Calciphylaxis is characterized by calcification of the media of the small arteries and arterioles of the skin, provoking cutaneous ischemia. It affects patients with end-stage renal disease (ESRD) on hemodialysis and carries a high morbidity and mortality, with death most commonly due to sepsis.1 We describe the case of a patient with calciphylaxis treated successfully with multimodal therapy including sodium thiosulfate (ST) and prostaglandins.
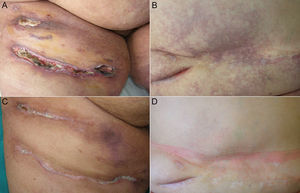
The patient was a 51-year-old woman on hemodialysis for ESRD secondary to polycystic kidney disease. She consulted for ulcers that had appeared on her abdomen and right thigh more than a year earlier; the ulcers produced intense pain refractory to opioid analgesia. Physical examination revealed deep, foul-smelling skin ulcers up to 10cm in diameter on the anterior surface of the thighs and lower abdomen, with areas of superficial necrotic eschar. The ulcers were situated in extensive areas of livedo racemosa and retiform purpura (Fig. 1, A and B). Important findings in the blood tests were secondary hyperparathyroidism with parathormone levels of 895.8pg/mL (normal range, 15-65mg/mL), calcium 9.4mg/dL (normal range, 8.2-10.3mg/dL), and phosphorus, 5.8mg/dL (normal range, 2.7-4.5mg/dL). Further additional tests to exclude other causes of livedo racemosa, including antinuclear antibodies, antineutrophil cytoplasmic antibodies with antimyeloperoxidase and antiproteinase-3 activity, cryoglobulins, anticardiolipin antibodies, and anticitrullinated peptide antibodies, were normal or negative. Skin biopsy showed calcification of the media of vessels in the subcutaneous cellular tissue with focal calcium deposits in subdermal lobules, confirming the diagnosis of calciphylaxis.
A, Calciphylaxis-related skin ulcers on the anterior aspect of the thighs. B, Livedo racemosa and retiform purpura on the abdomen. C, Healing of the ulcers on the anterior aspect of the thighs after combined treatment with intravenous sodium thiosulfate and alprostadil. D, Disappearance of the livedo racemosa and retiform purpura on the abdomen.
The patient was treated with intravenous (IV) ST, 25mg, administered immediately after each hemodialysis session, with no clinical response. She was receiving 3 hemodialysis sessions per week. Nausea was the only adverse effect. After 36 sessions of IV ST with no clinical response, we added treatment with IV alprostadil, 60μg, administered during each hemodialysis session. From the first infusion of alprostadil, the patient reported rapid pain relief that enabled the opioids to be withdrawn. With this combination, the skin ulcers and livedo racemosa improved progressively. In order to accelerate healing of the skin ulcers and to reduce the risk of infection, we added treatment with monthly intralesional infiltrations of 10mL of ST solution, 1/6M, around the borders of the ulcers, without previous anesthesia, and hyperbaric oxygen therapy for 3 months. Hyperbaric oxygen therapy was performed on Monday to Friday each week, with a duration of 60min per session, at an absolute pressure to 2.4 atmospheres, with a total of 70 sessions. After 5 months of treatment, all the skin ulcers and the livedo racemosa had resolved (Fig. 1, C and D). For more than a year, the patient has continued on maintenance treatment with IV alprostadil during the hemodialysis sessions combined with IV ST after each session and occasional ST infiltrations when small ulcers develop. This multimodal therapy has achieved good overall control of this severe disease more than 2 years after its onset.
The medical treatments most widely used for calciphylaxis are IV ST and the bisphosphonates.2 ST has a vasodilator effect that reduces pain and is a chelator of calcium salts, making them more soluble.3 Alprostadil, or prostaglandin E1, is well known for its vasodilator effect and antiplatelet and fibrinolytic activity.4 There are no reports in the scientific literature of any case of calciphylaxis successfully treated with the combination of IV and intralesional ST and IV alprostadil. Miceli et al.5 described the combination of IV ST and prostaglandin E1 in a patient with calciphylaxis associated with a marked deterioration in the patient's general state of health; despite treatment, the patient showed further deterioration and died. Alikadic et al.6 reported the use of a prostacyclin analog, iloprost, in combination with hyperbaric chamber treatment and autologous skin cell culture for the treatment of calciphylaxis, achieving a good response. Horishita et al.7 described the use of alprostadil to prevent a fall in peripheral blood flow to damaged tissues during general anesthesia in a patient with calciphylaxis, but not as a treatment for this disease. Alprostadil has also been effective in other obstructive alterations of the cutaneous microcirculation, such as livedoid vasculopathy.4
In our patient, IV ST was ineffective until IV alprostadil was added; this led to a rapid improvement in the pain, skin ulcers, and livedo racemosa. We believe that this is an interesting therapeutic association because of the combined blood-vessel calcium chelating effect of IV ST and the vasodilator and antithrombotic effect of the prostaglandins, which help to dilate vessels made rigid by calcium deposits.3,4 Calciphylaxis obliterates blood vessel lumens due to calcification of the wall, fibrosis of the intima, and the development of fibrin thrombi.8
Intralesional ST has also been described in the literature as local treatment for ulcers secondary to calciphylaxis.9 Treatment with hyperbaric oxygen acts by improving healing through its beneficial effects on neovascularization and fibroblast proliferation and by reducing the risk of infection through the release of reactive oxygen species. It is now considered a safe and viable option as part of a multidisciplinary approach to the treatment of calciphylaxis.8,10,11 The improvement in the livedo racemosa can be explained by the prostaglandin-related vasodilatation.
Tolerance to maintenance therapy has been good for more than a year, with a low economic cost given the elevated morbidity and severity of this disease. We therefore consider that the adjuvant role of intravenous alprostadil should be evaluated in cases of severe calciphylaxis that do not respond to standard treatment with IV ST.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Ossorio-García L, Jiménez-Gallo D, Arjona-Aguilera C, Linares-Barrios M. Tratamiento multimodal de la calcifilaxis con tiosulfato sódico, alprostadil y oxigenoterapia hiperbárica. Actas Dermosifiliogr. 2016;107:695–697.