Alopecia areata (AA) is a frequent autoimmune non-scarring hair-loss disorder which can have a significant impact on quality of life. It usually presents with sharply demarcated alopecic patches, although multiple clinical variants of AA have been described. Linear alopecia areata (LAA) is exceedingly rare.1–4 Here we present a series of patients (one adult and two children) with LAA.
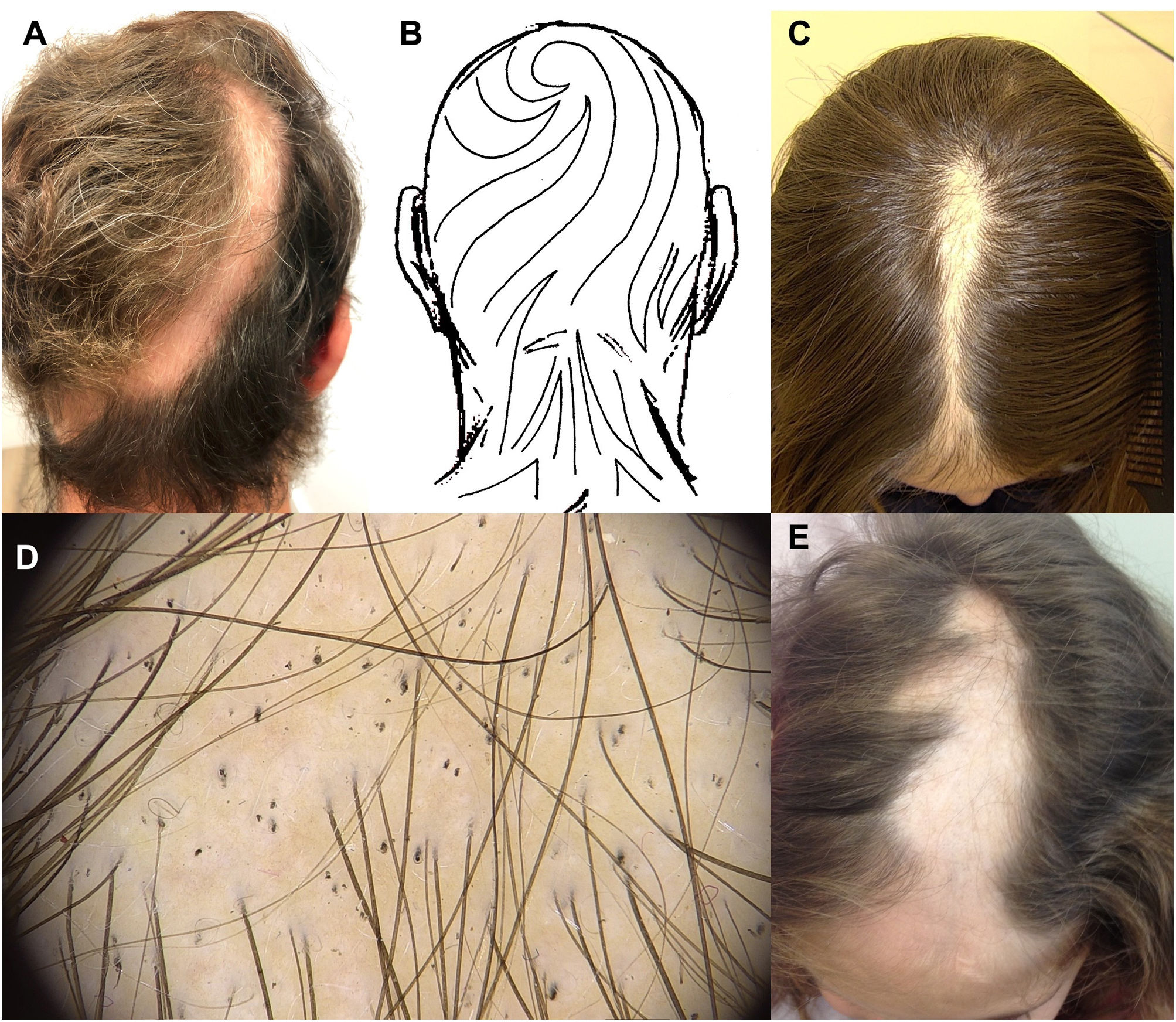
The first case was an otherwise healthy 26-year-old male who presented with a history of 8 months of hair loss. Physical examination revealed a 23cm linear alopecic patch extending from the vertex to the left occipital area (Fig. 1A), following Blaschko's lines (Fig. 1B). The skin was normal in appearance in the alopecic area. Trichoscopy showed black and yellow dots, short vellus hairs and exclamation mark hairs. A diagnosis of LAA was made. Topical 5% minoxidil, mini-pulse therapy with prednisone (20mg on two consecutive days weekly) and intralesional triamcinolone acetonide injections every six weeks were started. In the following 4 months, a mild response was observed, and topical 1% anthralin lotion was initiated with partial response after 3 months. The patient was lost to follow-up.
Linear alopecia areata. (A) Linear alopecic patch extending from the vertex to the left occipital area, following Blashko's lines. (B) Blashko's lines on the head. (C) Linear alopecic patch along the interparietal area. (D) Trichoscopy shows black dots, pigtail hairs and exclamation mark hairs (FotoFinder® medicam 1000, Fotofinder systems, Germany). (E) Linear alopecic patch on the frontal and left parietal area.
Our second case, a 9-year-old girl with no previous comorbidities presented with scalp hair loss during the previous 3 months. On physical examination a linear alopecic patch was observed along the interparietal area (Fig. 1C). The pull test was positive. Trichoscopy showed black dots, pigtail hairs and exclamation mark hairs (Fig. 1D). No erythema, atypical vessels or perifollicular scaling were seen. These findings were consistent with LAA. Oral prednisone 15mg/day was prescribed with progression of the alopecia during the following month. Dexamethasone 0.1mg/kg twice a week was then initiated, with complete response after 6 months. Treatment was then stopped. No recurrences have been seen after 2 years of follow-up.
The third case, an otherwise healthy 5-year-old girl presented with hair loss during the previous month. Physical examination showed a linear alopecic patch with normal skin appearance on the frontal and left parietal area (Fig. 1E). The hair pull test was positive. Trichoscopy revealed yellow and black dots and exclamation mark hairs. A diagnosis of LAA was made. Topical 0.05% Clobetasol foam was prescribed and complete response was observed during the following three weeks, and topical corticosteroid was then suspended. The patient was lost to follow-up.
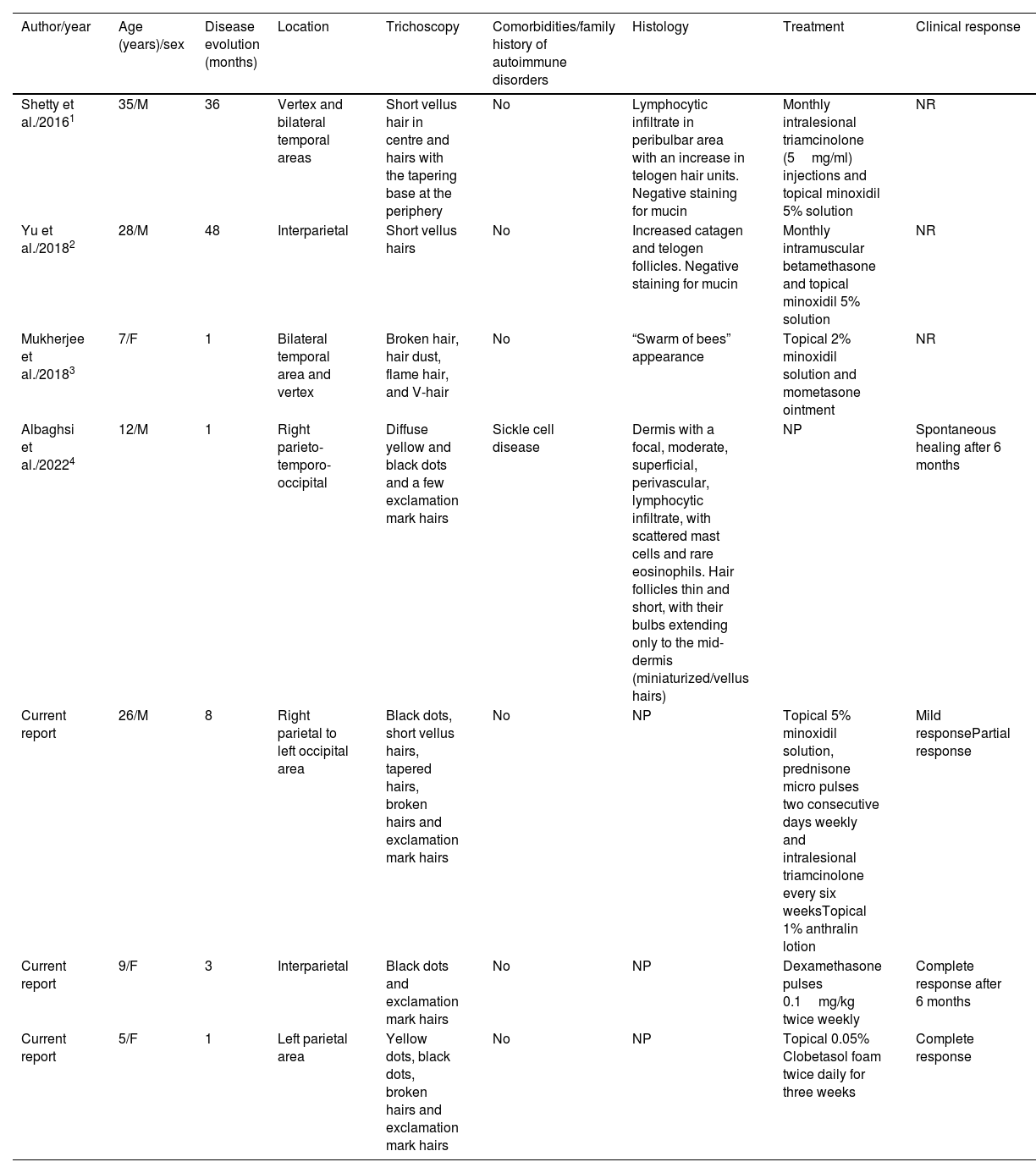
The clinical presentation of AA can be highly variable, even annular or rectangular-pattern variants have been described.5 Only four cases (two adults and two children) presenting with LAA have been reported (Table 1).1–4 While the gold standard in the diagnosis of hair-loss disorders is the histopathology, in real-life practice the diagnosis of AA is generally based on clinical and trichoscopic findings, and histologic study is only performed in challenging cases. Trichoscopy of AA is characterized by the presence of black and yellow dots, short vellus hairs, pigtail (circle) hairs, upright regrowing hairs, tapered hairs, Pohl-Pinkus constrictions and exclamation mark hairs.3
Cases with linear alopecia areata described in the literature.
| Author/year | Age (years)/sex | Disease evolution (months) | Location | Trichoscopy | Comorbidities/family history of autoimmune disorders | Histology | Treatment | Clinical response |
|---|---|---|---|---|---|---|---|---|
| Shetty et al./20161 | 35/M | 36 | Vertex and bilateral temporal areas | Short vellus hair in centre and hairs with the tapering base at the periphery | No | Lymphocytic infiltrate in peribulbar area with an increase in telogen hair units. Negative staining for mucin | Monthly intralesional triamcinolone (5mg/ml) injections and topical minoxidil 5% solution | NR |
| Yu et al./20182 | 28/M | 48 | Interparietal | Short vellus hairs | No | Increased catagen and telogen follicles. Negative staining for mucin | Monthly intramuscular betamethasone and topical minoxidil 5% solution | NR |
| Mukherjee et al./20183 | 7/F | 1 | Bilateral temporal area and vertex | Broken hair, hair dust, flame hair, and V-hair | No | “Swarm of bees” appearance | Topical 2% minoxidil solution and mometasone ointment | NR |
| Albaghsi et al./20224 | 12/M | 1 | Right parieto-temporo-occipital | Diffuse yellow and black dots and a few exclamation mark hairs | Sickle cell disease | Dermis with a focal, moderate, superficial, perivascular, lymphocytic infiltrate, with scattered mast cells and rare eosinophils. Hair follicles thin and short, with their bulbs extending only to the mid-dermis (miniaturized/vellus hairs) | NP | Spontaneous healing after 6 months |
| Current report | 26/M | 8 | Right parietal to left occipital area | Black dots, short vellus hairs, tapered hairs, broken hairs and exclamation mark hairs | No | NP | Topical 5% minoxidil solution, prednisone micro pulses two consecutive days weekly and intralesional triamcinolone every six weeksTopical 1% anthralin lotion | Mild responsePartial response |
| Current report | 9/F | 3 | Interparietal | Black dots and exclamation mark hairs | No | NP | Dexamethasone pulses 0.1mg/kg twice weekly | Complete response after 6 months |
| Current report | 5/F | 1 | Left parietal area | Yellow dots, black dots, broken hairs and exclamation mark hairs | No | NP | Topical 0.05% Clobetasol foam twice daily for three weeks | Complete response |
Abbreviations: M, male; F, female; NP, not performed; NR, not reported.
Differential diagnoses of alopecia with linear distribution include linear epidermal nevi, linear scleroderma, linear lichen planus, linear folliculitis decalvans, linear cutaneous lupus erythematosus (LCLE),6 LAA and trichotillomania.3 An accurate diagnosis is important since management and clinical implications can be different. Trichoscopy can be very useful in this context: in LCLE it may reveal thick or prominent arborizing blood vessels, brown or blue-grey speckled pigmentation and black dots; in linear scleroderma, pili torti, broken hairs, and black dots on a whitish skin surface and thick telangiectatic vessels; and in trichotillomania, broken hair, black dots, flame hair, and V-hair.3
As we all know, the prognosis of AA is extremely variable and difficult to predict. We have found no reports suggesting that LAA can have different prognosis or outcomes.
We have presented a series of three patients with LAA and highlighted the importance of trichoscopy in the differential diagnosis of linear-pattern hair loss. Dermatologists should be aware of this in order to avoid performing invasive diagnostic procedures.
Conflict of interestThe authors declare that they have no conflict of interest.