Microvenular hemangioma (MVH) is a rare acquired benign vascular tumor that clinically can be confused with a malignant lesion.1,2 Around 67 cases have been reported in the literature,1–4 but dermoscopic study has only been reported in 3 of these.3–5
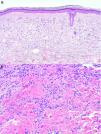
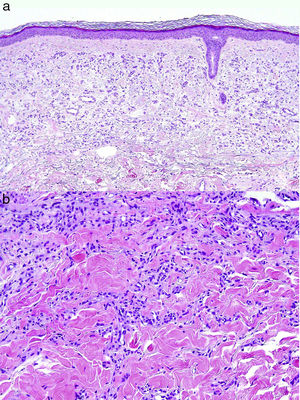
This study presents 3 new cases of MVH, 2 in men and 1 in a woman. Table 1 presents the clinical information of interest and Figure 1 shows the findings of the physical examination and dermoscopy. The lesions were excised and histological findings were diagnostic of MVH and similar in all 3 cases (Fig. 2A and B).
Published Cases of Microvenular Hemangioma With Dermoscopic Description.
| Case | Author/Year | Age | Sex | Comorbidity | Clinical description | Lesion duration | Site | Size, mm | Symptoms | Predisposing factor | Differential diagnosis | Dermoscopy |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Fernández-Morano (2016) | 35 | F | No | Erythematous papule with whitish halo | 8 months | Abdomen | 10×5 | No | No | NR | Pinkish background Scaling Fine pigment network at the periphery |
| 2 | Rivas-Tolosa (2016) | 31 | F | Dysplastic nevus syndrome In situ MM (3 years previously) | Erythematous-violaceous macule | 1 year | Chest | 7 | No | No | NR | Pinkish background Small red globules |
| 3 | Scalvenzi (2007) | 31 | F | No | Erythematous plaque | 6 months | Dorsal | 20×10 | No | No | NR | Pinkish background Red globules of differing sizes Fine pigment network at the periphery |
| 4 | Present series | 67 | M | Lung carcinoma metastatic (RT+CT) (18 years previously) Aortic valve disease | Erythematous plaque measuring 20mm (Fig. 1a) | Several years | Right forearm | 20 | No | Immunosuppression | BCC Amelanotic MM Cutaneous lupus Lymphoma | Pinkish background Fine arborizing telangiectasias |
| 5 | Present series | 70 | M | Type II diabetes mellitus, hypertension, and dyslipidemia | Erythematous macule measuring 6×8 mm (Fig. 1c) | 1 year | Right forearm | 6×8 | Occasional pruritus | Immunosuppression | Kaposi sarcoma Acquired elastotic hemangioma | Pinkish background Fine telangiectasias |
| 6 | Present series | 32 | F | Miscarriage 1 month earlier (8th week of pregnancy) | Erythematous papule measuring 7×5mm (Fig. 1e) | 4 months | Chest | 7×5 | Occasional pruritus | Hormonal | Leishmaniasis Spider veins | Pinkish background Fine telangiectasias White globule |
Abbreviations: BCC, basal cell carcinoma; CT, chemotherapy; F, female; M, male; MM, melanoma; NR, not reported; RT, radiotherapy.
A, Case 1: MVH on right forearm in a 67-year-old man. B, A homogeneous area of pinkish color only is observed along with fine arborizing telangiectasias. The whitish area corresponds to the biopsy scar. C, Case 2: MVH (right) adjacent to a ruby dot (left) on the forearm of a 70-year-old male. D, Dermoscopic image of MVH showing a reddish homogeneous central area and fine, patchy telangiectasias. E, Case 3: MVH on the right side of a 32-year-old woman. F, Dermoscopy shows a central area of whitish-pink color with branched telangiectasias and a milium pseudocyst inside, surrounded by an erythematous area with a peripheral network of telangiectasias.
MVH presents clinically as asymptomatic or mildly pruriginous macules, papules, or nodules of erythematous appearance or violaceous color, which are slow growing and often present as multiple lesions.6 The preferred site is the forearm, as occurred in 2 of our cases. Lesions have also been reported on the chest, abdomen, forehead, legs, and soles.6–9
The pathogenesis of MVH is unknown, although the lesion has been associated with immunosuppression.1 The first of our patients had received treatment for cancer and diabetes could be considered as an immunosuppressive factor in the second case. The disease has also been associated with hormonal factors, which may explain the slight predominance in women,7 and hormonal factors could have played a role in the third case, in which the lesion developed after a miscarriage.
MVH is not usually suspected clinically. In fact, in 50% of published cases, the lesion was excised without any clinical diagnosis. In all remaining cases, the clinical diagnosis issued was incorrect, with malignant vascular tumor being the main suspected condition (Kaposi sarcoma [KS] and well-differentiated angiosarcoma), followed by benign vascular tumor (hemosiderotic hemangioma, tufted angioma, capillary angioma, pyogenic granuloma, angiolipoma, or angiokeratoma). Some cases, including those presented as multiple lesions, were confused with leiomyomas, dermatofibromas, nevocellular nevi, epidermoid cysts, and inflammatory diseases.1–10
In dermoscopy, all our cases as well as the other 3 published cases showed a pinkish tone and fine telangiectasias.3–5 In 2 of the published cases, red globules were also present,4,5 but these were lacking in the third published case3 and in all of our cases (Table 1). In 2 patients, a network of peripheral pigment was observed. The pinkish tone and fine arborizing telangiectasias can also be observed in superficial basal cell carcinoma (sBCC), initial KS, and cutaneous leishmaniasis (CL); and so these lesions may be indistinguishable from MVH. However, MVH does not present characteristic findings of sBCC such as nests and grey-blue globules, maple-leaf structures, wagon wheels, or superficial erosions. Initial KS can also show superficial scaling and peripheral pigment network, but the background tone can be more bluish and, although infrequent, the characteristic pattern described as rainbow form can be seen. Cutaneous leishmaniasis lesions, for their part, usually have an orange-colored background (pointing to the granulomatous etiology of the process), white-yellowish lumps that resemble yellow tears, and, in the most advanced lesions, central ulceration surrounded by hyperkeratosis described as white starburst pattern.9
Definitive diagnosis of MVH is histological. Poorly defined vascular proliferation is observed in the papillary and reticular dermis, with small fine-walled vessels comprising a single layer of endothelial cells and collapsed lumen with no signs of atypia, sometimes grouped into lobules,5 which resemble those observed in tufted angioma, occasionally accompanied by lymphoplasmacytic infiltrate.2 Immunohistochemistry is positive for CD31, CD34, and the angiogenesis marker WT1, and negative for the D2-40 marker of lymphatic differentiation as well as for GLUT-1 (specific to infantile hemangioma), and herpes virus VIII (positive in KS).10
In conclusion, we present 3 cases of MVH, 2 located on the forearm of elderly patients possibly related to immunosuppression and 1 on the chest of a young woman with a history of recent miscarriage. Dermoscopic study of these 3 patients revealed a pinkish background and fine telangiectasias. Unlike the published cases, we did not observe red globules or a peripheral pigment network. Although the dermoscopic findings do not enable diagnosis to be reached, they do distinguish between many but not all of the other lesions included in the differential diagnosis. It is therefore necessary to provide more cases of MVH with dermoscopic study.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Giacaman A, del Pozo LJ, Bauzá A, Saus C. Hemangioma microvenular: estudio morfológico de 3 casos. Actas Dermosifiliogr. 2018;109:381–384.