50 | Psoriasis | PUVACiclosporinMethotrexateEtanerceptEfalizumab | Infliximab | 13 | Stomach | Interruption of infliximabEradication Hp therapyMethotrexate (psoriasis) | Partial, 1 |
| Current case | M/68 | Psoriasis | PUVAMethotrexateEfalizumab | Ustekinumab | 32 | Stomach | Radition therapyInterruption of ustekinumab | Complete, 4 |
Abbreviations: F, female; Hp, Helicobacter pylori; IS, immunosuppressant; M, male; PUVA, psoralen plus UV-A therapy; RA, rheumatoid arthritis.
MALT lymphoma is a B-cell non-Hodgkin lymphoma. It is usually low-grade and located in the gastrointestinal tract. Ninety percent of patients with gastric MALT lymphoma have concomitant H pylori infection. H pylori eradication therapy achieves remission in 80% of low-grade lymphomas and in just 50% of high-grade lymphomas. This remission is maintained for many years following the eradication of infection. Recurrence, however, is observed in 10% of cases, hence the need for lifetime endoscopic follow-up. Radiation therapy is the next best option for patients who do not respond to eradication therapy.10
In conclusion, we have presented the third case of a patient who developed gastric MALT lymphoma during biologic therapy and the first case involving a patient treated with ustekinumab.8,9 We cannot, however, rule out that the lymphoma may have been triggered by the patient's chronic inflammatory state induced by psoriasis, or by previous use of immunosuppressant therapy. It is, of course, also possible that the association was merely coincidential. We stress the importance of treatment discontinuation in patients like ours who develop a lymphoma during biologic therapy.
Please cite this article as: González-Ramos J, Alonso-Pacheco M, Mayor-Ibarguren A, Herranz-Pinto P. Linfoma gástrico de tejido linfoide asociado a mucosa en un paciente con psoriasis grave en tratamiento con ustekinumab. Actas Dermosifiliogr. 2015;106:326–327.