A 23-year-old woman consulted for the gradual appearance of painful lesions on the external aspect of the thighs. The lesions had first appeared 5 weeks earlier. The patient reported similar flare-ups over 3 consecutive years; these appeared during the coldest months of the year and resolved without scarring as the seasonal temperature increased. No other manifestations were observed. The patient was a horseback rider and rode and cared for horses on a daily basis.
Physical ExaminationThe examination revealed erythematous-violaceous lesions that were painful to the touch and tended to coalesce and form plaques on the outer part of the upper thigh (both legs) (Fig. 1). Erythematous-violaceous reticulated macules with a vascular appearance were observed on the rest of the thigh. The local temperature was lower in the affected areas.
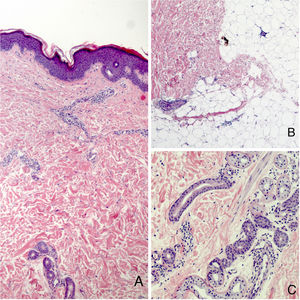
HistopathologyThe histopathology workup (Fig. 2A) revealed a perivascular and periadnexal dermal lymphocytic infiltrate beneath a normal epidermis (Fig. 2C), as well as venulitis in the deep reticular dermis and hypodermis (Fig. 2B). No signs of panniculitis were observed. Alcian-blue staining did not reveal mucin deposits.
Additional TestsThe results of the laboratory work-up were normal (negative for autoimmunity, cold agglutinins, cryoglobulins, and serology). Capillaroscopy performed on the hands revealed normal findings, as did Doppler ultrasound of the lower limbs.
What is Your Diagnosis?DiagnosisCold-associated perniosis of the thighs (CAPT).
Course and TreatmentThe patient was recommended to wear looser clothing and prescribed medium-potency topical corticosteroids. The lesions had improved at the 1-month check-up.
CommentCAPT is the term proposed in 2016 by Ferrara and Cerroni1 to describe a condition for which no consensus had been reached and that had been reported with various names: equestrian panniculitis, equestrian-type perniosis, or equestrian-type chilblains. Diagnosis is based on previous exposure to cold, cutaneous lesions on the side of the thighs, and a compatible history.
The usual clinical picture of CAPT does not differ significantly from that originally described in 1980 by Beacham et al.2 under the name of equestrian cold panniculitis. It is characterized by the presence of infiltrated erythematous-violaceous plaques that may be pruritic or painful. The plaques are found mainly on the outer part of the upper thigh and are not accompanied by other abnormalities.
The term equestrian was replaced by cold-associated. Other causes have been identified, for example, riding a bicycle, occupational exposure to humid environments, toboganning,3 wearing jeans with a low waistband,4 and application of icepacks.5
The term perniosis is now preferred to panniculitis because signs of panniculitis were not observed in many of the cases analyzed. The most common finding is a perivascular and periadnexal lymphocytic infiltrate in the superficial and deep dermis. Other findings include mucin deposits in the dermis and inflammation of small- and medium-caliber venules. Some cases also present lymphocytic lobular panniculitis, which is probably an advanced stage of deep venulitis. Histology makes it possible to differentiate the condition from other conditions in which cold leads to necrosis of hypodermal fat, such as Haxthausen disease or panniculitis caused by sucking ice cream; the term cold-induced panniculitis should be reserved for these conditions.1,6 Furthermore, cases of cold-induced dermatosis have been reported in horseback riders or persons who have applied cold locally in order to treat low back pain. This can take the form of panniculitis and chilblains (perniosis), which, in histologic terms, resemble lupus.7
The outer part of the upper thigh is the most common location, for several reasons. The area is more exposed to cold, thus leading to vasoconstriction and increased blood viscosity. In addition, it is exposed to tight clothes that place continuous pressure on the area and reduce blood flow in the subcutaneous fat. Moreover, the area is characterized by abundant adipose tissue, which isolates blood vessels and makes them more susceptible to the effects of cold.8
Treatment is based on recommending loose clothing. Topical corticosteroids can also be applied. Vasodilators are not useful.9 The condition usually resolves without scarring after a few weeks.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Conejero R, Rivera-Rodríguez Á, Ara M. Nódulos dolorosos en muslos. Actas Dermosifiliogr. 2021;112:357–358.