The diagnosis of flat pigmented lesions on facial skin chronically exposed to sunlight presents particular challenges for the dermatologist. The clinical presentation is that of an acquired flat pigmented lesion, in shades of brown to black, with irregular edges and characterized by slow growth. With such lesions, we are always concerned about the possibility of melanoma, and the differential diagnosis includes solar lentigo (or flat seborrheic keratosis), pigmented actinic keratosis, and lichenoid keratosis. While dermoscopy has obviously helped a great deal, it is clear that the definitive diagnosis in such cases will always be dermatopathological.
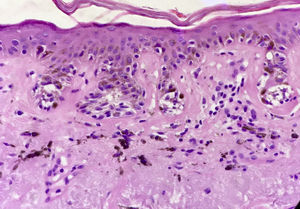
The first question we must ask ourselves is whether a diagnosis of melanocytic nevi is a possibility with this kind of lesion. Any clinical dermatologist who looks at the image in Figure 1 will agree that melanocytic nevi is not a possible diagnosis in this case. This lesion could not be a junctional nevus, a compound nevus, or even a dysplastic nevus. It is not the right size, the clinical appearance is not that of a nevus, and nevi do not present slow and progressive growth in adults. In fact, we know that nevi on the faces of older people are generally papular and in appearance are like the lesion shown in Figure 2.
However, if we fail to provide adequate clinical information to the pathologist when we biopsy a flat pigmented lesion on the face of an older adult we may receive a report identifying the lesion as a junctional, compound, or dysplastic nevus.1 If this happens, it is crucial to provide the pathologist with the clinical data required to reach a more accurate diagnosis. Therefore, while it is important to accompany any biopsy sample with clinical information that can help the pathologist to make an accurate clinical and pathological correlation, this information is absolutely essential in the case of this particular type of lesion.
A study of serial histological sections will often be sufficient to resolve the problem, but at times it may be necessary to repeat the biopsy. These are often large lesions on which a partial biopsy was performed, so a second biopsy is generally feasible.
It should be noted that in this type of lesion, partial biopsies are much more useful when they are guided by dermoscopy. Sampling an area where dermoscopy reveals a rhomboid pattern or where a follicular opening is occluded by pigment is much more likely to lead to a correct diagnosis.
In conclusion, when the possible clinical diagnoses are solar lentigo vs lentigo maligna and the biopsy report identifies the lesion as a nevus, it is time for us to contact the pathologist and provide more clinical information because, in such cases, the most likely possibility is that the lesion is, in fact, a melanoma.
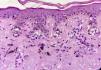
The Problem of Flat Pigmented Lesions on the Face from the Pathologist's StandpointPathologists evaluating a biopsy sample taken from a flat melanocytic facial lesion in an older person should bear in mind that the diagnostic criteria for melanoma in such cases differ from the classic criteria used to differentiate nevi and melanomas in other settings. For example, in the case of a lesion like the one shown in Figure 1, the presence of nests along the dermoepidermal junction and prominent solar elastosis should already make us suspect in situ melanoma (Fig. 3). It does not matter whether there is melanocytic atypia or pagetoid spread or whether the melanocytes compromise the follicle; the most likely diagnosis is melanoma. ¿Why? Because the lesion in Figure 1 can never be a junctional or dysplastic nevi; in fact, it can never be any type of melanocytic nevi.
An important factor that contributes to diagnostic error is that the samples we receive for the assessment of these facial lesions are often small partial biopsies. These are usually extensive facial lesions and the clinician does not have the required diagnostic certainty to perform the excision biopsy that would be indicated in the case of a melanoma. To minimize disfiguring scars, therefore, a partial biopsy is performed in case the lesion turns out to be benign.
A partial biopsy of a melanocytic lesion is difficult to evaluate: for example, the pathologist does not know whether the lesion is asymmetric or poorly circumscribed, both very important characteristics in the assessment of a melanocytic lesion. Moreover, the biopsy may have been taken from an area of the lesion characterized by fewer atypical or pagetoid melanocytes or less mitosis.
We should also point out that dermatopathologists often encounter cases where the evidence is even less obvious, in which a diagnosis of lentigo maligna must be reached without the presence of nests, solely on the basis of an exaggerated proliferation of atypical melanocytes. In such cases, the differential diagnosis with pigmented actinic keratosis or melanocytic hyperplasia secondary to photodamage can be difficult. Sun-damaged skin can demonstrate increased melanocytic density, and the cells may even have atypical features that are not due to malignant proliferation. In such situations, immunohistochemical techniques are needed to help us identify a lentigo maligna. Melan A is the most widely used technique for identifying basal melanocytic proliferations. However, some authors consider that it may overestimate the number of melanocytes because it stains melanocytic dendrites and possibly pigmented keratinocytes. They advocate using other immunohistochemistry techniques, such as MITF-1 and SOX -10.2
Another complex issue is whether a diagnosis of lichenoid keratosis is accurate or whether the lesion is, in fact, a melanoma in regression. Melanomas with lichenoid regression may mimic a benign lichenoid keratosis, and the regression reaction can obscure the melanocytes upon hematoxylin and eosin staining. Immunohistochemical techniques are also useful in such cases.
Finally, when the biopsy is a sample of facial tissue, the presence of nests of melanocytes at the dermoepidermal junction in association with prominent solar elastosis is highly suggestive of melanoma. Sometimes immunohistochemistry techniques are required to diagnose lentigo maligna, especially when the presentation is lentiginous and the differential diagnosis is between pigmented actinic keratosis, lichenoid keratosis, and melanocytic hyperplasia in sun-damaged skin.
Final ConsiderationsIt is questionable whether the concepts we are dealing with apply only to flat pigmented lesions in older people when they are on the face or whether they also apply to lesions in other chronically sun exposed sites.
The above assertions are valid for any areas where nevi quickly become intradermal, such as the face and neck. However, we know that in other areas, such as the upper limbs and the trunk, nevi evolve in different ways and may be flat in older people. We must, therefore, be much more careful when assessing the possibility of a diagnosis of in situ melanoma in such settings. It is essential to look for other features that might support a diagnosis of melanoma, such as the classical criteria proposed by Ackerman (nonequidistant scatter of melanocytes, melanocytes at the dermoepidermal junction, descent of melanocytes into adnexal structures, etc.).3
The need for a different approach to flat pigmented lesions on the face in older people forces us to address the uncomfortable issue of what we mean by older people. In reality, the main limiting factor for all of the above to be applicable is whether a diagnosis of nevus could be included in the differential diagnosis of the lesion. If a diagnosis of nevus is possible given the patient's age and the type of lesion, the criteria of “nests of melanocytes at the dermoepidermal junction in association with prominent solar elastosis is highly suggestive of melanoma” does not apply.
It is clear that all of these diagnostic difficulties are minimized if the clinical pathological correlation is good. If the dermatologist provides clear information on the type of clinical lesion sampled, the dermatopathologist will understand that nevus is not a good diagnostic option, even when the biopsy is small and there is minimal or no melanocytic atypia. The most powerful weapon for good diagnostics is still teamwork between clinicians and pathologists that facilitates and encourages clinical and pathological correlation.
ConclusionsIt can be useful to remember the title of this article when faced with the problem of diagnosing a flat pigmented lesion on the face of an elderly patient: Is it solar lentigo or lentigo maligna? It is not a nevus.
Please cite this article as: Mazzei ME. ¿Lentigo solar vs lentigo maligno? No es nevo. Actas Dermosifiliogr. 2016;107:451–453.