Microsporum audouinii, an anthropophilic dermatophyte fungus that has been rarely reported since the middle of the last century, is re-emerging in several European countries. Unlike other species that cause ringworm, it can cause epidemics of tinea capitis in schools. We present a typical clinical case and summarize the clinical and epidemiological data from cases recorded in our microbiology department between 2005 and 2017.
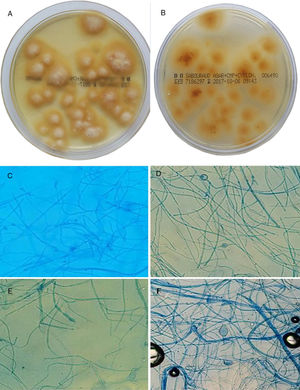
A 5-year-old black boy was seen for multiple areas of alopecia and gray scaling on the scalp (Fig. 1) that had appeared 1 month earlier. Hair and scales were collected from the scalp with a scalpel, carpet square, and a sterile brush. Microscopic examination with 20% KOH + 40% DMSO revealed a mycelium and ectothrix spores compatible with a dermatophyte fungus. Hairs and scales were cultured in Sabouraud chloramphenicol actidione agar, in which flat colonies with a stellate fringe, a woolly-white superficial mycelium, and a pale yellow-orange underside grew after 5 days (Fig. 2A and B). Examination of microscopic morphology after 7 days in potato dextrose agar revealed pectinate hyphae, abortive macroconidia, and intercalary and terminal chlamydospores, enabling identification of the species as M audouinii (Fig. 2C–F). M audouinii was also identified by examination of the culture by matrix-assisted laser desorption/ionization time-of-flight mass spectrometry (MALDI-TOF MS; VITEK MS, bioMérieux, Marcy l’Etoile, France) after incubation for 7 days in potato dextrose agar. The patient had never left Spain, but did have contact with his black African father who had travelled outside the country. Clinical examination and mycological culture of scalp samples from members of the patient's family (except for the father, who was unavailable) confirmed that none presented any lesions or were asymptomatic carriers. No new cases were reported in the patient's school. The patient was treated with micronized griseofulvin in oral suspension (10 mg/kg/d). He responded well during the first month, but fungal regrowth was observed in the second month and the dose was increased to 20 mg/kg/day. Four weeks later, with no further improvement observed, the dose was increased to 25 mg/kg/day. Cure was achieved 8 weeks later, after a total of 5 months of griseofulvin treatment.
A and B, Culture of hairs and scales in Sabouraud chloramphenicol actidione agar for 15 days at 28°C. Flat colonies with a stellate fringe, a woolly-white superficial mycelium (A), and a pale yellow-orange underside (B) are observed. C–F, Microscopic morphology after incubation for 7 days in potato dextrose agar: C, pectinate hyphae (comb-like structure); D, intercalary chlamydospores (original magnification ×20); E, macroconidium (original magnification ×20); F, terminal chlamydospores of M audouinii (original magnification ×20).
Between 2005 and 2017, 16 cases of ringworm due to M audouinii were recorded in our hospital (Table 1). The first was recorded in 2010. Eleven of the 16 cases had tinea capitis and 7 were originally from Africa or had been in contact with other Africans.
Summary of Epidemiological and Clinical Data of Cases of M audouinii Ringworm Recorded in our Microbiology Department From 2005 to 2017.
| Total No. of Cases | 16 |
|---|---|
| No. of cases per year | 3 (2010)0 (2011)0 (2012)2 (2013)1 (2014)1 (2015)8 (2016)1 (2017) |
| No. of cases per age groupChildren, 3–7 yAdults, 20–57 y | 133 |
| No. of cases per clinical form | Tinea capitis: 11Tinea corporis: 4Tinea corporis with tinea capitis: 1 |
M audouinii is a globally distributed anthropophilic dermatophyte fungus, and together with Trichophyton soudanense is the most common cause of tinea capitis in Africa, where it is endemic. Identification by MALDI-TOF MS involves characterization of the isolate's protein profile and comparison with those recorded in a protein library. The results are comparable to those obtained by DNA sequence analysis, provided that the reference spectra of the species to be identified are present in the library used. A review of the incidence of dermatophytes in Spain from 1926 to 1994 found that M audouinii was very common in patients with tinea capitis in Madrid, Zaragoza, Valencia, and Andalusia between 1930 and 1950,1 but practically disappeared in the 1960s after the introduction of griseofulvin.2 The most recent Spanish series indicate that M audouinii continues to be sporadically isolated from patients with tinea corporis, tinea capitis, tinea faciei, and tinea pedis.3,4 However, numerous cases have been recorded in France, again in the form of tinea capitis, and there have been outbreaks in Switzerland, Germany, Belgium, and Australia.4,5 An outbreak among refugee children in Israel was likely due to transmission from other African refugee children.6 Gilaberte and coworkers have described transmission from immunocompetent African mothers to their babies, who become infected in childhood and in whom the fungus persists without causing evident clinical signs.7 A 2016 Cochrane review8 of the treatment of tinea capitis due to Microsporum species reported that griseofulvin treatment for 6 to 12 weeks was more effective than terbinafine treatment for 6 weeks in achieving complete cure (50.9% and 34.7% of patients, respectively), and found no differences in adherence and a reasonable safety profile for both drugs. The recommended dose for griseofulvin is 20mg/kg/day to 25 mg/kg/day for the micronized form available in Spain,8 and 10mg/kg/day to 15 mg/kg/day for the ultramicronised form.9 In the Summary of Product Characteristics provided with the medication supplied to our patient the indicated dose was 10 mg/kg/day, even though the formulation was the micronized form. The patient's mother administered the recommended dose up until the first examination, at which point we noticed the error. Forms of tinea other than tinea capitis can be successfully treated using topical antifungals or, in case of follicular involvement, systemic antifungals such as itraconazole (100 mg/d for 3 months).10
Because the incidence of this dermatophyte fungus is likely to continue to increase in Spain, it is important to be aware of its clinical and demographic features and the risk of possible outbreaks.
Please cite this article as: Lozano-Masdemont B. Microsporum audouinii: un dermatofito causante de una tiña reemergente Eczema y urticaria en Portugal. 2019;110:785–787.