Although dermatology has traditionally been practiced through outpatient consultation, hospitalized patients often have dermatologic problems. The aim of this study was to describe and quantify the volume of interdepartmental consultation of the dermatology department of Hospital Universitario Virgen del Rocío.
Material and methodsIn this year-long prospective observational cohort study of 429 patients we used a specific data collection form to record information on consultations for patients admitted between July 2010 and June 2011.
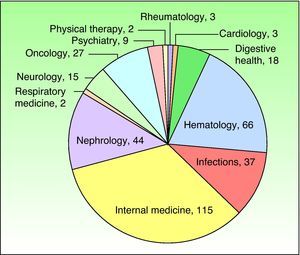
ResultsThe 429 consultations over the 12 months of study accounted for 1.56% of all first consultations with a dermatologist during the period. A mean of 1.75 new patients were attended each day. The mean (SD) age of the patients was 52.63 (19) years, and the ratio of men to women was 1.21. Immunocompromised patients accounted for more than a third of the cohort. The medical specialties consulting most often were internal medicine (n=115) and hematology (n=66). The most frequent diagnoses were inflammatory skin conditions (36.2%) and infectious skin diseases (26.5%).
Discussion and conclusionsTo date, the role of interdepartmental consultation in dermatology has been little studied. Our results suggest that dermatology plays a fundamental role within the hospital. We have identified the most common skin problems in hospitalized patients and their clinical course.
La Dermatología se ha considerado clásicamente una especialidad limitada a las consultas externas. Sin embargo, los pacientes ingresados presentan frecuentemente problemas dermatológicos. El objetivo de este estudio es describir y cuantificar el volumen de la interconsulta hospitalaria del Servicio de Dermatología del Hospital Universitario Virgen del Rocío.
Material y métodosSe trata de un estudio observacional sobre una cohorte prospectiva de 429 pacientes durante un año. Se recogieron todas las interconsultas sobre pacientes ingresados desde julio de 2010 a junio de 2011, a través de la utilización de una ficha.
ResultadosSe recogieron un total de 429 interconsultas durante 12 meses; esto supuso el 1,56% de todas las primeras consultas durante este periodo, con una media de 1,75 pacientes nuevos/día. La edad media de los pacientes atendidos fue 52,63 años (±19). La distribución entre ambos sexos, a razón mujer/hombre, fue de 1,21. Más de un tercio de los pacientes atendidos estaban inmunodeprimidos. Las especialidades médicas más demandantes fueron Medicina Interna (n=115) y Hematología (n=66). El diagnóstico más frecuente correspondió a las dermatosis inflamatorias (36,2%), seguido por las dermatosis infecciosas (26,5%).
Discusión y conclusionesHasta el momento el papel de la interconsulta en Dermatología ha sido escasamente valorado. Nuestros resultados nos permiten afirmar que la Dermatología desempeña un papel fundamental dentro del ámbito hospitalario, así como ha posibilitado que conozcamos la dolencia dermatológica más frecuente en pacientes ingresados y la evolución de los mismos.
Although their routine practice largely consists of outpatient consultation, dermatologists also play a fundamental role in hospital care. Patients are rarely hospitalized for dermatologic problems alone, but such problems are common among admitted patients and can cause substantial comorbidity.
The mechanism by which other specialists contact the dermatology department to request a dermatologist's opinion is called interdepartmental consultation, an understudied and sometimes underestimated aspect of dermatology practice.
The general objectives of this study were to quantify the exact volume of interdepartmental consultation and to describe the characteristics of this activity (departments consulting most often, patient characteristics, most frequent diseases, number of follow-up visits, etc.).
Patients and MethodIn this prospective observational cohort study, we recorded information on all interdepartmental consultations requested of the dermatology department at Hospital Universitario Virgen del Rocío between July 1, 2010, and June 30, 2011.
This public hospital, managed by the Andalusian Health Service, directly serves a population of 553 179 and is the provincial referral hospital for a further 1 306 659 people.
In an average year, the dermatology department handles 27 395 initial consultations and 19 hospital admissions.1 Of the 10 dermatologists in the department, 1 is assigned to interdepartmental consultation on 2 full days a week (Mondays and Thursdays); on the remaining 3 weekdays the dermatologist combines consultation with outpatient practice.
The study subjects were patients admitted to Hospital Universitario Virgen del Rocío for whom our department received an interdepartmental consultation request from a specialist in another department. We excluded children (under 14 years of age), patients admitted on the recommendation of a dermatologist, and patients referred for interdepartmental consultation but not attended due to early discharge or any other reason.
Hospital policy allows specialists to contact the dermatologist on duty for interdepartmental consultation through 3 channels: an in-house telephone number (answered from 8AM to 3PM), a consultation request form on paper (submitted via internal mail), and a digital consultation request form (submitted via the hospital's integrated advanced clinical documentation system).
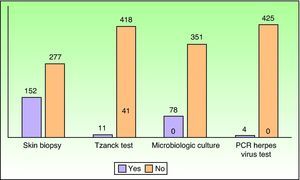
Each day, the dermatologist responsible for interdepartmental consultation and the assigned resident used a standard data collection form to record the following variables: patient administrative and demographic data, requesting department, form of contact, day of the week, complaint, relationship between the skin condition and hospital admission, previous dermatologic consultations, time elapsed between consultation request and first visit, additional tests requested and procedures performed (skin biopsy, Tzanck test, culture, polymerase chain reaction [PCR] herpes virus test), definitive dermatologic diagnosis, previous dermatologic treatment, treatment prescribed by the consultant dermatologist, number of follow-up visits, and discharge destination. The dermatology department responded digitally to all interdepartmental consultation requests via the hospital's integrated advanced clinical documentation system.
The complaints were grouped in the following categories: skin lesions, without further specification; simple lesions or descriptions (rash, exanthema, papules, nodules, etc.); and suspicion of a specific dermatologic diagnosis (acne, psoriasis, intertrigo, etc.). The dermatologic diagnoses were grouped in 7 categories: inflammatory skin conditions, infectious skin diseases, autoimmune and bullous skin conditions, skin tumors, drug-induced dermatoses, trophic disorders, and mucosal disease. Up to 3 diagnoses were allowed per patient.
All patients provided verbal informed consent before being included in the study database, having the lesion photographed, or undergoing a skin biopsy or culture. To ensure confidentiality, all patient data was encoded before it was included in the database.
Prior to analysis, another dermatologist reviewed and verified the data and filled in the standard data collection form. The information was then entered into a spreadsheet (Excel). The data distribution was analyzed and the frequency of each variable was calculated. The SPSS statistical package (version 19.0) was used.
ResultsDuring the 12 months of the study (245 working days), 429 initial interdepartmental consultations took place (mean of 1.75 new patients each day), accounting for 1.56% of all initial consultations in the department during the period. In 257 of the 429 initial consultations, the complaint was resolved with a single visit. The total number of follow-up visits was 495; the number per patient ranged from 1 to 25. During the study period, 752 visits took place (mean, 3 patients each day).
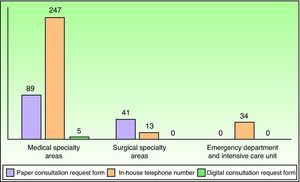
Requests for interdepartmental consultation were made by telephone in 294 cases (68.53%), on paper in 130 cases (30.30%), and via the hospital's computer system in only 5 cases (1.17%). Fig. 1 shows the frequency of each form of contact by the medical, surgical, and intensive care specialty areas.
Most interdepartmental consultation requests were received on Thursdays (166 [38.69%]) and Mondays (109 [25.41%]). The remaining requests were distributed homogeneously across the other days of the week, with 57 (13.29%) received on Wednesdays, 55 (12.82%) on Fridays, and 42 (9.79%) on Tuesdays.
Of the 429 patients, 93% saw a dermatologist on the same day the request was submitted (within 7h), 5.6% were attended within 24hours, and just 1.4% waited longer than 24hours. In 97.56% of the interdepartmental consultations, the patient was attended by a dermatologist and a resident. In 2.43% of the consultations, the patient was attended by a dermatology resident only.
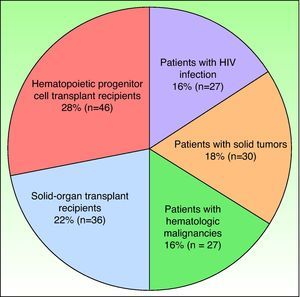
Demographic characteristics of the patients were recorded. The ratio of men to women was 1.21, the mean (SD) age of the patients was 52.63 (19) years; the median age was 54 years. Sixty-two percent of the patients were older than 50 years of age. A total of 166 patients (38.69%) were immunocompromised (Fig. 2).
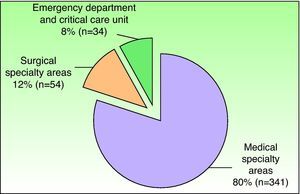
The departments that most frequently consulted a dermatologist are shown in Figs. 3 and 4.
In descending order of frequency, the most common complaints were as follows: skin lesions, without further specification (223 patients); simple lesions or descriptions (rash, exanthema, papules, nodules) (184 patients); and suspicion of a specific dermatologic diagnosis (22 patients).
A total of 114 different diagnoses were established. Inflammatory skin conditions accounted for 35.79% (160 consultations), infectious skin diseases for 25.72% (115), autoimmune and bullous dermatoses for 10.51% (47), tumors for 9.39% (42), drug-induced dermatoses and toxic dermatitis for 8.72% (39), trophic disorders for 7.82% (35), and mucosal disease for 2.01% (9) (Table 1).
Most Common Diagnoses.
| Diagnosis | No. of Patients (%) |
| Inflammatory skin conditions | 160 (35.79) |
| Irritant contact dermatitis/eczema | 11 |
| Eczema | 13 |
| Graft-versus-host disease | 11 |
| Exudative erythema multiforme | 11 |
| Plaque psoriasis | 29 |
| Infectious skin diseases | 115 (25.72) |
| Intertrigo | 20 |
| Herpes simplex virus | 11 |
| Herpes zoster virus | 18 |
| Folliculitis | 9 |
| Cellulitis | 6 |
| Autoimmune and bullous skin conditions | 47 (10.51) |
| Systemic vasculitis | 18 |
| Autoimmune panniculitis | 8 |
| Leukocytoclastic vasculitis | 5 |
| Pemphigoid | 4 |
| Subacute lupus erythematosus | 3 |
| Skin tumors | 42 (9.39) |
| Basal cell carcinoma | 7 |
| Tumor infiltration of the skin | 7 |
| Cutaneous metastasis | 6 |
| T-cell lymphoma | 4 |
| Pyogenic granuloma | 2 |
| Drug-induced dermatoses | 39 (8.72) |
| Toxic dermatitis | 32 |
| Toxic epidermal necrolysis | 4 |
| Drug-induced lichenoid eruptions | 1 |
| Carbamazepine hypersensitivity syndrome | 1 |
| Trophic disorders | 35 (7.82) |
| Excoriations | 9 |
| Venous ulcers | 7 |
| Stasis dermatitis | 5 |
| Pressure ulcers | 3 |
| Calciphylaxis | 3 |
| Mucosal disease | 9 (2.01) |
| Recurrent aphthae | 4 |
| Irritant balanitis | 2 |
| Irritant vulvitis | 3 |
In 187 patients (43.58%), the skin disease was already present prior to hospitalization; in 71 patients (16.55%), it coincided with or was a concomitant reason for admission; and in 171 patients (39.86%), it developed during the hospital stay.
Prior to hospitalization, 63 patients (14.68%) had been assessed for the same condition on an outpatient basis by a dermatologist from our department.
No additional testing was required for 199 patients (46.39%). Fig. 5 shows the most frequently requested additional tests.
The percentage of patients who underwent further testing varied considerably from one consulting department to another. Additional tests were requested for 28 of the 66 patients admitted by the hematology department (42.42%), 15 of the 44 nephrology patients (34.09%), and 2 of the 54 surgical patients (3.70%).
In 183 cases (42.65%), the patient's physician had prescribed treatment for the skin condition prior to the interdepartmental consultation; the remaining 246 patients had received no previous treatment. Table 2 shows the dermatologic treatments prescribed.
Treatments Prescribed by the Dermatologist.
| Treatment Prescribed by Dermatologist | No. of Patients (%) |
| General measures | 30 (7) |
| Topical treatment | 224 (52.21) |
| Systemic treatment | 99 (23.08) |
| Systemic antibiotic therapy | 26 (6) |
| Systemic antiviral therapy | 23 (5.3) |
| Systemic antifungal therapy | 16 (3.73) |
| Surgery | 16 (3.73) |
| Nonsteroidal anti-inflammatory drugs | 7 (1.63) |
The discharge destination varied: 107 patients (25%) of patients were discharged to outpatient dermatology care, 64 (14.92%) to primary care, and 250 (58.2%) to the requesting department. Eight patients (1.9%) died while hospitalized.
DiscussionDermatology is a field in upheaval. Today's dermatologists are branching into a growing number of fields: dermatologic surgery, pediatric dermatology, cosmetic dermatology, phototherapy, and many more. Nevertheless, few dermatologists practice on hospitalized patients in Spain. While several studies on the fundamental role played by dermatologists in interdepartmental consultation have been carried out in other countries,2–14 we have found only 1 such study conducted in a Spanish hospital.15
Our review of the literature revealed 11 relevant articles2–5,7,9–11,13–15 on the role of interdepartmental consultation in dermatology; Table 3 provides a detailed comparison of the findings of these studies.
Comparison of Similar Studies.
| Author and Reference No. | Year | Hospital/Country | No. of Patients | Duration of Study, mo | Requesting Department | Final Diagnosis |
| Sherertz2 | 1984 | Gainesville HospitalUSA | 700 | 12 | Not reported | Cutaneous manifestations of systemic disease 9.4%Drug reactions 9.2%Superficial mycoses 9.1% |
| Hardwick et al.3 | 1986 | Groote Schuur HospitalSouth Africa | 500 | 16 | Internal medicine 45.6%General surgery 10.6% Obstetrics and gynecology 8.4% | Dermatitis 17.1%Drug reactions 10.5%Superficial mycoses 7.0% |
| Arora et al.4 | 1989 | Base HospitalIndia | 662 | Not specified | Internal medicine 49.8%Surgery 22.7%Pediatrics 9.8% | Cutaneous manifestations of systemic disease 23%Drug reactions 9.1% |
| Falanga et al.5 | 1994 | Jackson Memorial HospitalUSA | 591 | 8 | Medicine 39%Emergency 16%Pediatrics 14% | Miscellaneous 48%Drug reactions 8.8%Atopic dermatitis 5.1% |
| Itin7 | 1999 | Kantonsspital AarauSwitzerland | 594 | 12 | Internal medicine>50% | Infectious skin diseases 21.7%Drug reactions 9.8% |
| Fischer et al.9 | 2004 | University HospitalGermany | 2390 | 24 | Internal medicine>42.8%Pediatric medicine 11.7% Neurology 9.9% | Infections 24.4%Candidiasis 23.9%Eczemas 12.4% |
| Walia et al.10 | 2004 | 158 Base HospitalIndia | 971 | 60 | Surgery 29.8%Medicine 29.7%Psychiatry 16.4% | Allergic dermatitis 30.2%Infections 29.8% |
| Antic et al.11 | 2004 | Kantonsspital AarauSwitzerland | 1290 | 36 | Only internal medicine included | Precancerous skin lesions 6.2%Drug reactions 4.2% |
| Maza et al.13 | 2009 | CHU Timone, CHU Sainte-Marguerite,CHU Nord,Hospital Militair LaveranFrance | 352 | 3 | Medicine 60.8%Emergency 11.6%Surgery 10.5% | Infectious skin diseases 34.8%Miscellaneous 26.4%Inflammatory skin conditions 21.7% |
| Mancusi et al.14 | 2010 | Hospital das Clinicas FMUSPBrazil | 313 | 4 | Internal medicine 24%Neurology 12%Cardiology 11% | Infectious skin diseases 25.8%Eczemas 16.6%Drug reactions 14% |
| Peñate et al.15 | 2009 | Hospital Insular de Las PalmasSpain | 3144 | 96 | Internal medicine 21.5%Pediatric medicine 11.4%Neurology 8.3% | Contact dermatitis 8.9%Drug reactions 7.4%Candidiasis 7.1% |
| Lorente-Lavirgen et al. (present study) | 2010-2011 | Hospital Universitario Virgen del RocíoSpain | 429 | 12 | Internal medicine 27%Hematology 15%Surgery 12% | Inflammatory skin conditions 36.2%Infectious skin diseases 26.5%Autoimmune processes 10.10% |
The duration of these studies has varied widely, ranging from 3 months13 to 96 months.15 Our study covered 12 months. Studies were done in a single hospital in several cases, whereas others were multicenter projects, such as that of Maza et al.13 (4 hospitals).
Hospital characteristics have also varied widely in the literature. Because the sample size, population characteristics, study period, and number of facilities studied have been so disparate, it is very difficult to compare the studies.
Another point of difference has been the number of patients enrolled. Our study only included patients for whom an interdepartmental consultation was requested by other specialists and excluded patients hospitalized for exclusively dermatologic conditions. We believe that it is important to differentiate between these 2 types of patients: true dermatologic interdepartmental consultations involve patients who require the care of a dermatologist despite being hospitalized for a different underlying disease.
None of the reviewed studies specifies how interdepartmental consultation was organized within the dermatology department. Because the volume of interdepartmental consultation is highly variable and unpredictable, it is very difficult to organize this activity, especially in combination with outpatient practice. This study enabled us to identify the days of the week with the largest number of interdepartmental consultation requests—Thursday followed by Monday—and assign a dermatologist exclusively to this activity on those days. We believe it is not by chance that Monday and Thursday are the days with the heaviest caseload. The number of consultation requests probably rises on Thursday as a result of preparations for patient discharges ahead of the weekend and rises again on Monday because new patients have been admitted over the weekend.
Despite the difficulty of combining interdepartmental consultation with outpatient practice, more than 90% of patients were attended on the day the request was submitted. Similar results have been reported in other studies.13,14 Moreover, our procedures give priority to interdepartmental consultation requests for patients in the hematology, nephrology, emergency, and intensive care units as well as immunocompromised patients and those in whom the attending physician suspects a serious skin disease. Ensuring early medical attention for these patients requires good work organization, a dermatologist on duty who prioritizes interdepartmental consultation, and the availability of an in-house telephone number.
Only 3 of the 11 studies we analyzed report the number of visits per patient. Complaints were resolved with a single visit in 85% of cases in the study by Fischer et al.,9 in 71.8% of cases in the study by Peñate et al.,15 and in 58% of cases in the study by Mancusi et al.14 Our findings are consistent with these figures. We therefore conclude that most interdepartmental consultations are requested for common, nonserious, easy-to-manage diseases. This conclusion is corroborated by the fact that most of the prescribed treatments were topical agents and that just one-fourth of the patients required outpatient follow-up care after discharge.
None of the reviewed studies specify the means by which the dermatologist responsible for interdepartmental consultation was contacted. Fig. 1 shows that most requests in our study were made by telephone, especially by doctors in medical specialty areas, the emergency department, and the intensive care unit. However, other channels were preferred by doctors in surgical specialty areas, except for the plastic surgery department. This exception may be attributable to the fact that our department works closely with the plastic surgery department in routine clinical practice. The availability of an in-house telephone number answered throughout the workday makes it easy for other specialists to contact a dermatologist, helps patients with serious diseases gain quick access to medical attention, and encourages the attending physician and the dermatologist on duty to share ideas. Moreover, we believe that the use of pagers is essential to providing a good interdepartmental consultation service.
The demographic characteristics of the patients (sex and age) were consistent with those of the hospitalized population at our facility during the study period.1 Our results corroborate those of earlier studies in which the medical specialty areas—especially internal medicine—accounted for a large proportion of dermatologic interdepartmental consultations.3,7,9,10,13–15 The reviewed studies generally found that medical specialty areas request consultation more frequently than surgical specialty areas, probably due to the fact that hospital stays are longer in those departments and the patients are more likely to have multiple conditions and be taking multiple medications. The previous studies found that internal medicine (ranking first) was generally followed in frequency of consultation requests by the pediatric, emergency, and neurology departments.3,7,9,10,14,15
In this study, we excluded pediatric patients because a pediatric dermatologist was responsible for both pediatric outpatient care and interdepartmental consultations. Moreover, we believe that because children have specific characteristics, the management of their conditions should be assessed in a different type of study. It is worth noting that although departments such as hematology, nephrology, and infectious disease requested fewer interdepartmental consultations than internal medicine, the patients in those departments required more follow-up visits and additional tests. This difference is undoubtedly due to the greater complexity of these patients, most of whom have immune deficiency diseases or are transplant recipients. Immunocompromised patients accounted for a large proportion (over a third) of all interdepartmental consultations.
The most common complaints were consistent with those reported elsewhere.13 Nonspecific skin lesions or conditions such as a skin rash causing itching accounted for most complaints. In descending order of frequency, the most common diagnoses reported in similar studies are infections, inflammatory skin conditions, and drug reactions.3,7,9,13–15 In our study, the most common diagnoses were inflammatory skin conditions followed by infectious skin diseases. Drug reactions comprised the fifth most common diagnostic category, after autoimmune dermatoses and tumors. Nevertheless, if the specific diagnoses are considered individually rather than as categories, the most common diagnosis was toxic dermatitis.
Autoimmune processes were unusually frequent in our study, a finding which is attributable to the separate category we established for them given that our hospital's internal medicine department is home to a leading collagen disease unit; in contrast, other researchers generally counted them as inflammatory skin conditions. In general, it is difficult to compare the frequencies of specific diseases in the reviewed studies because the classification and quantification criteria were not uniform. Generally speaking, however, intertrigo was the most frequently diagnosed infectious skin disease and eczema the most common inflammatory skin condition.3,7,9,13–15 In our study, eczema and plaque psoriasis were the most common inflammatory conditions. In the category of infectious skin diseases, the most common diagnosis was candidal intertrigo, followed by herpes zoster virus reactivation.
We were interested in examining the relationship between the onset of the skin disease and the reason for hospitalization. Skin lesions can be the first manifestation of severe systemic disease. This was the case in the 5 kidney transplant recipients with generalized herpes zoster, the 7 patients with malignant tumor infiltration of the skin, and the 2 patients with septic fungal vasculitis; for these patients, the skin condition was an indication for hospitalization.
In the reviewed literature, the percentage of patients who required additional testing ranged from 6.4% (Peñate et al.15) to 48% (Mancusi et al.14); our findings were consistent with the latter figure. The proportion of patients requiring additional testing varied substantially by requesting department: far more tests were requested for patients referred by the hematology and nephrology departments than for patients referred by the surgical specialty areas. As noted above, we believe that this difference can be attributed to the fact that the aforementioned medical departments handle complex patients with severe underlying disease (transplant recipients, other immunocompromised patients, etc.).
It is also interesting to know whether the patients had been treated prior to the consultation request. Previous treatment was generally a disadvantage because it sometimes produced artifacts in the lesions, making final diagnosis more difficult.
Only 25% of the patients required follow-up care after discharge; most complaints were resolved satisfactorily during hospitalization.
Our study had several limitations:
- 1
We had to categorize complaints that were highly varied and, in most cases, not very specific. The lack of common criteria for classifying complaints makes it difficult to compare our findings with those of previous studies.
- 2
The diagnoses were determined by a single dermatologist or by a dermatologist and a resident and were not subsequently verified, except in cases in which a biopsy or culture was performed.
- 3
Because our hospital is made up of several physically separate buildings, specialists in different areas often have little contact with one another. As a result, some units may not request interdepartmental consultation because they are unaware that this service is available. This hypothesis might explain why the otolaryngology department made no interdepartmental consultation requests and the cardiology and urology departments made very few.
Irrespective of our data and results, we believe that residents’ participation in an activity that forms an integral part of hospital care but that is organized by the dermatology department is a valuable training exercise because it provides contact with hospitalized patients as well as the opportunity to observe acute, serious conditions in patients not seen in an outpatient setting, such as transplant recipients and intensive care patients.
We believe it may be possible to extrapolate our findings to other Spanish tertiary care hospitals that serve populations with similar characteristics. Because skin complaints are highly prevalent in hospitalized patients, the incorporation of a consultation service in the daily activity of dermatology departments could improve inpatient care in all types of hospital.
In conclusion, our results suggest that hospitals should promote inpatient dermatology consultation. By playing an integral role in evaluating acute skin conditions that coincide with or arise during hospitalization, dermatologists improve inpatient care and decrease comorbidity during hospital stays.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
We are grateful to the dermatology department of Hospital Universitario Virgen del Rocío for helping with data collection.
Please cite this article as: Lorente-Lavirgen AI, et al. Interconsulta hospitalaria en Dermatología sobre una cohorte prospectiva en un hospital español de tercer nivel. Actas Dermosifiliogr. 2013;104:148–55.