Dissecting cellulitis of the scalp (DCS) is a follicular occlusion disorder that may progressively lead to scarring alopecia. It presents as multifocal painful nodules and boggy plaques with alopecia which is reversible in early disease, but can become scarring in longstanding lesions.1 Dermoscopy is an useful non-invasive method for diagnosis and management of hair and scalp disorders, including cicatricial alopecia, such as lichen planopilaris, lupus erythematosus, and folliculitis decalvans.2–5
We first report here the dermoscopy features in 6 patients with DCS. The patients included 5 males and 1 female aged 26–46 years. These included 1 Caucasian male and 5 African Americans. All patients presented with multiple patches of alopecia overlying painful scalp nodules (Fig. 1). Duration of the disease ranged from 3 months to 3 years.
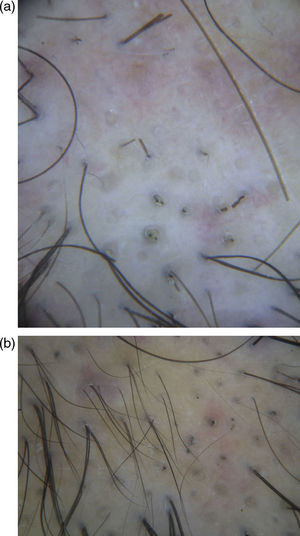
Dermoscopy of the alopecic patches showed yellow dots, red dots, empty follicular openings, black dots and cadaverized hairs (Fig. 2a). Exclamation mark hairs were absent.
(a) Dermoscopy showing yellow dots, empty follicular openings, black dots and cadaverized hairs, very similar to AA. Exclamation mark hairs were absent (dermoscopy, at 40× magnification). (b) Dermoscopy of follow-up, showing short regrowing hairs and dystrophic hairs (dermoscopy, at 70× magnification).
All patients used oral and topical antibiotics. Follow-up revealed partial hair regrowth in all cases. Dermoscopy was also useful in the short-term follow-up, showing short regrowing hairs and variable dystrophic hairs (Fig. 2b).
The dermoscopic patterns observed were very similar to those observed in non-scarring alopecias, simulating active lesions of alopecia areata (AA) in some cases, especially when the nodules were small.
Dermoscopy of AA have been widely described, and active lesions present black dots, tapering and broken hairs and short vellus hairs.6
We consider that early DCS might be included in the differential diagnosis of patch alopecia with the dermoscopic pattern similar to AA.
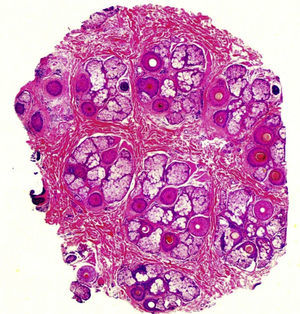
Histopathology showed in all cases preserved number of follicular units at the isthmus level and preserved follicular density (Fig. 3). There was an increased number of follicles in catagen/telogen phase and decreased number in anagen. On the average 33% were in telogen versus 67% in anagen which is a sign of shortened hair cycle and premature conversion to catagen. Pigment casts were observed in a few follicles as a result from abrupt transition of anagen into catagen. At the infundibular level some follicles showed dilated empty infundibular ostia filled with sebum and keratin, which corresponds to the yellow dots on dermoscopy. A prominent feature was the presence of dense inflammatory infiltrate at the level of the isthmus around the follicles and interstitial in the interfollicular deep reticular dermis. The infiltrate was composed of neutrophils, lymphocytes, histiocytes and many plasma cells as well as red blood cell extravasation. Another feature was the increased number of fibrovascular streamers (stelae) showing inflammatory cells (lymphoctyes and plasma cells) and dilated vessels.
Early DCS shows dermoscopic features of non-scarring alopecia with signs of anagen hair loss. We believe that the acute dermal inflammation cause acute anagen interruption in follicles with high mitotic activity (late anagen phases). Follicles in early anagen will enter prematurely into telogen. This explains dermoscopic and pathologic features observed in early lesions of DCS. Successful treatment of the disease at this stage is associated with complete hair regrowth.