Nevus psiloliparus is clinically observed as a well-defined, oval or round, hairless area with a smooth surface located in the parietal or frontoparietal region. Histological examination shows a skin lesion with rudimentary hair follicles and cords of adipose tissue penetrating the dermis. This nevus is the main hallmark of encephalocraniocutaneous lipomatosis (ECCL), otherwise known as Haberland syndrome1-5; however, 2 cases of nevus psiloliparus have been described without neurological or ocular involvement.2 ECCL is a very rare form of neurocutaneous syndrome clinically characterized by lipomatous hamartomas on the face and scalp, ocular abnormalities, and ipsilateral malformations of the central nervous system. We report the case of a neonate with nevus psiloliparus and aplasia cutis congenita (ACC) on the scalp—an association known as a didymosis aplasticopsilolipara—in addition to ocular lesions (lipodermoid cysts and coloboma), a right temporal arachnoid cyst, and aortic coarctation.
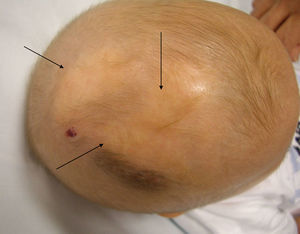
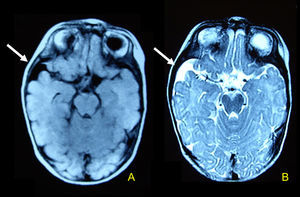
The patient was a 6-day-old neonate, born at term after an uncomplicated pregnancy and normal vaginal delivery; he was the first child of unrelated healthy parents. Physical examination showed a hairless, well-defined, soft, yellowish area adjacent to a bright red, hairless, circumscribed lesion covered by a thin transparent membrane in the right frontoparietal region (Fig. 1). In addition, 2 yellow papules were observed on the right upper eyelid (Fig. 2); these were diagnosed by the ophthalmologist as lipodermoid cysts associated with an ipsilateral coloboma. Neurological examination was normal. Histopathologic examination of the hairless area of the scalp showed abundant fatty tissue, rudimentary hair follicles, and isolated arrector pili muscles; the findings were compatible with nevus psiloliparus. Brain magnetic resonance imaging (MRI) showed an arachnoid cyst occupying the right temporal fossa (Fig. 3) and echocardiography revealed moderate aortic coarctation.
The clinical, histological, and brain MRI findings led to a diagnosis of ECCL.
ECCL is a neurocutaneous syndrome of unknown etiology. Described in 1970 by Haberland and Perou,6 it is characterized by unilateral lesions in tissues of ectodermal and mesodermal origin: skin, eye, adipose tissue, and brain. Aortic coarctation, progressive bone cysts, and jaw tumors have also been described in association with this syndrome.7 The differential diagnosis with other neurocutaneous mosaicisms, such as Delleman, Goltz, Goldenhar, or Proteus syndromes, can be very difficult due to the large number of overlapping features.
Nevus psiloliparus in close association with ACC was first described in 2 patients by Torrelo et al.1 in 2005; a third case was reported by Stieler et al.2 in 2008. This association, known as didymosis aplasticopsilolipara, has been described as an example of nonallelic twin spotting.1,2,8
Our case is the fourth report of ACC and nevus psiloliparus in association with ECCL. The fact that this association has been described in isolated cases only suggests that it is purely coincidental; however, we consider that if new cases of ECCL with this characteristic clinical presentation are reported, we may need to consider the possibility that ACC and nevus psiloliparus form part of the clinical spectrum of this neurocutaneous syndrome.
Please cite this article as: Martí N, Alonso V, Jordá E. Lipomatosis encefalocraneocutánea y didimosis aplasticopsilolípara. Actas Dermosifiliogr.2012;103:341-342.