Penile Mondor's disease (PMD) is a non-migratory and self-limited thrombophlebitis of the superficial veins of the penis. It is considered a subtype of Mondor's disease, in which thrombophlebitis is often found in the shaft.1,2 Despite being linked to multiple triggers, its specific etiopathogenesis is unknown. Diagnosis requires confirmation of thrombophlebitis, preferably via ultrasound, as well as ruling out other causes of thrombophilia.1,3 We present the first case ever reported in the literature of PMD following selective sentinel lymph node biopsy (SLNB) in the groin of a patient without risk factors for thrombosis.
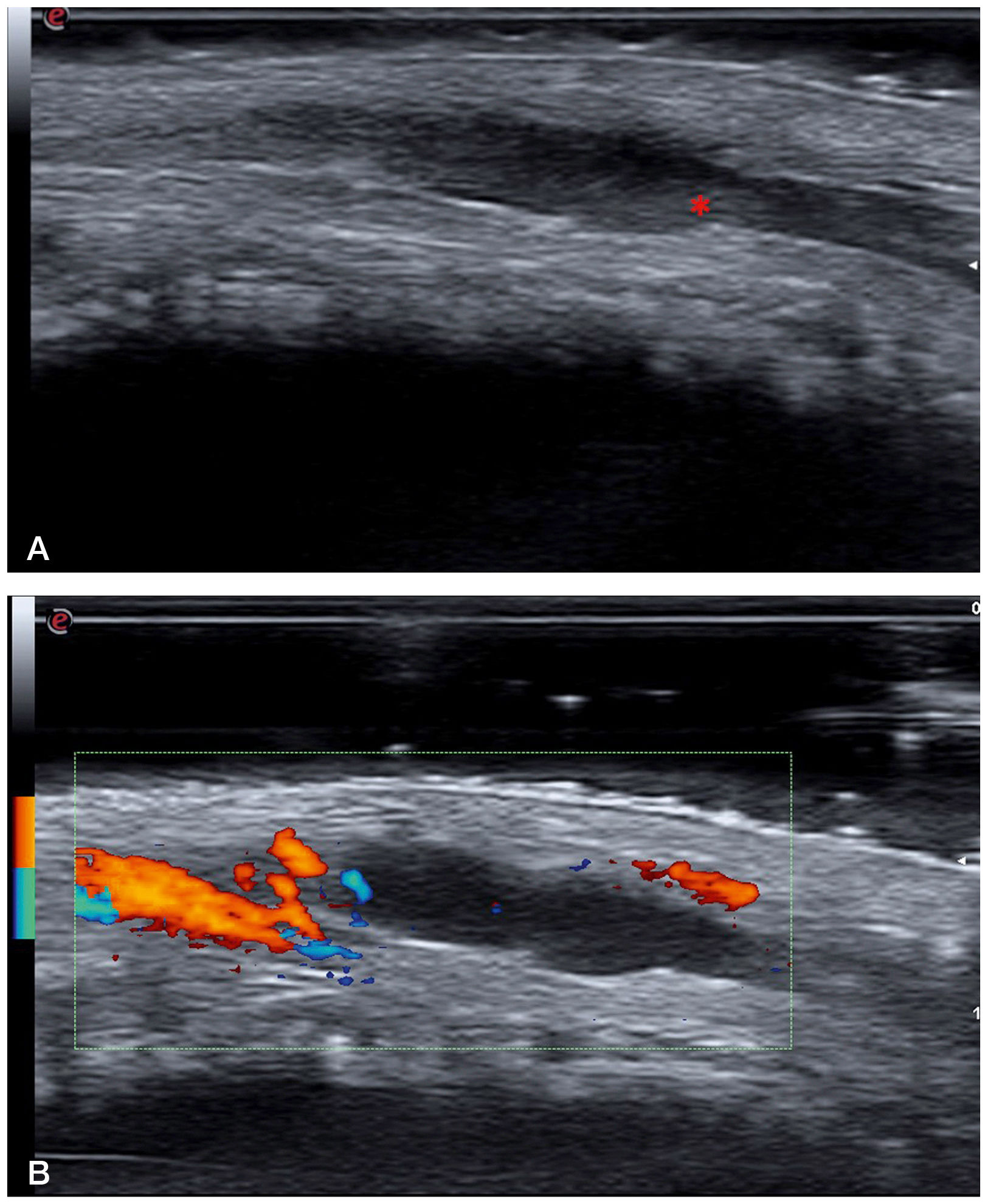
A 54-year-old man, with no relevant past personal history was diagnosed with a stage IIA 2.1mm Breslow thickness melanoma in the medial lumbar region after a regular check-up. Subsequently, a surgical wide excision was performed, followed by an extension study with bilateral inguinal lymph node ultrasound which revealed no pathological findings. Additionally, a right inguinal SLNB performed tested negative. Fifteen days after surgery, he consulted for pain in the dorsal shaft of the penis. Physical examination revealed the presence of an indurated subcutaneous cord with no additional findings (fig. 1). A cutaneous ultrasound (Esaote MyLab Gamma®, linear probe of 6-18 MHz) revealed the presence of a dilated, hypoechoic, non-compressible tubular structure with hyperechoic content and no Doppler flow inside, which was consistent with thrombosis of the penis superficial dorsal vein (fig. 2). A suspected diagnosis of PMD due to inguinal SLNB followed. The patient was assessed by the urology department, which prescribed analgesic treatment with diclofenac and performed a soft tissue ultrasound that eventually confirmed the diagnosis of superficial venous thrombosis without deep involvement. The patient was also evaluated by the hematology department, which ruled out other causes of primary thrombophilia and administered low molecular weight heparin (LMWH). The course of the disease was favorable, and serial ultrasound follow-up confirmed the resolution of thrombosis after 2 months. LMWH was discontinued after resolution, and no recurrences or thrombophlebitis in other areas have been reported at the 18-month follow-up.
a: B-mode ultrasound image (18 MHz) showing a hypoechoic and dilated tubular structure, which is consistent with a superficial vein. This structure was not compressible under pressure. The hyperechoic content indicated by the asterisk corresponds to the intraluminal thrombus. b: Power Doppler ultrasound image showing absence of flow inside the thrombosed vein. The image Doppler flow comes from one of the dorsal arteries of the penis.
Multiple conditions favor the occurrence of thrombosis. These are usually categorized as primary or secondary thrombophilias.3 We should mention that most patients with thrombophilia will not end up developing thrombosis, and it is the addition of several predisposing factors that eventually determines its occurrence.
In PMD, the main predisposing factor described is intense and prolonged sexual intercourse, which would cause endothelial microtrauma, leading to thrombus formation. Similarly, it has also been associated with direct trauma or the use of vacuum devices or intracavernosal injections in the context of erectile dysfunction.1
Of all the triggers described, the only one identified in our patient was a recent inguinal SLNB. Cases of PMD after pelvic surgical procedures and inguinal hernia surgeries have been reported, the latter being the most representative antecedent for our case.4 Although in melanoma patients, lower limb deep vein thrombosis has been described after SLNB, no cases of penile vein thrombosis following this procedure have been reported to this date.5
Clinically, PMD presents as an indurated and painful subcutaneous cord located on the dorsal haft of the penis, which resolves spontaneously within 4 to 8 weeks.1 Atypical forms with involvement of the circumflex or ventral veins have been described.6,7 For the diagnosis of thrombosis, the technique of choice is Doppler ultrasound.1,8 The main differential diagnosis is sclerosing lymphangitis of the penis, which presents as a self-limited indurated subcutaneous cord in the balanopreputial sulcus. Since it is a lymphatic vessel disorder, ultrasound will not show any images of venous thrombosis.1,9 Additionally, ultrasound allows us to rule out the presence of solid tumors in the shaft of the penis that may be clinically suggestive of thrombosis.10
There is no consensus on the need for other additional tests, which should be individualized for each patient. Therefore, multidisciplinary management is essential here. As part of the initial study, blood tests are considered appropriate to rule out causes of primary thrombophilia. Given that PMD should be a self-limited and non-migratory condition, any variation in its course would require considering an alternative diagnosis. Because of its good prognosis, conservative management with analgesics can be administered, while the jury is still out on the need for anticoagulant therapy.1
In conclusion, PMD should be understood as a benign and self-limited entity with multiple predisposing factors, and its diagnosis should always be one of exclusion. Of note the role of cutaneous ultrasound to both diagnose and monitor and this condition.
Conflicts of interestNone declared.