Cutaneous metastases (CMs) account for 2% of skin tumors and their incidence varies between 0.7% and 9% in patients with cancer. The objective of this study was to describe and analyze the demographic, clinical, and histopathologic characteristics of CM in patients who visited 2 hospitals in the Santiago de Chile metropolitan region.
Material and methodsWe performed a retrospective, descriptive, analytical, observational, cross-sectional study. We reviewed the pathology reports, patient records, pathology slides, and dates of death for diagnosed cases of CM from the anatomic pathology departments of 2 hospitals in the Santiago de Chile metropolitan region between 2015 and 2017.
ResultsNinety-six patients with CM were included in the study; 60.42% were women and 39.58% were men. The mean (SD) age was 67.95 (13.74) years, with a range of 28 to 96 years. The most common primary tumor was melanoma in 27.08% of cases (n=26), followed by breast cancer (18.75%, n=18), and adenocarcinoma (15.63%, n=15). The median time between diagnosis of the tumor and cutaneous metastasis was 9 months. Patients with CM of melanoma had a higher survival rate than patients with metastasis of other primary tumors (P<.05). A histopathologic study of 91 slides showed that diffuse infiltration of the tissue with tumor cells was the most common pattern and vascular invasion was rare.
ConclusionsThe results are similar to those found worldwide. CM is a rare manifestation of internal tumors. It presents mainly at an advanced age and is equally prevalent in both sexes.
Las metástasis cutáneas (MC) constituyen el 2% de los tumores cutáneos, y su incidencia varía entre el 0,7% y el 9% de los pacientes con cáncer. El objetivo de este estudio es describir y analizar las características demográficas, clínicas e histopatológicas de las MC en población consultante de 2 hospitales de la Región Metropolitana.
Material y métodoEstudio retrospectivo, descriptivo, analítico, observacional y transversal. Se revisaron los informes histopatológicos, fichas, láminas histopatológicas y fechas de defunción de los casos con diagnóstico de MC del servicio de anatomía patológica de 2 hospitales de la Región Metropolitana entre los años 2005 y 2017.
ResultadosSe incluyeron 96 casos de MC. El 60,42% fueron mujeres y el 39,58% hombres. La edad promedio al momento del diagnóstico fue de 67,95±13,74 años, con un rango de 28 a 96 años. La fuente neoplásica primaria más frecuente fue melanoma en el 27,08% (n=26), seguido de carcinoma de mama 18,75% (n=18) y adenocarcinoma 15,63% (n=15). La mediana de tiempo entre el diagnóstico del tumor y la metástasis cutánea fue de 9 meses. Los pacientes con MC de melanoma presentaron una mayor sobrevida que aquellos con metástasis de otro origen (p<0,05). El examen histopatológico de 91 láminas mostró con mayor frecuencia una infiltración difusa del tejido con células tumorales y con baja frecuencia la presencia de permeación vascular.
ConclusionesLos resultados obtenidos se asemejan a la realidad internacional. Las MC son poco frecuentes, constituyendo una rara manifestación de neoplasias internas, se presentan principalmente a edades avanzadas y en ambos sexos por igual.
Cutaneous metastasis is the result of malignant cell spread from a primary tumor to the skin.1 It is a manifestation of systemic spread and can present as the first clinical sign of disease or as a sign of recurrence or advanced disease.2 The tumor cells can originate from an internal tumor or a primary skin cancer.
Cutaneous metastasis has a variable incidence, with rates ranging between 0.7% and 9% depending on the series.3 It accounts for 2% of all cutaneous tumors.4 Its incidence has grown for a number of reasons, including longer patient survival, better treatment options, and a higher average life expectancy among the general population.
Diagnosis is based on the integration of clinical findings and pathologic features identified in the affected skin. In most cases, the metastatic cells have similar histologic features to those seen in the primary tumor. Because these cells may be anaplastic and poorly differentiated, it is sometimes only possible to classify the lesions in general terms, such as a poorly differentiated tumor with features consistent with carcinoma, melanoma, sarcoma, or a hematolymphoid neoplasm. Immunohistochemical studies are useful in such cases, but pathognomonic markers are not always available.5
The main aim of this study was to analyze the characteristics of cutaneous metastases in patients from 2 high-level hospitals in Santiago de Chile, Chile. The specific aims were to characterize demographic, clinical, and histopathologic features, analyze the association between clinical and histopathologic features, and describe overall survival rates.
Material and MethodsWe conducted a descriptive, analytical, retrospective, observational, cross-sectional study.
The study was approved by the scientific-ethics committee for both hospitals.
Cases were identified by searching through pathology reports issued between January 2005 and July 2017. Cases in which skin involvement was due to local tumor extension were excluded. We collected personal and clinical information from the patients’ medical records and then reviewed the pathology slides and obtained dates of death from the national death registry.
Anonymity was ensured by assigning a consecutive number to each patient as they were included in the study (e.g. 1, 2, 3). All data thereafter were processed only by the lead investigator, who was blinded to the identity of the patients at all times, guaranteeing thus full anonymity.
To be included, patients had to have been diagnosed with cutaneous metastasis in the pathology departments of Hospital Clínico de la Universidad de Chile and Hospital Barros Luco Trudeau between January 2005 and July 2017.
Statistical AnalysisNormality of distribution of continuous variables was assessed using the Shapiro-Wilk test. Qualitative variables were expressed as absolute numbers and percentages. Categorical variables were compared using the exact Fisher exact, while continuous variables were compared using the t test for unpaired samples. Multiple comparisons of continuous variables were performed using the Kruskal-Wallis test.
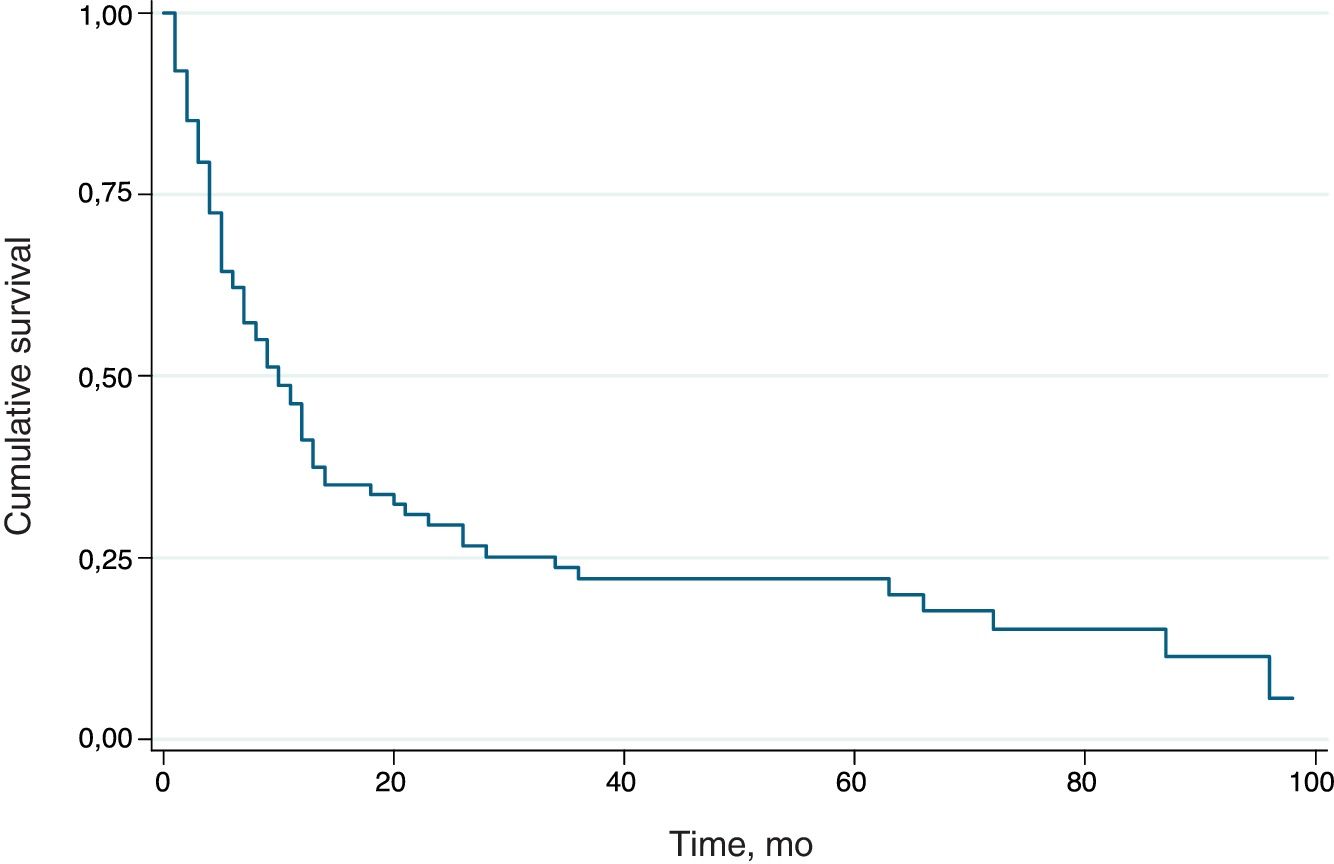
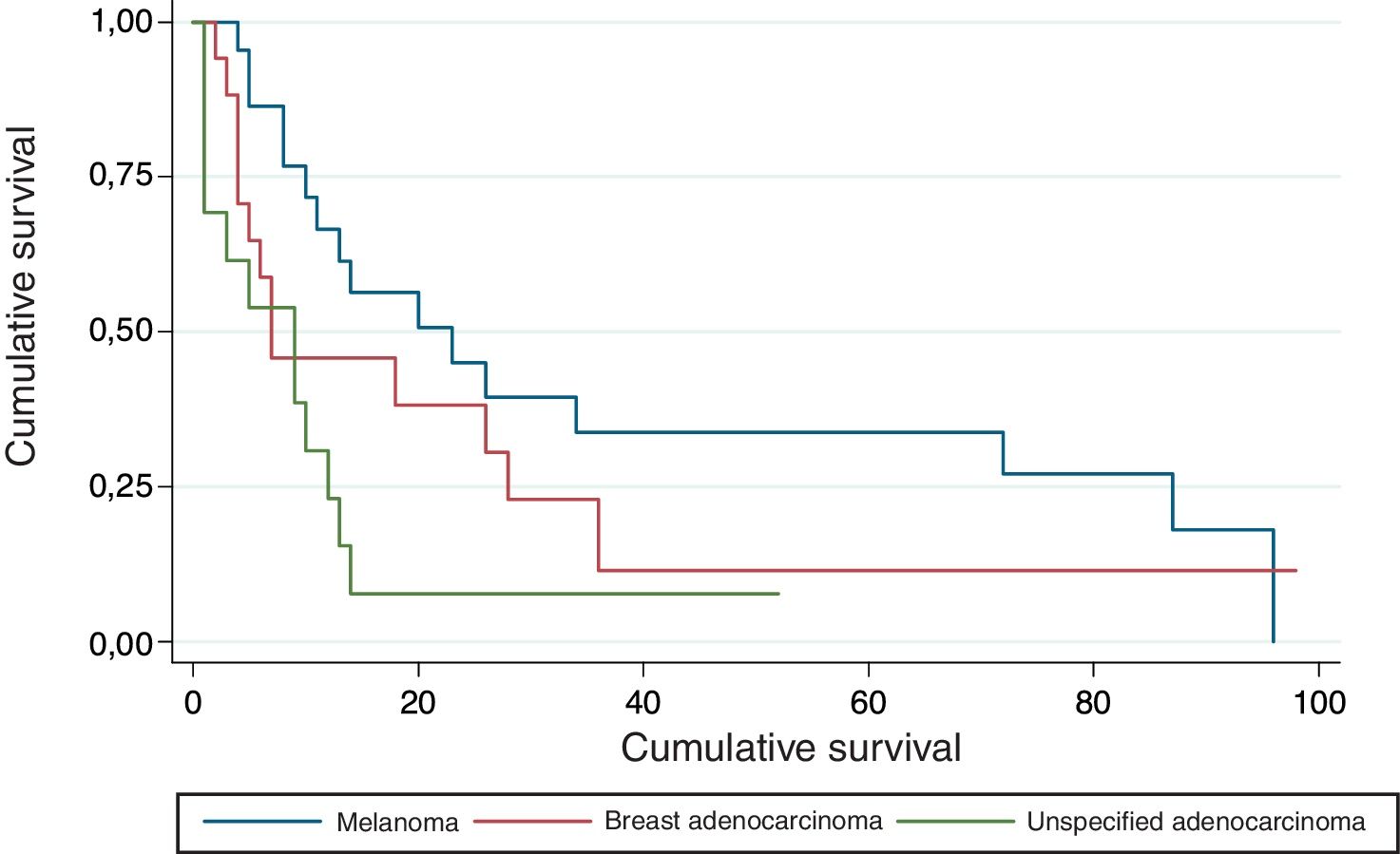
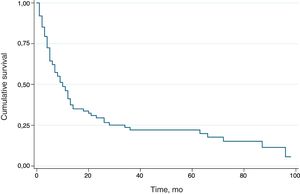
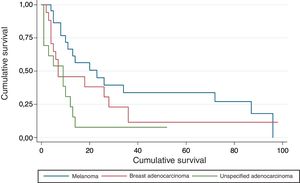
Survival was analyzed using Kaplan-Meier curves and the nonparametric log rank test was applied to analyze differences according to categorical variables.
A statistical significance of P = .05 was established. Statistical analysis was performed using Stata 12 (StataCorp LP).
ResultsSex. We identified 96 pathology reports for 93 patients: 38 from Hospital Clínico de la Universidad de Chile and 58 from Hospital Barros Luco Trudeau. Fifty-eight patients (60.42%) were women and 38 (39.58%) were men.
Age. Mean (SD) age was 67.95 (13.74) years (range, 28-96 years). A majority of patients were observed in the 60-to-80 group. Mean age according to sex was 70.05 (13.32) years for women and 64.72 (13.94) years for men.
Comorbidities. The most common comorbidities were hypertension (29.03%, n=27), type 2 diabetes mellitus (13.98%, n=13), and hypothyroidism (3.23%, n=1).
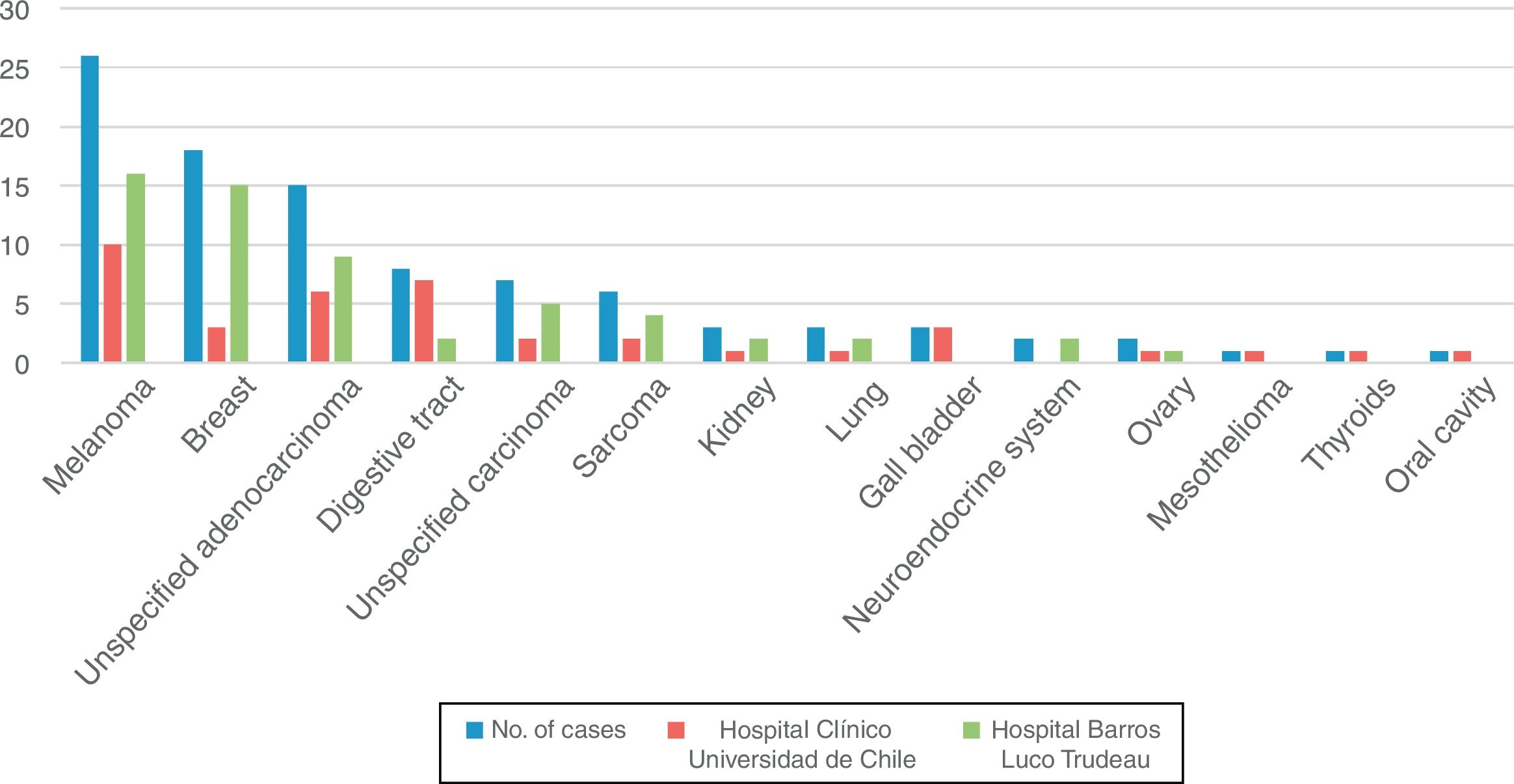
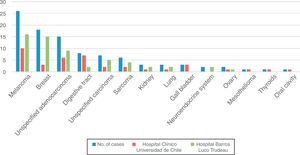
Diagnosis. According to the pathology reports, the cutaneous metastases originated from melanoma in 26 cases (27.08%), breast adenocarcinoma in 18 (18.75%), unspecified adenocarcinoma in 15 (15.63%), digestive tract carcinoma (esophagus, stomach, small intestine, colon, rectum, and anus) in 8 (8.33%), unspecified carcinoma in 7 (7.29%), sarcoma in 6 (6.25%), renal cell carcinoma, lung carcinoma, and gallbladder carcinoma in 3 cases each (3.13%), neuroendocrine carcinoma and ovarian carcinoma in 2 cases each (2.08%), and mesothelioma, thyroid carcinoma, and oral cavity carcinoma in 1 case each (1.04%). Figure 1
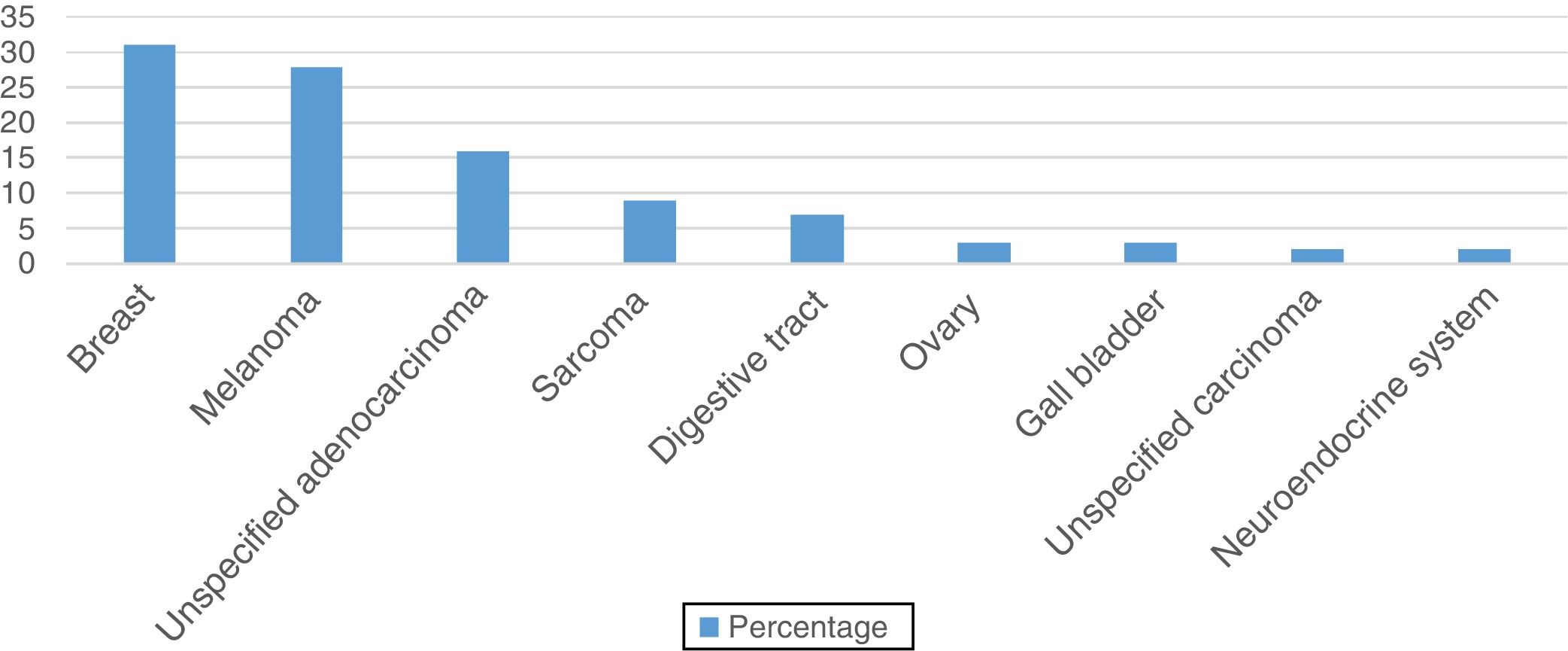
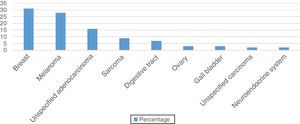
The distribution of diagnoses varied significantly according to sex (P<.001). In the group of women (58 pathology reports), the cutaneous metastases originated from breast adenocarcinoma in 31.03% of cases (n=18), melanoma in 27.59% (n=16), and unspecified adenocarcinoma in 15.52% (n=9) (Figure 2).
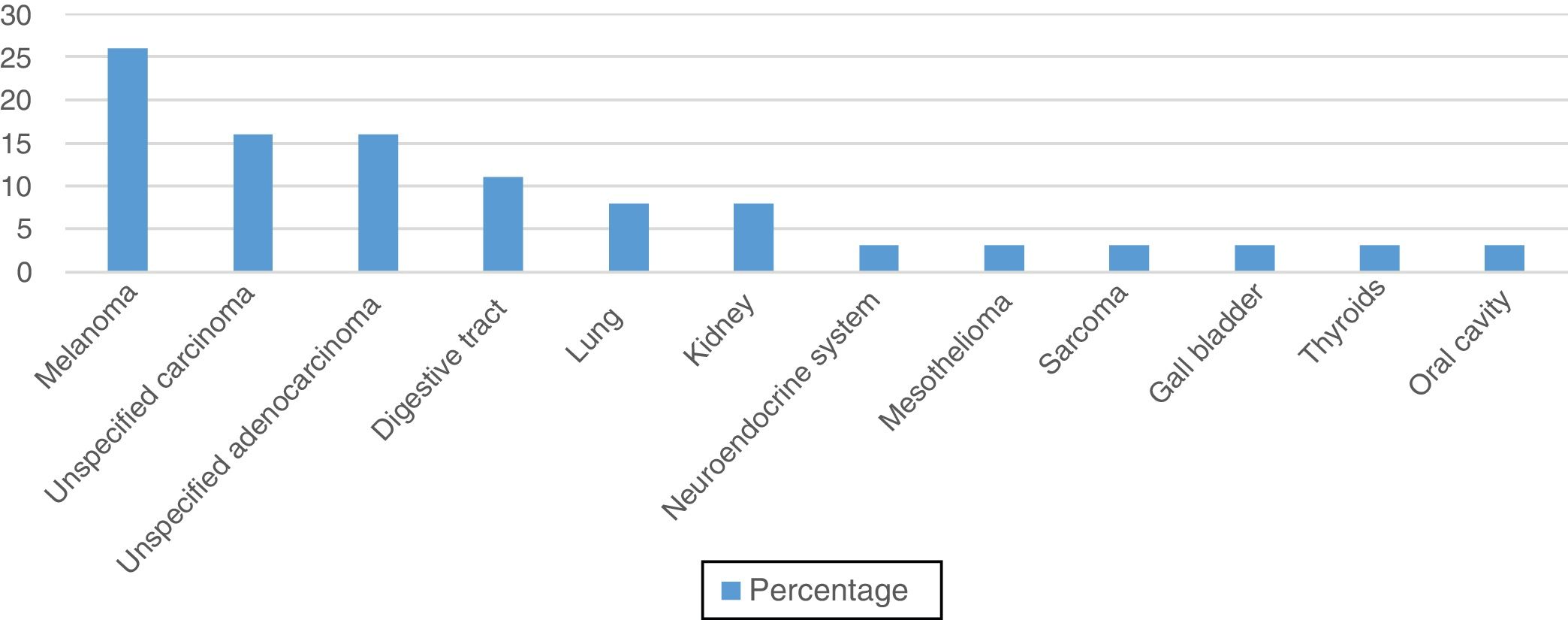
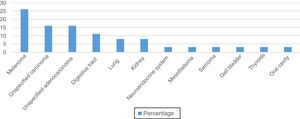
In the male group (38 pathology reports) the main primary tumors were melanoma (26.32%, n=10), unspecified adenocarcinoma (15.79%, n=6), and unspecified carcinoma (15.79%, (n=6) (Figure 3).
Clinical ManifestationsThe cutaneous metastases were mostly located on the abdomen (29.51% of cases) followed by the extremities (29.03%), the thorax (27.87%), the head and neck (22.95%), and the back (9.84%). For metastases from melanoma, the most common locations were the extremities (58.82%), the head and neck (17.65%), and the back (11.76%).
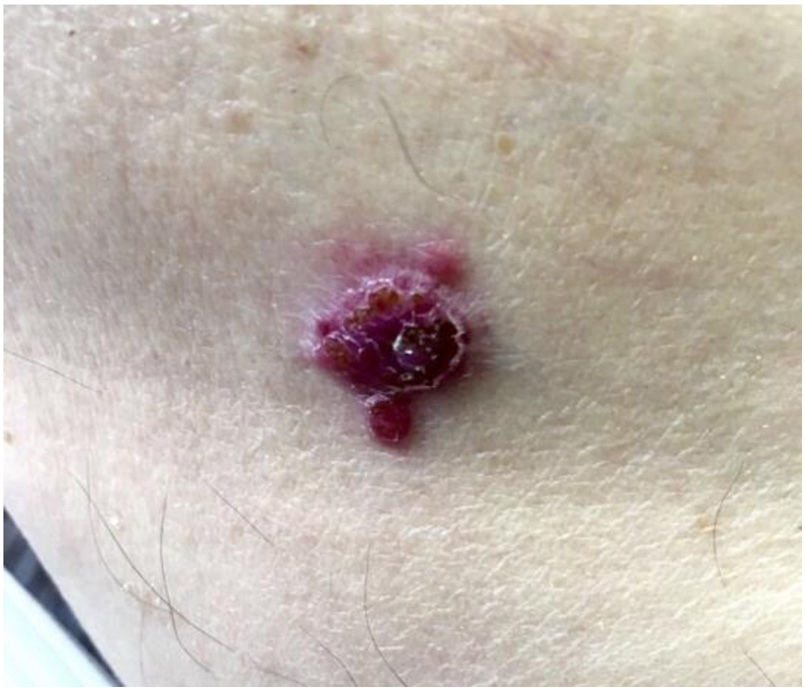
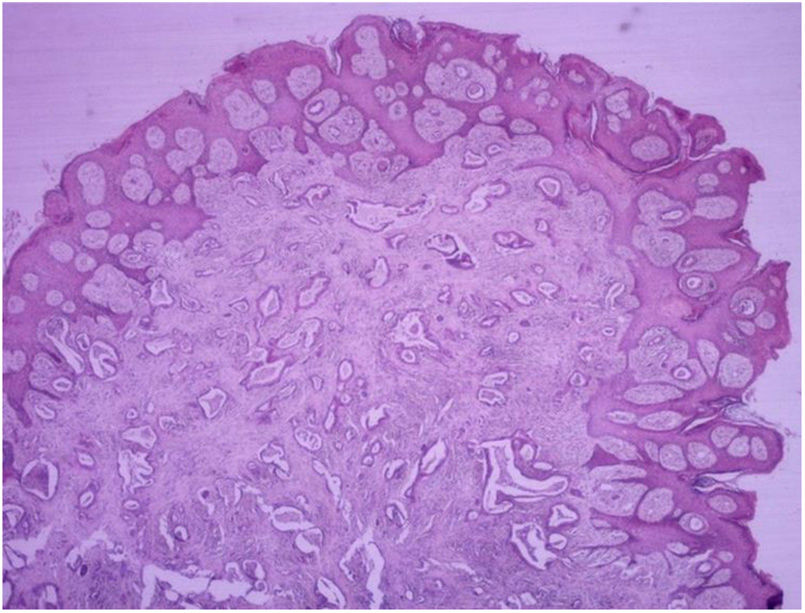
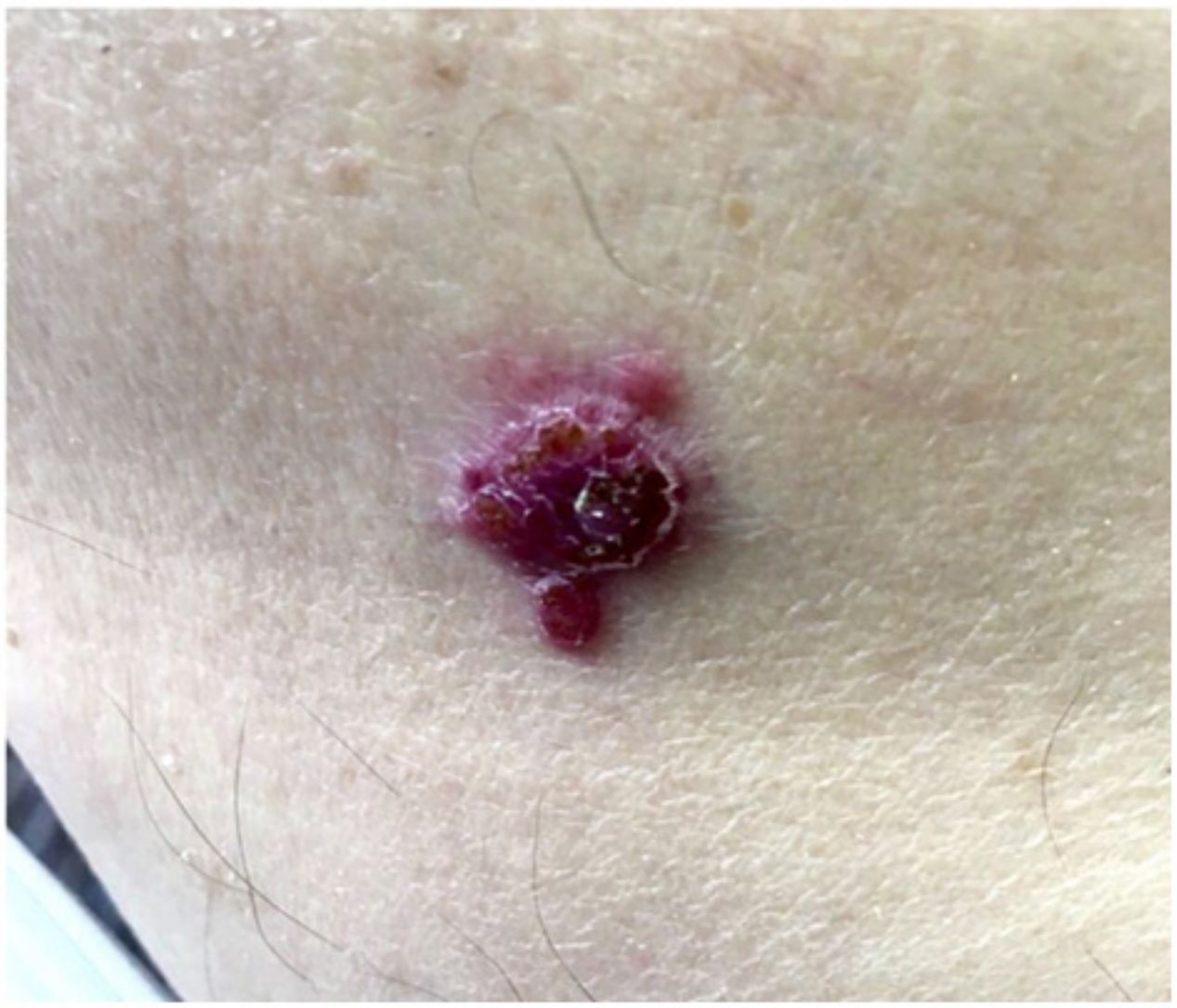
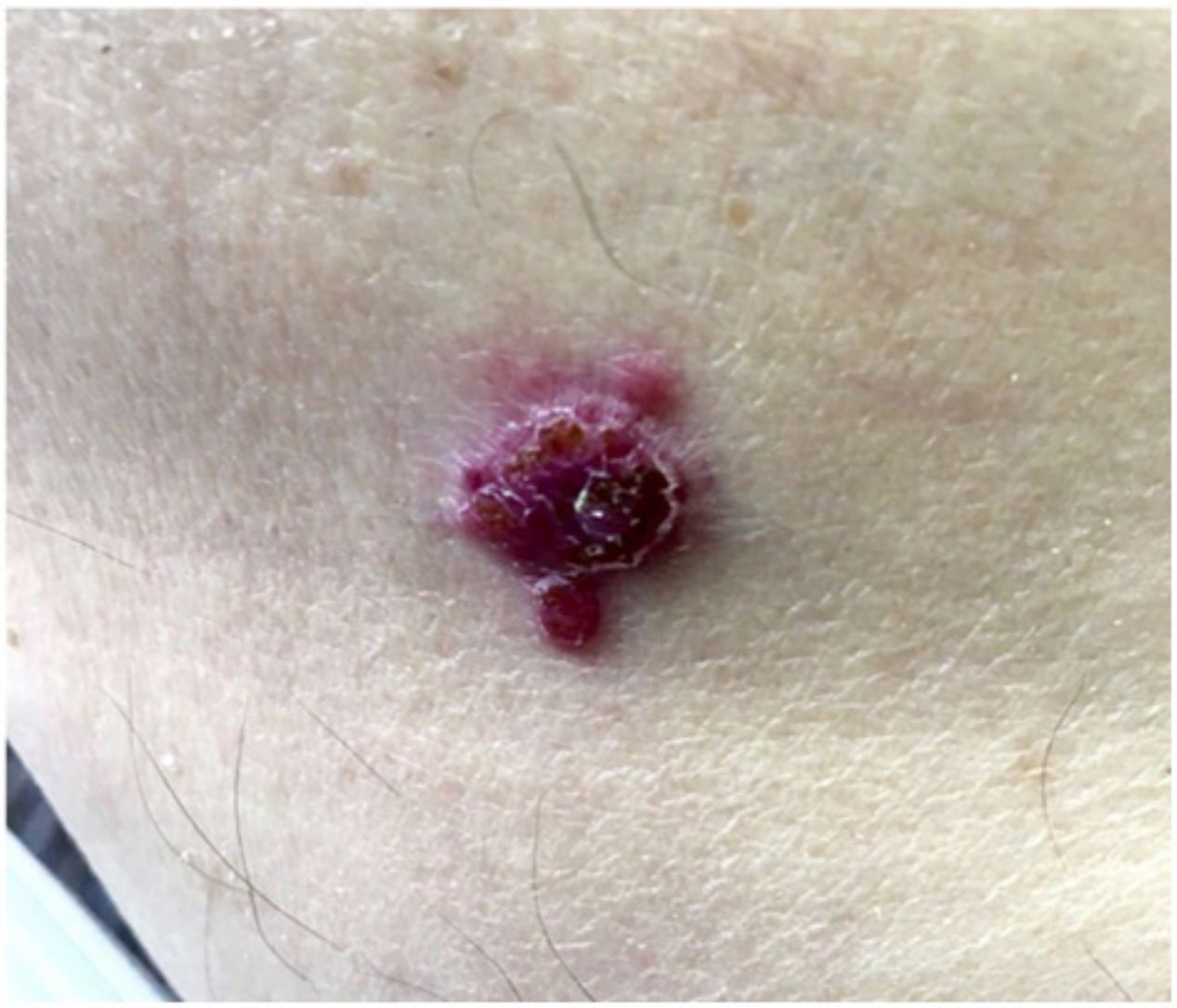
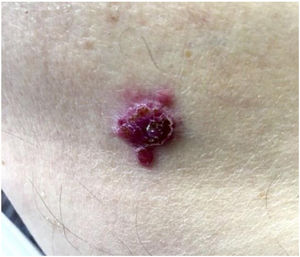
Patient-reported manifestations were highly variable. The main manifestations reported were nodules, plaques, tumors (solid lesions >1cm), and macules. They appeared as solitary or multiple lesions (≥2), some with an ulcerated surface and/or pigmentation. They were largely painful, but some were asymptomatic. Photographs of 2 of the lesions are shown in Figures 4 and 5.
Stony hard tumor with a papillary surface on the lateral aspect of the left foot. Histopathologic findings consistent with a moderately differentiated tubular adenocarcinoma. Integration of these findings with the information from the patient's medical record led to a diagnosis of gall bladder adenocarcinoma.
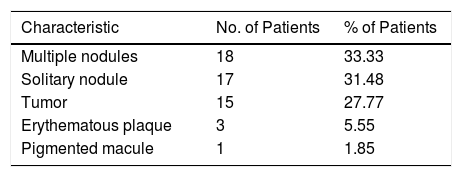
The skin lesions were described for 54 cases. In the remaining cases, a description was missing from the file or this was not available. The results are summarized in Table 1.
SurvivalOverall survival and potential predictors were analyzed using Kaplan-Meier curves. The overall survival curve for the group is shown in Figure 6. Median survival, calculated using the log-rank test, was 10 months.
The survival curves according to primary tumor site are shown in Figure 7. Median survival was 23 months for melanoma, 7 months for breast adenocarcinoma, and 9 months for unspecified adenocarcinoma. Survival was significantly longer in patients with metastasis from melanoma than from either breast or unspecified adenocarcinoma (P=.024).
Median survival according to time of presentation was 5 months for metastases detected before the primary tumor and 10 months for those detected after detection. The difference was not statistically significant (P=.134).
Mean survival according to time of presentation in the case of melanoma was 5 months for metastases detected before the primary tumor and 34 months for those detected later (P=.074).
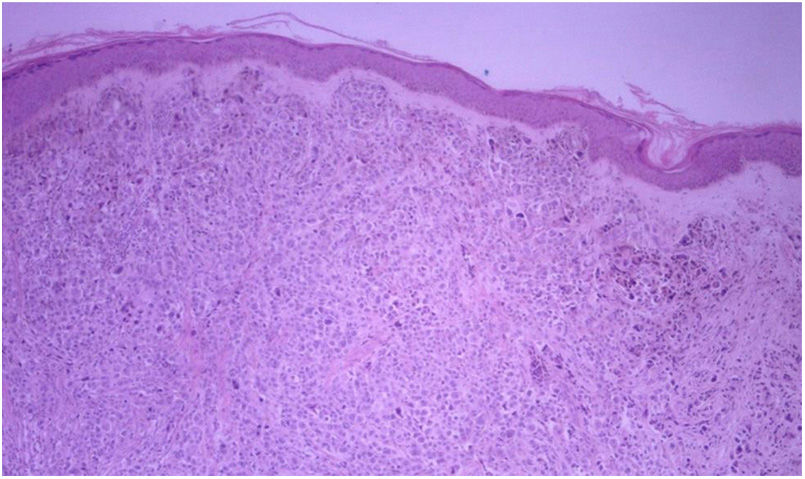
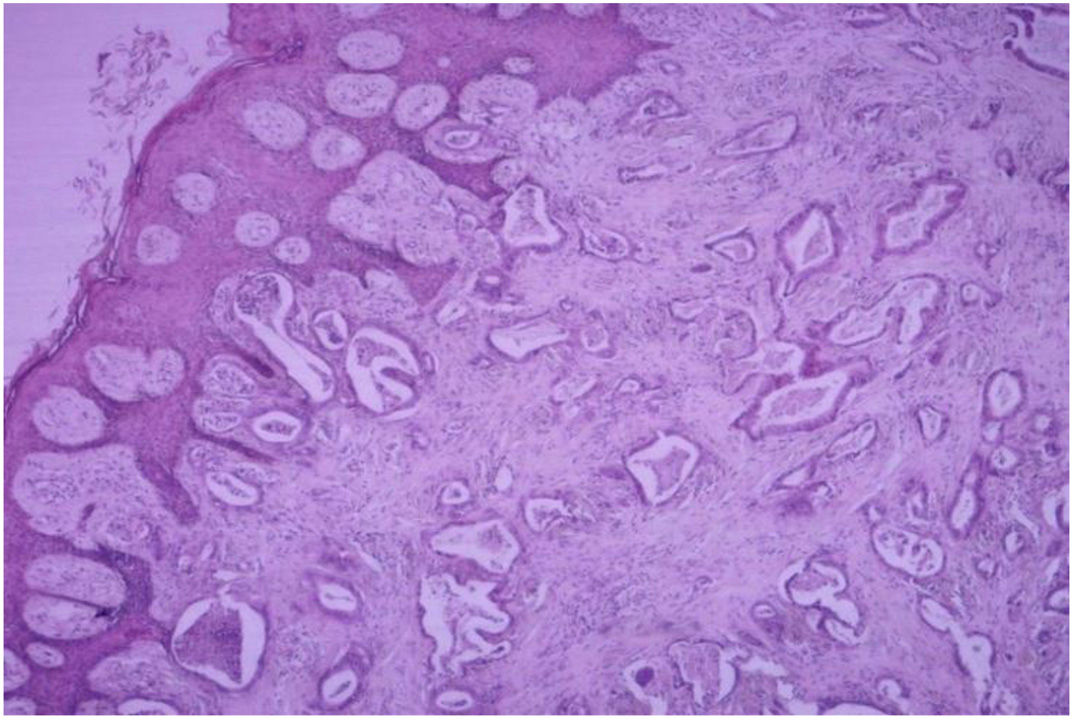
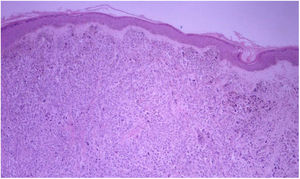
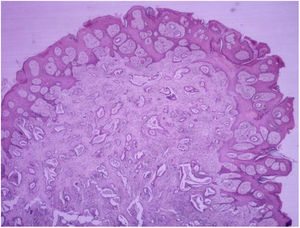
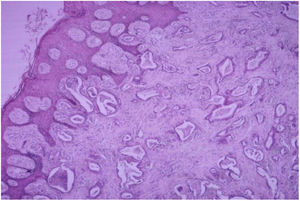
HistopathologyDiffuse infiltration of tumor cells was observed in 69.23% (n=63) of the 91 biopsy specimens analyzed (Figure 8). There were 27 cases of nodular infiltration (29.67%) (Figures 9 and 10) and 1 case of a mixed diffuse and nodular pattern (1.1%). Most of the specimens (60.44%) showed diffuse dermal infiltration of pleomorphic cells.
Vascular invasion was observed in just 21.98% of cases.
All the biopsy specimens showed an inflammatory infiltrate. This was mild in 93.52% of cases (n=76), lymphoplasmacytic in 84.62% (n=77), and mixed (with an associated acute component) in 15.38% (n=14).
Margins were positive in 65.93% of cases (n=60).
DiscussionIn this study, we analyzed data on cutaneous metastases at 2 high-level hospitals to provide preliminary insights into the nature of this condition in our country. The fact that the study was based on a retrospective review of pathology reports will have generated some selection bias, as we only analyzed cutaneous metastases that had been biopsied.
The distribution of cases among men and women (40% vs. 60%) is consistent with reports from the international community.4
Cutaneous metastasis was first described in 1972 by Brownstein et al.,6 who found that the most common primary tumors in men were lung cancer (24%), colorectal carcinoma (19%), melanoma (13%), and squamous cell carcinoma (12%). In women, they were breast cancer (69%), colorectal cancer (9%), melanoma (5%), and ovarian cancer (4%).
The only data available on cutaneous metastasis for Latin America are from a study of 51 cases from Peru, published in 2010.4 The most common primary tumors in this case were non-Hodgkin lymphoma, breast cancer, and renal cell carcinoma. Contrasting with reports from the international literature, we observed a high proportion of unspecified adenocarcinomas, which accounted for the third most common tumor in women and the second most common one in men. Just 3 cases of lung cancer were observed (2 in women), but this low prevalence might be because poorly differentiated adenocarcinomas and carcinomas were not studied by immunohistochemistry in the earlier years of the study.
The regional distribution of skin metastasis is not always predictable, as it can be related to the location of the primary tumor and the mechanism of spread.
Cutaneous metastases from gastrointestinal tumors are preferentially located on the abdomen and this was also the case in our study. Sister Mary Joseph nodule, a metastatic periumbilical nodule resulting from a tumor in the abdomen or pelvis, is an uncommon manifestation of visceral tumors (1%-3%).7 It has been associated with peritoneal carcinomatosis and poor prognosis and has mainly been reported in patients with metastasis from ovarian, gastrointestinal, or prostate cancer.8
In our series, metastases from melanoma were preferentially located on the extremities, supporting reports by Plaza et al.9
Cutaneous metastasis is the first sign of internal malignancy in 0.6% of cases,10 and identifying the primary tumor can be difficult, time-consuming, and costly. In our series, 17 of the cutaneous metastases were diagnosed before the primary tumor and 5 of these were metastases from melanoma.
Cutaneous metastasis can have a wide variety of clinical presentations. In a retrospective study of 164 cases of cutaneous metastasis from breast adenocarcinoma, the most common presentations, observed in 80% of cases, were cutaneous papules and nodules.11 In agreement with reports by El Khoury et al.,12 the most common presentations in our study were multiple nodules followed by solitary nodules. Based on the information from the patients’ medical records, 10 (38.46%) of the metastases from melanoma were pigmented. Pigmentation was not reported for any of the metastases originating from nonmelanoma cancer, although there have been reports of pigmentation in patients with breast cancer.13 Our analysis of clinical features was limited by the availability of medical records and the scant details given on the lesions observed during the physical examination.
Histopathologically, most of the samples showed a dermal infiltrative pattern with little epidermotropism and no ulceration. Noteworthy findings included the scant vascular invasion and the relatively mild nature of the inflammatory infiltrates, which can possibly be explained by tumor evasion of the immune system.
Of the 24 slides corresponding to cutaneous metastases from melanoma, 20.83% (n=5) showed signs of epidermotropism. This rate is high compared with rates reported in the literature (5%-10%).9 The general presentations were quite similar. There were 13 nodular and 11 infiltrative patterns, with scant vascular invasion and superficial ulceration. It should be noted that vascular invasion is not specific to metastasis, as primary melanomas may also exhibit this feature.9
Of the variables contemplated in the survival analysis (sex, primary tumor, and clinical presentation), only primary tumor was associated with a significant difference in survival. Median overall survival was 10 months, but patients with cutaneous metastasis from melanoma lived longer than those with metastasis from breast adenocarcinoma and unspecified adenocarcinoma. The main limitation of our survival analysis is that we did not have information on cause of death or analyze survival in relation to the involvement of other organs. These 2 factors would have enhanced our findings.
ConclusionsCutaneous metastases are rare manifestations of visceral tumors. They are mainly seen in elderly patients and affect men and women similarly. A high index of suspicion is essential as the clinical signs are relatively nonspecific and metastasis to the skin from a primary tumor is a sign of poor prognosis. Early diagnosis is essential considering the advances that have been made in the treatment of late-stage cancer. More specific immunohistochemical techniques are now available that can help to identify the primary tumor, including poorly differentiated carcinoma and adenocarcinoma. It is also important to integrate clinical and pathologic findings to guide the histopathologic study.
The 3 most common primary tumors in our series were cutaneous melanoma, breast adenocarcinoma, and unspecified adenocarcinoma. Contrasting with reports in the international literature and general cancer rates in Chile, cutaneous metastases from lung cancer were not common in the male population analyzed. The use of more sophisticated immunohistochemical techniques could help to identify poorly differentiated cases of adenocarcinoma and carcinoma, including metastases from lung cancer.
This study, which involved a long observation period given the low frequency of cutaneous metastasis in Chile, has provided preliminary insights into the situation in our country.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Kaplan V, Morales C, Bobadilla F, Fernández J, Segovia L, Vera V, et al. Caracterización epidemiológica e histopatológica de metástasis cutáneas en la población consultante de 2 hospitales de Santiago durante los años 2005 a 2017. Actas Dermosifiliogr. 2019;110:220–226.
This study forms part of the thesis by Dr Viera Kaplan within the Training Program for Dermatology and Venerology Specialists at the University of Chile.