Hailey-Hailey disease (HHD) or familial benign chronic pemphigus is a rare skin disorder characterized clinically by vesicles and erosions in the intertriginous areas, mainly the axillas and groin.1–4 The site of the lesions, the pain, and sometimes their smell have a marked impact on patients’ quality of life5; this has led to the use of numerous medical and surgical treatments, with variable degrees of success. We present a patient with long-standing, extensive HHD who presented an excellent response to doxycycline.
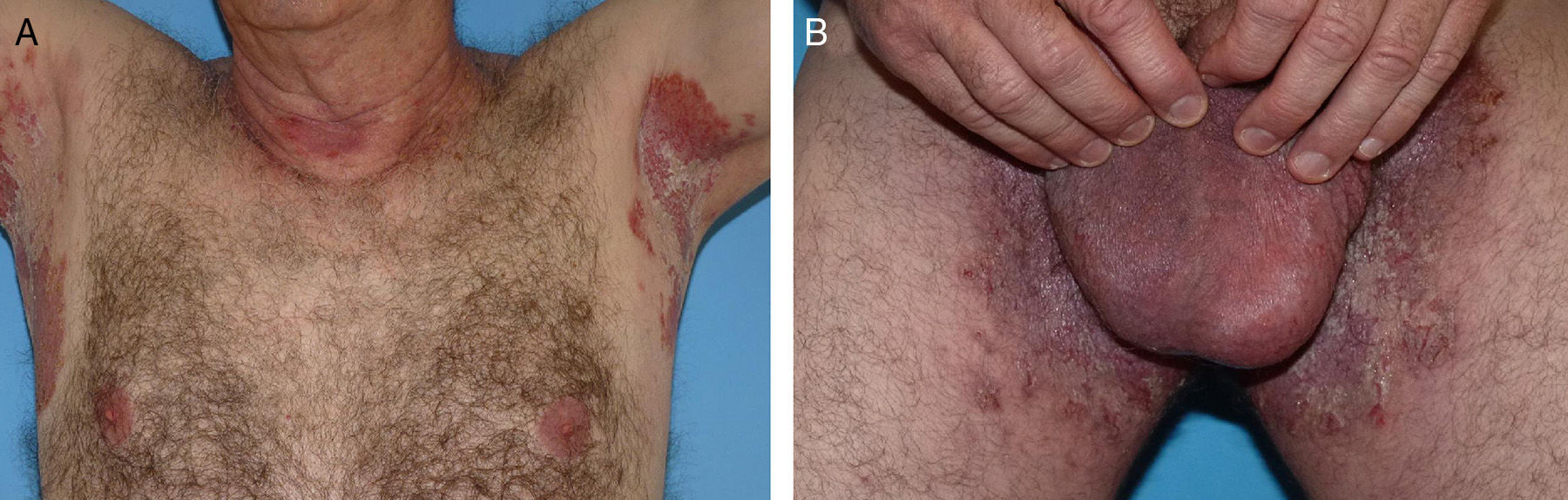
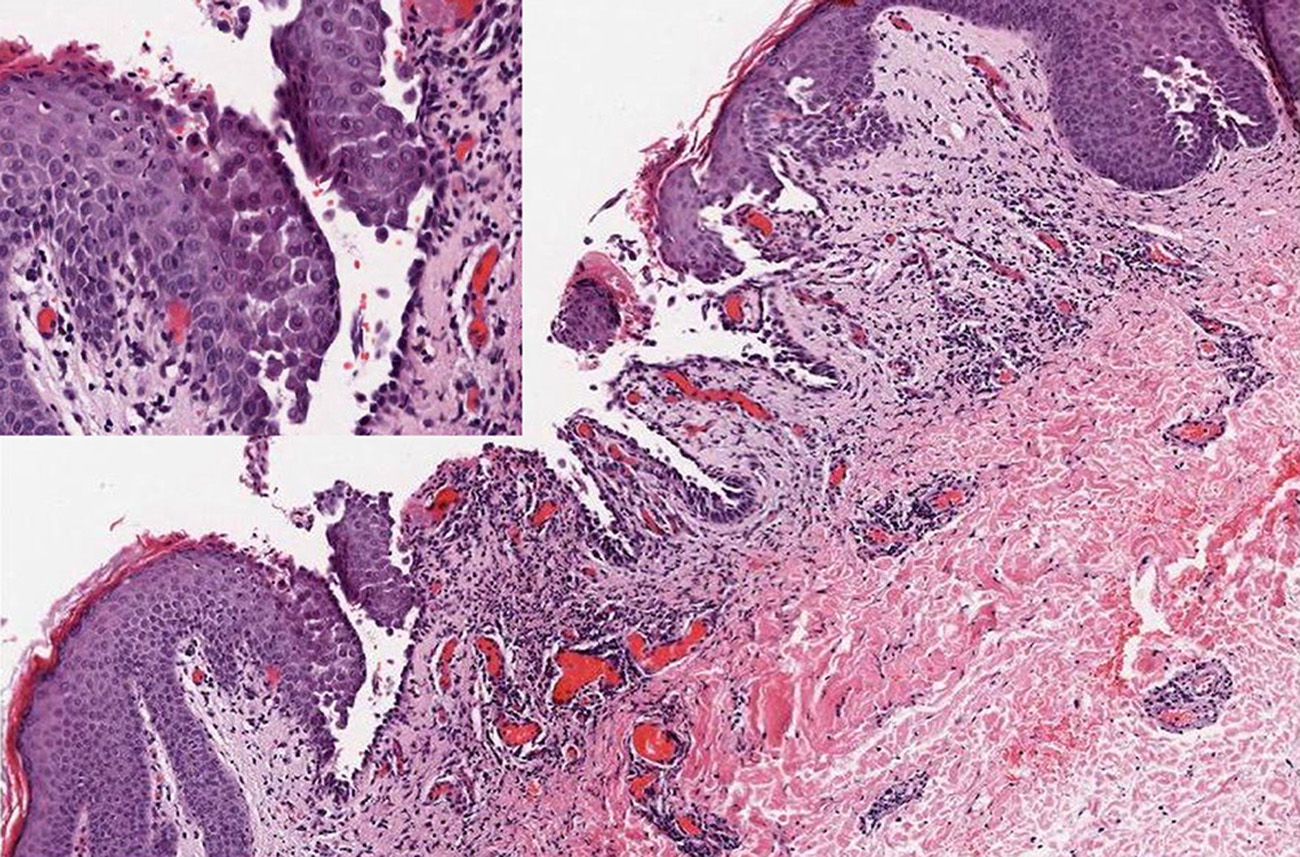
A 60-year-old man with no past history of interest was referred from another health area for a recurrent dermatosis that had arisen 20 years earlier and affected the skin folds. He presented crusted, exudative, erosive-vesicular lesions in the skin folds, particularly the axillary and inguinal folds (Fig. 1), the cubital fossa, neck, and perineum. The lesions were pruritic and painful and became worse during the summer and with exercise. He had previously been treated with corticosteroids and topical antibiotics with little improvement. The patient reported no family history of skin disease, though the youngest of his 4 offspring (2 women and 2 men) presented similar but milder lesions on the neck and in the axillas. Biopsy confirmed the diagnosis of HHD (Fig. 2). Direct immunofluorescence was negative. Routine blood tests were normal and antinuclear antibodies and indirect immunofluorescence for anti-intercellular cement substance and antibasement membrane zone antibodies) were negative.
Treatment was prescribed with doxycycline at a dose of 100mg/d. This was very well tolerated and led to a rapid improvement that was maintained throughout the summer months. The dose was then reduced to 50mg/d. After 16 months of follow-up on the same dose, the patient remained asymptomatic (Fig. 3).
HHD is a rare chronic genodermatosis of autosomal dominant inheritance. It is caused by mutations in the ATP2C1 gene on chromosome 3q21-24. Mutations of this gene, which codes for the secretory pathway Ca++/Mn++-ATPase (SPCA1) of the Golgi apparatus, cause changes in calcium-dependent intracellular signals, producing a loss of cell adhesion in the epidermis, leading to acantholysis.1–3 The exact mechanism of the changes remains unclear.2,3
HHD has been treated with varying degrees of success using a variety of treatments aimed at mitigating the inflammation or reducing the triggering factors; treatments reported in the literature include topical and systemic corticosteroids, topical antibiotics, oral retinoids, immunosuppressants such as ciclosporin and methotrexate, dapsone, botulinum toxin, oral glycopyrrolate, dermabrasion, various lasers, and photodynamic therapy.6
Tetracycline, doxycycline, and minocycline have been used with success in dermatology, exploiting their nonantimicrobial effects as anti-inflammatory agents (inhibition of leucocyte chemotaxis and activation and regulation of inflammatory cytokines in keratinocytes) and their anticollagenase activity via inhibition of the dermal matrix metalloproteinases. Metalloproteinase 9 and its inhibitor have been implicated in HHD and in Darier disease.7,8
The recent publication of 6 cases of HHD with a dramatic response to doxycycline,7 with ease of access and management, low cost, and few side effects, led us to use this drug. The treatment achieved an excellent response never before experienced by our patient either spontaneously or with other topical treatments (dermal corticosteroids and fusidic acid).
Conflicts of InterestThe authors declare that they have no conflicts of interest
Please cite this article as: Flores-Terry MÁ, Cortina-de la Calle MP, López-Nieto M, Cruz-Conde de Boom R. Enfermedad de Hailey-Hailey, adecuada respuesta a doxiciclina. Actas Dermosifiliogr. 2016;107:537–539.