A 58-year-old woman with a history of chronic obstructive pulmonary disease presented with cutaneous lesions that had appeared on both legs and knees over the previous 7 days. The leg lesions were painful, but those on her knees were asymptomatic and had only come to her attention while she was examining the other lesions. She reported no trauma to the area or subcutaneous injections. There were no digestive or respiratory symptoms, fever, or joint pain. The physical examination showed 15 to 20 erythematous nodules measuring 20 to 40mm on both legs and knees; the lesions were largely located on the anterior aspects (Fig. 1). The lesions on the knees were flat, linearly arranged, red-orange papules measuring 2 to 3mm.
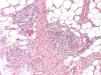
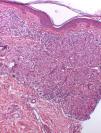
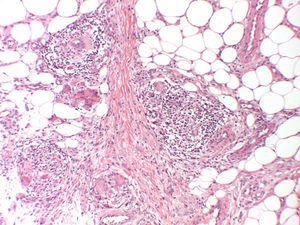
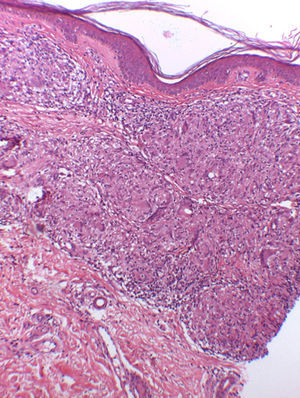
HistopathologyHistologic examination showed an inflammatory infiltrate of histiocytes in the hypodermis for one of the nodules (Fig. 2) and granulomas in the dermis for one of the papules (Fig. 3). Ziehl-Neelsen staining was negative in both cases.
Additional TestsNormal results were obtained for complete blood count, liver function, angiotensin converting enzyme, C reactive protein, and erythrocyte sedimentation rate. Cultures for bacteria, mycobacteria, and fungi were negative for both lesions, as was the Mantoux tuberculin skin test. The chest radiograph showed findings consistent with the patient's underlying lung disease. The eye study was normal.
What Is Your Diagnosis?
DiagnosisSarcoidosis: papular sarcoidosis of the knees and erythema nodosum (EN).
Clinical Course and TreatmentThe patient was prescribed ibuprofen 600mg/8h and rest with leg elevation. The knee and leg lesions resolved within 8 weeks. No involvement of other organs was observed in a year of clinical follow-up.
CommentThe cutaneous manifestations of sarcoidosis are classified as nonspecific (e.g., EN), or specific (granulomatous).1 Papular sarcoidosis of the knees is considered to be an intermediate form of papular sarcoidosis and scar sarcoidosis.2 It consists of small brownish-red papules on both knees that are frequently arranged linearly and have a lichenoid appearance.2 Histology shows noncaseating granulomas with scarce lymphocytes in the papillary dermis, and on occasions, the hypodermis.2,3 The differential diagnosis should include other entities with noncaseating granulomas, i.e., certain types of tuberculosis (with positive Ziehl-Neelsen staining), tuberculoid leprosy (with nerve involvement), Crohn disease (diffuse, with perivascular lymphocytic cuffing and frequent eosinophils and ulceration), and foreign body granuloma. Foreign material is frequently detected under polarized light microscopy,2 but this does not rule out a diagnosis of sarcoidoisis.2,4 This material was not observed in our case. In papular sarcoidosis of the knees, the presence of linear papules together with the absence of a histologic scar and history of trauma suggests that the granulomas could be the result of a reaction to foreign bodies following a small penetrating injury rather than a scar tissue reaction.2
When viewed under low magnification, EN can be confused with other entities that predominantly affect the adipose septa, namely, leukocytoclastic vasculitis (characterized by venules with fibrinoid necrosis, neutrophils within vessel walls, and nuclear dust), superficial thrombophlebitis (inflammation around a thrombosed vein, without involvement of the fat lobules), and polyarteritis nodosum (involvement of muscle arteries, also in the dermis). Marcoval et al.4 found EN in 11 of 13 patients with papular sarcoidosis of the knees and considered this coexistence to be a key factor for distinguishing this variant of sarcoidosis from other conditions associated with EN. The 13 cases of papular sarcoidosis reported by Marcoval et al.4 and the case reported by Choi et al.15 were all systemic, unlike our case. Papular sarcoidosis of the knees can also occur in association with nodules other than EN nodules, as demonstrated by the case reported by Kondo and Nishii3 in which a patient, diagnosed with subcutaneous sarcoidosis, developed clinically different lesions under several plaques. Maculopapular lesions tend to be associated with acute forms of sarcoidosis,6 and papular sarcoidosis of the knees also appears to be more common in these acute forms, which are associated with a better prognosis.2,3,5
We have described a new case of papular sarcoidosis of the knees and EN with, to date, exclusive cutaneous involvement, providing further support of the good prognosis associated with this condition. Nevertheless, it is advisable to monitor patients to check for future outbreaks and the involvement of other organs.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Lozano-Masdemont B, Gómez-Recuero-Muñoz L, Baniandrés-Rodríguez O. Nódulos y pápulas eritematosas en piernas y rodillas. Actas Dermosifiliogr. 2016;107:423–424.