Longitudinal melanonychia is characterized by the presence of light to dark brown or black pigmentation of the nail plate. It occurs in individuals of certain racial origins, such as blacks, Latin Americans, and Asians, but it can also be induced by trauma or drug therapy or found in benign conditions such as infections and melanocytic lesions (e.g., nail apparatus lentigo and nevi). It is also a feature of subungual melanoma. Subungual melanoma is a rare malignancy that accounts for approximately 0.7% to 3.5% of all melanomas in the general population.1 Dermoscopy is a useful tool for the differential diagnosis of longitudinal melanonychia.2 One of the hallmark signs of subungual melanoma is the Hutchinson sign, which describes periungual pigmentation of the nail folds and hyponychium.3,4 The sign has traditionally been associated with poor prognosis in subungual melanoma as it indicates radial growth. Not all Hutchinson signs, however, are associated with subungual melanoma. Some individuals may have a pseudo-Hutchinson sign, which refers to the presence of a dark pigment made visible through a translucent cuticle.4,5 In addition, patients with benign melanocytic lesions, such as congenital nevi, may also have periungual pigmentation of the nail folds, raising suspicion of subungual melanoma6–8 even though this tumor is very rare in the pediatric population.
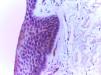
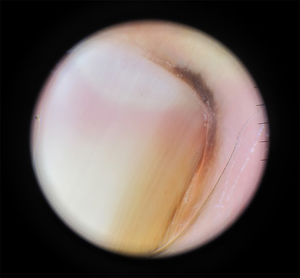
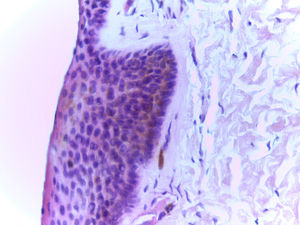
Case DescriptionA 25-year-old woman presented with longitudinal melanonychia on her right index finger. The pigmentation had been present since the patient was 8 years old and had not changed in appearance. The patient had Fitzpatrick type III skin and the physical examination showed a dark brown band measuring 2mm in width on the right index finger. There was also a notable Hutchinson sign (Fig. 1). The dermoscopic examination showed brown parallel bands along the length of the nail plate and the Hutchinson sign in the proximal and lateral folds (Fig. 2). An excisional biopsy of the nail matrix and affected folds showed a mildly acanthotic squamous epithelium with preserved epithelial maturation and epithelial melanosis in the basal layer, but no evidence of lentiginous melanocytic proliferation or melanocyte nests. Periodic acid-Schiff staining was negative and there were no signs of hemorrhage (Fig. 3). The findings were consistent with nail apparatus lentigo. The functional and cosmetic results after just a few months were satisfactory.
Determining the benign or malignant nature of melanonychia is challenging and requires 3 steps, the first of which is to determine whether the pigment is melanin. If it is, the second step is to discover whether the increase in melanin is due to melanocytic activation or proliferation. Dermoscopically, gray homogeneous bands suggest activation, while brown or black bands suggest proliferation.2 The third step is to determine whether the melanocytic proliferation corresponds to a benign condition (acquired, congenital, or lentiginous nevi) or a malignant one (subungual melanoma). Signs that suggest subungual melanoma include a loss of parallelism, progressive thickening of the nail band, heterogeneous pigmentation, Hutchinson sign, and nail dystrophy.2 The problem is when a patient has melanonychia with benign features and the Hutchinson sign.
Intraoperative nail matrix dermoscopy has identified dermoscopic patterns that correlate strongly with certain benign lesions and melanoma, and while still in its infancy, this diagnostic modality could be clinically useful in the future.9
The Hutchinson sign, which was first described in 1886, has always been considered to be strongly suggestive for subungual melanoma. False positives, however, are relatively common and are seen in benign conditions such as Peutz-Jeghers and Laugier-Hunziker syndrome, radiation therapy, drug therapy (minocycline), trauma-induced injuries, congenital nevi, ethnic pigmentation, and systemic diseases, such as hyperthyroidism, Cushing syndrome, and deposition disorders.2,3 Congenital nevi may also exhibit signs of malignancy, such as the Hutchinson sign and progressive darkening and thickening of the nail band.6–8
Our patient had had longitudinal melanonychia since childhood and had experienced no changes. We performed a biopsy because of the Hutchinson sign, even though the dermoscopic image showed a parallel lesion with uniform coloring (Fig. 2). It is important to note that the Hutchinson sign is not considered pathognomonic for melanoma and this is particularly true for children, where clinical and dermoscopic criteria have not been validated as they have for adults.6,10 We have presented this case because it provides an example of a false positive for subungual melanoma. We do, however, strongly recommend performing biopsy whenever the Hutchinson sign is observed due to its close association with subungual melanoma.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Catalán V, Yagnam M, Morales C, Villagra M. ¿Es el signo de Hutchinson patognomónico de melanoma subungueal. Actas Dermosifiliogr. 2018;109:573–575.