Dermatofibroma is the most common fibrohistiocytic tumor of the skin and one of the benign neoplasias that generates most visits to the dermatologist. It usually presents as an isolated lesion and rarely occurs as multiple lesions. The term multiple dermatofibroma is defined either as the appearance of at least 15 dermatofibromas within a few months1 or, more recently, as 5 to 8 dermatofibromas in 4 months.2 In 1984, Dupré et al3 described another form of presentation that is far less common: multiple clustered dermatofibromas. We report a new case of this rare condition. A 25-year-old woman was seen in our department for small, erythematous papular lesions, with a dark center and paler borders, and asymptomatic, residual hyperpigmented macules in smaller numbers, all located on the medial surface of the right thigh. The lesions had appeared at 1 year of age, increased in number and size over 2 to 3 months, and subsequently remained stable except for partial remission of isolated lesions (Fig. 1). The patient reported no general or local history of interest. She brought a magnetic resonance imaging scan that had been performed previously to rule out lymphangioma and that showed no atrophy of the adipose tissue or muscle, and no other relevant alterations.
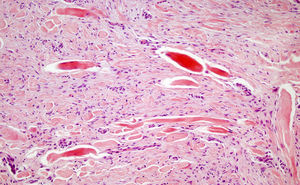
Biopsy of a lesion revealed epidermal hyperplasia and a proliferation of spindle cells arranged in fascicles or whorls interspersed in bundles of thickened collagen in the underlying reticular dermis (Fig. 2). Immunohistochemistry showed an intense, diffuse expression of vimentin and factor XIIIa. Smooth muscle actin, muscle-specific actin, and CD34 were negative. After histopathological confirmation of the diagnosis of dermatofibroma, it was decided to follow up the patient but to apply no treatment.
We have found 13 cases of multiple clustered dermatofibromas described in the literature, the majority of which were reported in the review by Gershtenson.4 There is no clinical, histological, or phenotypic differentiation between the individual lesions of multiple clustered dermatofibroma and isolated dermatofibroma lesions. No local triggering factors have been described and, unlike multiple dermatofibromas, no association has been found with states of immunosuppression or other comorbid conditions. Only on 1 occasion did the lesions arise over a thrombosed superficial vein in a patient who had undergone kidney transplantation 1 month earlier. In most of the articles published the lesions had appeared on lower limbs, as was the case in our patient. Apart from our case and 1 case of congenital lesions,5 the dermatofibromas developed in patients up to 30 years of age. A benign course was reported for all patients and no malignant change or secondary metastases have been described to date. Berbis6 reports a case followed for 20 years without complications. We believe it is important to bear this in mind for the management and follow-up of this condition.
In our patient, the symptoms, distribution of the lesions, and histopathology were identical to those previously described in the literature, although the onset of the condition at an early age is noteworthy.
In conclusion, we highlight the atypical presentation of multiple clustered dermatofibromas, a subgroup of a very common condition as is dermatofibroma, and its benign course in all the cases described to date.
Please cite this article as: Castellanos-González M, et al. Lo común a veces puede ser atípico: dermatofibromas múltiples agrupados. Actas Dermosifiliogr.2011;102:467-479.