A 12-year-old boy with a family history of melanoma consulted for changes in a pigmented lesion on the back first observed 2 months earlier. The patient's family reported that the lesion had existed for years and that it had increased in size and acquired a purple hue following a trauma. The only symptom reported by the patient was discomfort caused by rubbing.
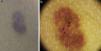
Physical ExaminationPhysical examination revealed a pigmented macule in the left scapular region; its purplish red coloration gave the lesion a bruise-like appearance and ecchymotic spots were visible in the central area (Fig. 1A) The most characteristic dermoscopic findings were areas characterized by a lightish brown fine reticular pattern around the periphery and a pseudo-lacunar background pattern dotted with thrombosed vessels in the central area (Fig. 1B).
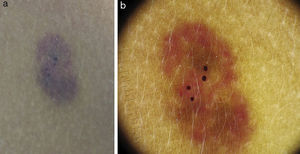
HistopathologyHistologic examination of a sample obtained by punch biopsy revealed irregular dilated vessels in the superficial dermis and protuberant endothelial cells in the vascular lining with characteristic hobnail morphology. Slight epidermal hyperplasia and hyperpigmentation of the basal layer were also observed (Fig. 2A).
Immunohistochemistry completed the histologic study, and the endothelial cells lining the vessels in the lesion tested positive for D2-40, an antibody that identifies podoplanin and is specific to the lymphatic endothelium (Fig. 2B).
What Is Your Diagnosis?
DiagnosisTargetoid hemosiderotic hemangioma (hobnail hemangioma).
Clinical Course and TreatmentWhen informed of the histologic findings and the benign nature of the lesion, the family decided to adopt an attitude of watchful waiting.
CommentTargetoid hemosiderotic hemangioma (THH) is a vascular lesion usually found on the trunk or extremities in young adults. The typical clinical presentation is a single violaceous papule surrounded by a brownish erythematous halo, which may increase or decrease in size or even disappear periodically leaving only the central papule.1 When complemented by a careful and comprehensive medical history, dermoscopy is a useful noninvasive tool in the diagnosis of these lesions. It has been suggested that THH may appear as a result of trauma to a preexisting hemangioma.2 In the case described here the patient reported prior trauma and dermoscopic examination revealed a non-palpable lesion with a reticular pigmented pattern on an erythematous macule characterized by a pseudo-lacunar appearance and the presence of ecchymotic dots suggestive of thrombosed vessels in the central area.
Only 7 cases of THH with dermoscopic findings have been reported.1–5 Most of the patients were young adults and the lesions were described as being targetoid with a palpable central lacunar pattern surrounded by an erythematous-violaceous halo. A fine pigmented reticular pattern around the periphery has only been described in 2 cases.1,3 This histologic feature has been correlated with hemosiderin deposition in the mid dermis1 and also with lentiginous epidermal hyperplasia and elongation of the rete ridges.3 The second of these hypotheses would appear to be the most accurate since the presence of hemosiderin deposits in the dermis would give rise to blue-gray areas and/or dots on dermoscopy.
No consensus has yet been reached on the etiology of the condition; Franke et al.6 proposed a lymphatic origin based on positive staining for D2-40 antibodies, as was the case in our patient.
The differential diagnosis should be posed primarily with other vascular lesions, such as the plaque forms of Kaposi sarcoma (especially lymphangioma-type) or acquired progressive lymphangioma, melanocytic lesions, such as melanocytic nevi, and other benign tumors, including dermatofibroma and inflammatory lesions such as insect bites.3
As it is a benign lesion that has no clinical repercussions THH does not require treatment. Dermoscopy and clinical history are usually the most useful tools for making a correct diagnosis, but in doubtful cases or when there are aesthetic reasons for removing the lesion, excision is the definitive treatment. No recurrence has ever been reported.
Please cite this article as: Padilla-España L, Hernández-Ibáñez C, Fúnez-Liébana R. Mácula equimótica sobre lesión pigmentada tras traumatismo. Actas Dermosifiliogr. 2014;105:707–708.