First described by Kossard1 in 1994, frontal fibrosing alopecia is a type of cicatricial alopecia that is clinically characterized by progressive and symmetrical recession of the frontotemporal hairline. It is accompanied by partial alopecia of the eyebrows in most cases2 and loss of body hair in a variable number of patients.3 It is more frequent in postmenopausal women, although there have been reports of cases in men and premenopausal women.2,4 Histopathology shows it to be a variant of lichen planopilaris, which is characterized by a reduced number of hair follicles, a perifollicular lymphocytic inflammatory infiltrate, and fibrosis.5 Few published studies describe the dermoscopic features of frontal fibrosing alopecia.6,7
We report the case of a 51-year-old woman who consulted with a 12-month history of hair loss at the frontal hairline. No other symptoms or associated diseases were present. Physical examination revealed a bald patch in the form of a band that delimited the hairline of the frontal region (Fig. 1). She also had partial alopecia of the eyebrows. The remaining findings were normal. The patient had previously taken high-potency topical corticosteroids and 2% minoxidil with no signs of improvement.
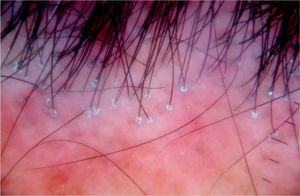
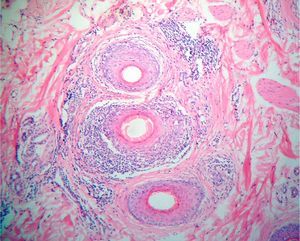
Dermoscopy (Dermlite 00 multispectral) highlighted a marked reduction in the number of follicular ostia in the central area and erythema, perifollicular desquamation, and perifollicular blue-gray dots at the border of the patch (Fig. 2). A biopsy specimen was taken, and histopathology revealed a marked reduction in the density of the pilosebaceous units, as well as laminar fibrosis and a perifollicular lymphocytic inflammatory infiltrate around the isthmus and infundibulum (Fig. 3). The clinical, dermoscopic, and histopathologic findings confirmed a diagnosis of frontal fibrosing alopecia.
Since it was first described in 1994, just under 200 cases of frontal fibrosing alopecia have been reported throughout the world.1,2,4 Although initially considered an uncommon entity, this condition is believed to be a much more common cause of cicatricial alopecia than previously thought.2 There are few published reports of dermoscopic findings in patients with this condition. Several dermoscopic findings are characteristic of frontal fibrosing alopecia, whereas others also appear in other types of cicatricial alopecia, such as discoid lupus erythematosus or lichen planopilaris. Inui et al.6 reported 3 dermoscopic findings in 4 patients with frontal fibrosing alopecia, namely, reduced follicular ostia, erythema, and perifollicular scale, which were also found in the case we report. Other dermoscopic findings also reported in patients with this condition include ramified capillaries, honeycomb-like pigment network, white patches, white dots, and vellus hair.7 In the present case, we also identified blue-gray dots around some follicles, a finding that has previously been reported in discoid lupus erythematosus, but not in frontal fibrosing alopecia.7 Although no studies have established a correlation between dermoscopic findings and histopathologic findings in cicatricial alopecia, it has been suggested that the white patches correspond to fibrosis and that they are more commonly found in long-standing bald patches.7 The blue-gray dots correspond to melanophages in the papillary dermis and the white dots to pigment incontinence7; the honeycomb pattern is the result of exposure of the bald patches to sunlight.8 Erythema and hyperkeratosis are the results of inflammation in the follicle and the hyperkeratosis that develops in lichen planopilaris and frontal fibrosing alopecia.8
Dermoscopic criteria are proving useful in the diagnosis of alopecia.9 In the present case, dermoscopic findings enabled us to rule out other causes of alopecia, such as alopecia areata. The correlation between clinical findings, dermoscopic findings, and histopathologic findings enabled us to establish a diagnosis of frontal fibrosing alopecia.
To date, no cases of frontal fibrosing alopecia have been reported in Latin America. Although this condition has characteristic manifestations, dermoscopy provides more detailed information. The present case underlines the role of dermoscopy for evaluating cicatricial alopecia and establishing a differential diagnosis.
Please cite this article as: Mireles-Rocha H, et al. Alopecia frontal fibrosante. Hallazagos dermatoscópicos. Actas Dermosifliogr. 2012;103:167–8.