Linear basal cell carcinoma was first described by Lewis1 in 1985 as a rare morphological variant of basal cell carcinoma. Since that time, 35 cases have been reported in the literature. The most common site is the periocular region.2,3
We report a new case of linear basal cell carcinoma, in which the clinical diagnosis was based on physical examination and dermoscopy and was confirmed by histological study. We review the current literature on linear basal cell carcinoma and discuss its principal features.
The patient, a 42-year-old woman, came to our department for a slowly enlarging, linear pigmented lesion on the right lower eyelid that had appeared one year earlier. She had skin phototype iv. There was no history of trauma or of a previous lesion at that site.
On physical examination there was a linear pigmented lesion measuring 1.5×0.4cm. The lesions had a pearly border and central scarring (Figure 1).
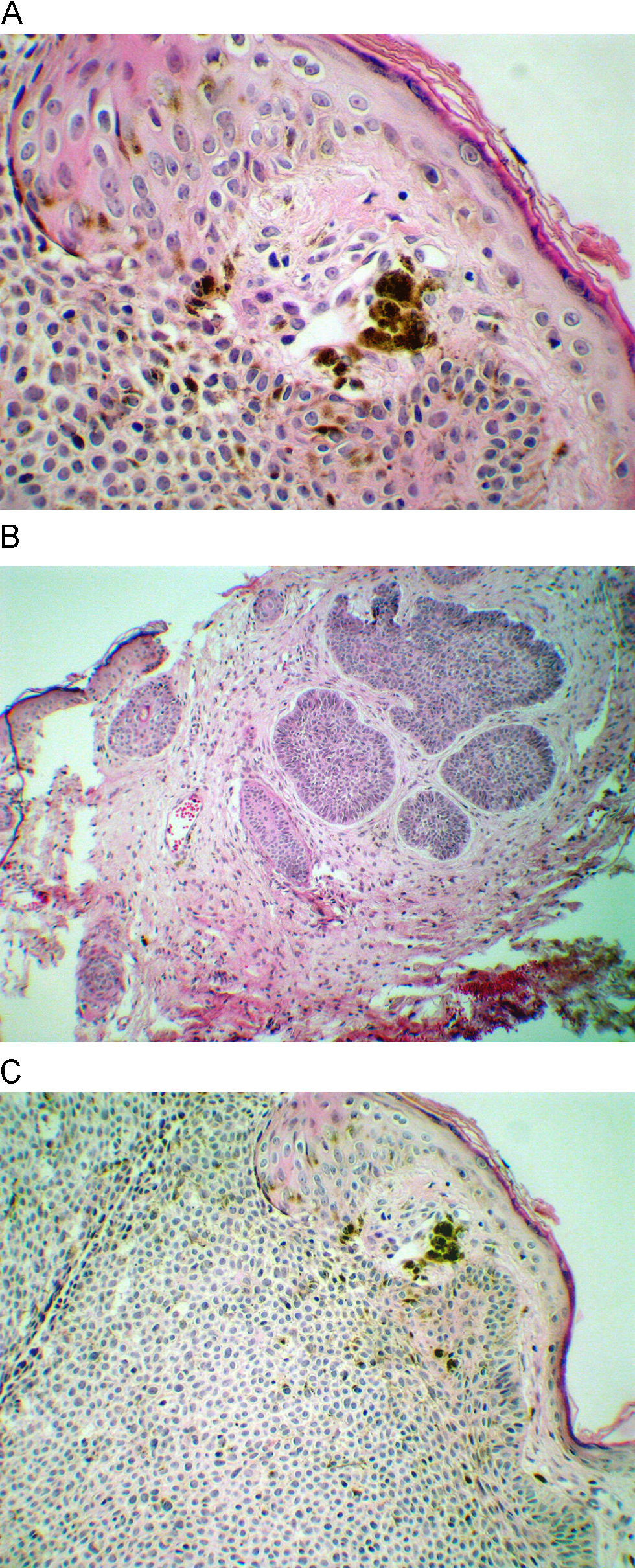
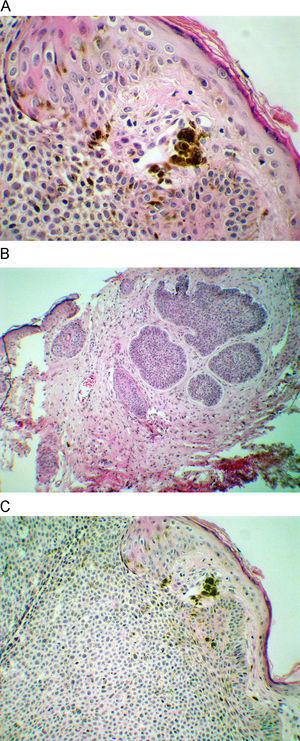
Dermoscopy revealed the absence of a pigmented network pattern and the presence of a specific BCC dermoscopy pattern: multiple blue-gray ovoid nests, arborizing telangiectatic vessels with a feathery appearance, and slight ulceration (Figure 2). The diagnosis of BCC was confirmed by histological study of a punch biopsy (Figure 3A).
The lesion was removed by simple excision, with primary closure of the wound. The surgical margins were free of tumor cells (Figure 3B). Pigmentation was present in tumor and in the stroma (Figure 3C). After 4 years of follow-up there has been no recurrence.
In 1985, Lewis1 reported a new clinical subtype of basal cell carcinoma in a patient with a 20mm linear pigmented lesion on the left cheek. Five years later he reported a further 4 cases.4 Since then, 33 cases of linear basal cell carcinoma have been reported as a distinct morphological entity.3,5 In 2007, Pardavilla et al.3 reported 2 more patients with this lesion, bringing the total to 35. We report a new case of linear basal cell carcinoma.
Some authors believe that linear basal cell carcinoma has specific clinical and histological features and can be regarded as a distinct entity. Mavrikakis et al.5 more objectively define linear BCC as a lesion that appears to extend preferentially in one direction, resulting in a lesion with relatively straight borders and with a length much greater than the width (ratio of 3:1). Histologically, it may vary from a predominantly nodular to an aggressive subtype.
Linear basal cell carcinoma occurs in equal proportions in men and women, in an age range from 40 to 87 years, though more than 92% of patients were aged over 60 years.6 The periocular area was the site most commonly affected (17 of the 35 cases), with the majority occurring on the lower eyelid or cheek (as in our case). The second most common site was the neck, followed by the trunk, lower face, and inguinal skin crease.2,5
Some of the mechanisms that have been suggested to explain this mode of growth include limitation of lateral spread of the lesion by dermal fibrosis or interactions of the stroma with the Langer lines (3). Other authors have speculated on the possibility of a Koebner phenomenon, based on its linear patterns and the fact that these tumors are oriented along the tension lines of the skin. However, there have only been 3 patients with a history of trauma among the 35 cases reported. The Koebner phenomenon cannot be implicated in our case as there was no history of trauma.
Scott and Menzies7 described the dermoscopic features of pigmented basal cell carcinoma. They stated that the diagnosis of a pigmented BCC required absence of the negative feature of a pigmented network and the presence of one or more of the following 6 positive features: large, blue-gray ovoid nests; multiple blue-gray globules; maple leaf-like areas; spoke wheel areas; ulceration; and arborizing “tree-like” vessels. In our case there were 3 positive features and the negative element was absent. The feather-like images were a new finding in this linear basal cell carcinoma and we would suggest that this could be included in the dermoscopic diagnosis of linear BCC.
The most common histological subtype in all 35 reported cases was nodular basal cell carcinoma, followed by the pigmented subtype.2 Of the 17 cases in the periocular region only 2 cases were pigmented. Pigmented BCCs are common in individuals with skin phototype iv, which was also our patient's skin type. Tunisia has a climate that predisposes to prolonged exposure to the sun, and this could therefore also have played a role.
Linear BCC can also be seen in linear unilateral basal-cell nevus syndrome with comedones. This extremely rare disease, which is characterized by the unilateral distribution of basal-cell carcinomas, comedones, epidermoid cysts and areas of stria-like atrophy, is believed to be distinct from the nevoid basal-cell carcinoma syndrome.8
Orientation along the tension lines of the skin allows technically simple excision (as in this case), and the healing and cosmetic results are good. The presence of the tumor along the relaxed tension lines, subclinical spread, and aggressive tumor behavior have been reported, and it is therefore suggested that margin-controlled excision should be considered for linear BCC.
In some cases, Mohs surgery is the second surgical option. However, some authors consider this technique to be the treatment of choice.5,6
Linear basal cell carcinoma is an uncommon morphological variant that requires clinical recognition and adequate treatment. Our patient is particularly interesting due to her relatively young age, the pigmented lesion, feather-like dermoscopic images, and good healing without recurrence.