Dermatitis artefacta is a rarely diagnosed disorder that is often a source of perplexity and anxiety for dermatologists because they know less about the cause of this self-inflicted condition than the patients themselves. It differs from other skin disorders in that diagnosis is made by exclusion rather than on the basis of histologic and biochemical findings and therefore involves a considerable investment of time and resources. Based on the findings of a study of 201 patients diagnosed with dermatitis artefacta between 1976 and 2006, we review the different clinical presentations of this skin disorder and discuss its diagnosis and treatment. The series analyzed comprised 152 women and 49 men (female to male ratio of 3.1:1) with a mean age of 31.2 years. The patients were mostly single and had a low educational level and few or no job qualifications or skills.
La dermatitis artefacta (DA) es un diagnóstico excepcional, que genera perplejidad y ansiedad al dermatólogo al encontrase ante una patología autoprovocada y de la que el paciente sabe más que el médico en cuanto a su etiología. Al contrario que otras dermatosis en la que existen pruebas histológicas o bioquímicas, en la DA el diagnóstico es de exclusión lo que exige un gran consumo de recursos y de tiempo. En el presente trabajo repasamos las diversas formas clínicas, criterios diagnósticos y manejo de estos pacientes y para ello nos basamos en la experiencia del estudio que realizamos de 201 casos de DA diagnosticados entre 1976 y 2006, de los cuales 152 eran mujeres y 49 varones, con una proporción de mujeres/varones de 3.1/1. La edad media fue de 31.2 años y estaba mayoritariamente constituida por personas con escasa o nula cualificación laboral, bajo nivel cultural y mayoritariamente solteros.
The nosological position of dermatitis artefacta (DA) is clear in the numerous classification schemes of skin conditions linked to mental disorders,1–6 in which it is invariably classified as a manifestation of a primary psychiatric disorder. While the Vienna Diagnoses Schedule for Psychodermatological Disorders is probably the most complete and comprehensive classification published to date,7 it is of little practical use for dermatologists who do not work in the field of psychodermatology. It may therefore be preferable to use Gupta's4 classification of psychodermatoses (Table 1), which is more didactic as it is based on the current concepts of psychiatric disease defined by the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV).8
Associations of Skin Disease with Psychiatric Disorders.
| 1. Primary psychiatric symptom that manifests as a dermatological condition |
| a) Delirium |
| b) Hallucinations |
| c) Body dysmorphic disorder |
| 2. Disorders associated with self-inflicted dermatoses |
| a) Dermatitis artefacta |
| b) Neurotic excoriations |
| c) Excoriated acne |
| d) Trichotillomania |
| 3. Miscellaneous syndromes |
| a) Burning mouth syndrome |
| b) Psychogenic pruritus |
| c) Psychogenic purpura syndrome |
Source: Gupta et al.4
The term dermatitis artefacta is only used to refer to the condition in which skin lesions appear in a secret and mysterious way while the patient denies all responsibility for their production. In DA, the patient produces skin lesions to satisfy a psychological need, often a desire to receive medical treatment.9 Malingerers also deny responsibility for producing the signs and symptoms of their disease, but they do so for easy-to-discover reasons, such as financial gain or a lawsuit. Munchausen syndrome sometimes includes skin involvement,9 generally DA, but in that setting the skin involvement is just 1 element in a broad spectrum of conditions affecting other organs10 and will be associated with repeated hospital admissions, which the patient tries to conceal while demanding medication and exploratory tests. Unlike DA, Munchausen syndrome is more common in men than in women. It is not unusual for DA to occur following treatment for another condition that brought the patient into contact with the hospital environment.9
DefinitionDA is defined as any condition involving self-inflicted skin lesions for which the patient denies all responsibility.11,12 However, some authors consider that the nosological definition of DA should specifically exclude cases in which a rational motive exists for the self-infliction of lesions, thereby excluding malingerers.13 Another essential characteristic of DA is that the patients conceal their role in producing the signs of their condition; this concealment is what differentiates DA from other self-inflicted dermatoses, such as self-mutilations by psychotic patients, neurotic excoriation, and trichotillomania.
EpidemiologySince DA is rare in routine dermatological practice, the literature contains few case series. Most authors have described isolated clinical cases of particular interest to specialists either because of the diagnostic challenges involved or the severity of the clinical presentation. However, it is believed that up to 5% of medical visits may relate to factitious disease, and such cases are not only observed in dermatology but also encountered by internal medicine, ophthalmology, endocrinology, and ear nose and throat specialists.12,14 Owing to the ease with which it can be damaged, the integrumentary system is the organ that is most often the object of self-inflicted lesions. This was shown by a study of 31 patients who presented with factitious conditions in a general hospital14; in that study there were 13 cases of DA, 12 cases of simulated fever, 3 of self-inflicted bleeding, 1 of polyuria-polydipsia syndrome, 1 of hypoglycemia, and 1 of hyperthyroidism.
Few series provide data that can be used to compare the relative incidence of DA and other psychodermatologic disorders. In a 3-year study carried out in Iran, 178 patients were diagnosed with various psychodermatologic disorders15: 128 neurotic excoriations (71.9%), 22 trichotillomania (12.4%), 16 delusional parasitosis (9%), and 12 DA (6.7%). Women outnumbered men in all of these diagnoses except delusional parasitosis, which was more frequent among men. DA was the least common diagnosis. In a study of 35 patients with dermatological disorders of strictly psychological origin, 8 patients had DA, 8 had delusional parasitosis, and 19 had various dysmorphic disorders.16
One of the first case series of DA was published by Azúa in 1909.17 After studying the cases of 4 women who had been diagnosed with “hysterical gangrene”, he confirmed the hysterical origin in 1 case but redefined the other 3 as self-inflicted lesions. One review of 59 articles on DA included 130 patients (116 women and 14 men).18 A retrospective study in Denmark covering 20 years included 57 patients with a diagnosis of DA.19 That group consisted largely of women (74%), with a female-to-male ratio of 2.8:1; the median age was 39 years (range, 12-86). A review of the records of a French dermatology department over a 15-year period identified 31 patients with a diagnosis of DA20; 23 of the patients were women (mean age, 32.4 years) and 8 were men (mean age, 23.7 years). Our series of patients diagnosed between 1976 and 2006 included 201 patients, with a clear preponderance of women (female-to-male ratio, 3.1:1) and mean age overall of 31.2 years.1,21 Other interesting characteristics observed in our series were the low or nonexistent skill level, low income, and low cultural level of the patients and the higher proportion of single people.
In children, DA is more common among girls than boys, as shown by a Mexican series of pediatric patients covering a period of 20 years, which included 25 girls and only 4 boys.22 Similarly, an Australian study covering a 15-year period included 24 girls and only 8 boys.23
DA can appear at any age, but the incidence is highest around 20 years of age. In many cases onset is preceded by a period of psychosocial stress, which is generally easily identified, such as the psychological disturbance that produced acne symptoms in an adolescent who injured his skin with a blister agent.24 It is not unusual to find a connection with the hospital setting in these patients, who may be nursing aides, nurses, relatives of physicians, or individuals who have had prolonged diseases in childhood3 or who have been affected by the death of a family member.9
In summary, we can say that DA is more common among females and1,2 in early adulthood and that a high proportion of those affected have a low social and cultural level.
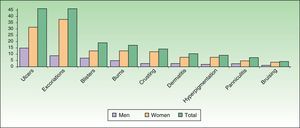
Clinical FeaturesDA presents in a great variety of clinical forms (Fig. 1) depending on the patient's creativity and the method used to produce the lesion.12,25 The most common presentations are as follows:
- 1.
Excoriations. Excoriations are the most easily diagnosed factitious lesions. They are usually linear (Fig. 2) and are most often inflicted using the fingernails (Fig. 3) although a variety of sharp objects may also be used (Fig. 4). Distinguishing between DA and neurotic excoriations can sometimes be difficult, but patients who have the latter condition recognize that they have caused the lesions. Excoriations are highly susceptible to infection and an indicative finding is the absence of itching before the onset of the lesion.26
Excoriations are a common clinical form of DA because the lesions are easy to inflict; in our case series they were observed in 52 (25.8%) of 201 patients and were more common in women (28.4%) than in men (17.7%).
- 2.
Ulcers. Ulcers are the most common lesions in most series. They are found either in the early stages of development or after resolution, when they take the form of an eschar (Fig. 5). The morphology of these ulcers tends to be odd,12 either because they have perfectly regular borders or because they have an irregular shape that includes linear segments (Fig. 6), acute and obtuse angles, triangular forms, star shapes etc. Linear lesions that extend outwards from a primary lesion are also observed (the drip sign). Sometimes, clearly ulcerated lesions appear together with other lesions that are either incompletely executed or caused by splashes of the caustic agent used to produce the ulcers. Scars from past or old injuries may also be observed. Old ulcerations that have been subjected to repeated irritation or modified by multiple treatments exhibit characteristics of torpidity (sclerosis, atrophy), and underlying osteitis or necrosis caused by secondary infections is sometimes present.26 Patients may also have scars with an irregular geometric shape.
Litmus paper can be used to test the alkalinity or acidity of unexplained ulcers as the results may indicate the use of a chemical product as a probable cause.12,27 Repeated failure of skin grafts, usually due to vascular problems, should raise the suspicion of interference by the patient, especially when the only organism found in cultures is fecal flora (a finding observed in 4 of our cases).
In our series, a clinical presentation described as an ulcer was observed in 52 patients (25.8%), making it, together with the category of excoriations, the leading manifestation. Ulcers were more common among males (31.1%) than females (23.8%). In a study of patients with DA affecting the breast, excoriations and ulcers were found to be equally common (33.33%).19
- 3.
Blisters. Self-inflicted lesions sometimes take the form of blisters. The appearance of these lesions may be odd; they may be elongated (Fig. 7), angular, polygonal, or occasionally very large, sometimes with several lobules. In most cases, blisters are found together with other lesions, such as ulcerations, scabs, and erythema in more or less geometric shapes.
The lesions may be irregularly shaped and have an unusual distribution, for example perfectly irregular.12,27 The course is always benign, but the size, number, and gangrenous nature of the blisters can sometimes produce veritable mutilations. Self-inflicted blisters are caused by burns or cauterization and are produced through the application of chemical or medical products.
Blisters can also be produced through friction on sites where the epidermis is thick and firmly attached to the underlying tissues. The histologic findings in such cases are characteristic and can distinguish these lesions from the blisters found in bullous disorders.28
In one report a rubber nipple was used to produce suction blisters mimicking pemphigoid.29 In another case of DA, an aerosol spray deodorant was used by a 12-year-old girl to induce blistering.29 The same method was used by 3 patients (a 12-year-old boy and 2 women aged 21 and 36 years), who induced bullous lesions on the extensor surfaces of the limbs by producing cold burns using a spray deodorant.30 This was probably also the method used in the case of a 13-year-old girl described in another case report.24
In our series, 21 (10.3%) of the 201 patients presented with a variety of bullous symptoms, a presentation more common among men (13.3%) than women (9.2%).
- 4.
Panniculitis. Ackerman et al.31 reported the case of an adolescent with fever, nodular syndrome, and nonsuppurating panniculitis—a presentation clinically and histologically consistent with Weber-Christian disease. By chance it was discovered that the manifestations were caused by self-injections of milk that produced erythematous nodules around the injection site accompanied by chills, fever, sweating, and general malaise. Steinman and colleagues32 described a similar case in a nurse whose symptoms were also produced by self-inoculation with milk on the dorsum of the left hand. In a study of 5 women with factitious panniculitis,33 the signs of disease were found to be produced by repeated trauma. The diagnosis was only confirmed after histologic examination revealed inflammatory features and bruising and after the lesions had been cured by means of occlusive dressings.
It is important to note that some patients develop indurated lesions on the breast, which sometimes ulcerate, and when they are referred for surgical treatment they may undergo a mastectomy without any prior biopsy having been performed.12 A recent Spanish study summarized the etiologic, pathogenic, clinical, and histologic features and treatment of panniculitis produced by trauma or the injection of drugs or chemicals.34
In our series, 7 patients (3.4%) were diagnosed with factitious panniculitis (Figs. 8 and 9). In 1 case, the symptoms were caused by subcutaneous injection of urine.
- 5.
Localized crusting. Carteaud35 described a case of factitious cheilitis, which he called le tic des levres. Some years later, Savage36 reported a similar condition, which he called localized crusting; he described cases of keratotic or bleeding scabs on the lips that had no apparent cause in which he suspected deliberate or unconscious manipulation by the patient. Several terms have been used to describe this clinical picture, including factitious lip crusting,37factitious cheilitis,38–40 and exfoliative cheilitis artefacta.41–43 It has been speculated that the mechanism of production might be repeated manipulation of the lips with the teeth, tongue, or even instruments.44 In some cases, the nasal pyramid is affected.
Our series included 6 patients (5 women and 1 man) with localized crusting; in one of the women, the crust was located on a finger. One of the woman (Fig. 10) had concomitant anorexia nervosa.45,46
- 6.
Eczematous lesions. Some patients produce eczematous lesions by applying irritants to the skin47 or exposing themselves repeatedly to an allergen in the case of patients with allergic contact dermatitis. It is sometimes difficult to prove the cause of such lesions.48
- 7.
Edemas. In 1911, Secretan49 described swollen limbs as a possible presentation of self-inflicted disease. Angelini et al.50 later called this form of self-harm Secretan syndrome. Smith51 defined a set of criteria that should raise a suspicion that the lymphedema is factitious: recurrent unilateral lymphedema without any apparent lymphatic or venous obstruction and any lymphedema that is clearly delimited by a ring of a different coloration. Several types of edema caused by ligatures are reported in the literature, including edema of the nipple,52 the tongue,53 the neck,54 and even of the scrotum leading to self-castration.55
- 8.
Purpuras and bruises. Gardner and Diamond56 first described the autoerythrocyte sensitization syndrome, which is characterized by painful ecchymoses in sites within reach of the hands, typically in women with psychological disorders (Fig. 11). The patients’ hypersensitivity to injections of their own blood has been used as a diagnostic criterion. Some authors have tried to differentiate between purpura factitia and autoerythrocyte hypersensitivity syndrome.57 In their view, the latter condition is characterized by the presence of prior pain and possibly bleeding in internal organs, while the appearance of lesions in purpura factitia is not preceded by pain and the results of challenge tests with the patient's own blood are negative if the site is protected with a bandage. However, the criteria for differentiating between purpura factitia and autoerythrocyte hypersensitivity syndrome are unclear. Despite these nosological difficulties, the authors of a recent review of the literature including 162 cases propose treatment with psychotropic drugs and psychotherapy.58 While differentiating these 2 disorders is difficult,59 the case of a patient with DA and painful bruising syndrome may be of some help.60
In our series, 3 women (aged 26, 27, and 36 years) had this condition.
The spectrum of clinical presentations of DA could be even broader than that described here as the manifestations depend on the patient's imagination.
DiagnosisA diagnosis of DA is difficult to establish because of the great variety of possible dermatologic conditions. The situation is further complicated by the diversity of methods used by patients to self-harm and the ingenuity they employ in doing so (Fig. 12).61
Three aspects can be used to establish a diagnosis of self-inflicted skin lesions: a) the morphology of the lesion; b) the patient's personality; and c) the medical history. However, it is not advisable to establish a diagnosis based on just one of these criteria.12,13 DA is the somatic expression of extremely serious and deeply buried mental suffering, of which the patient is unaware.13 In DA, the normal roles of patient, physician, and disease are subverted. This subversion takes the form of a twofold challenge, psychological on the one hand and a challenge to the standards underpinning medical practice on the other.
The diagnosis should not be reached merely by a process of elimination, but should rather be established from among the possible alternatives. The diagnosis of DA is made on the basis of a combination of positive dermatological and psychological findings and requires the collaboration of the medical team and their acceptance that DA is the expression of significant mental suffering, of which the patient is unaware.
Although very old, the Stokes and Gardner classification is still a useful tool for establishing a diagnosis of self-inflicted lesions. In the following sections we will outline the different aspects that form the basis of that classification.62
Shape and Configuration of LesionsThe diagnosis should be determined by the shape of the lesions and by ruling out other skin disorders with clearly defined characteristics. Although the lesions may be caused by chemical or thermal burns, they can also be the result of trauma. Cutaneous artifacts caused by an instrument tend to be regular and geometric in shape (Fig. 13), an uncommon morphology in the case of spontaneous eruptions. Chemical burns are regular in shape, although at times their borders may be interrupted by fingerlike projections caused by the linear spread of drips of the caustic liquid used to produce the lesion.
Lesions sometimes have a bizarre or fantastic appearance63 (Figs. 14 and 15), appearing suddenly at irregular intervals, generally singly or in pairs. The course may be unusually rapid. When the caustic substance is applied using a needle or tweezers, a method frequently used in gangrenous areas, the edges of the lesion have a saw-tooth or serrated appearance, caused by the repeated pricks made along the leading edge. When escharotic lesions are observed, they tend to be superficial and the scabbed area is separated from the normal skin by an intensely erythematous border.
It is sometimes possible to determine that the nails, fingers or a sharp object in the patient's possession are impregnated with the causal agent.
In summary, to the eyes of an expert, these lesions will appear odd from the very beginning and are easily recognized as unexpected and dubious. The initial impression of self-harm is strong (Fig. 16) and this is of great importance for the diagnosis; however, a diagnosis of self-harm should not be reached without careful critical analysis. Closer examination of the manifestations may provide the physician with evidence that will confirm the diagnosis of a self-inflicted lesion. DA is always destructive (ulcers, enucleations, gangrene)12 although such a clinical picture alone is not enough to establish a diagnosis of DA.25
Our series yielded a number of findings not yet reported in the literature: we were able to establish that the creation of lesions in multiple sites was more common among women, while solitary lesions were mainly observed in men.
Distribution of the LesionsThe lesions are generally located in areas accessible to the hands and tend to be more numerous in sites accessible to the right hand in right-handed patients and vice versa. When choosing sites for lesions patients typically avoid the palms, soles, nose, mouth, scalp, genitals, and the outer ear.63 The presence of lesions in an area inaccessible to the hands does not necessarily rule out a diagnosis of DA, since such sites can be reached by other means. Lesions are sometimes distributed regularly around a central point, such as a nipple or the navel, and they are often located close to a previous lesion, in an attempt to extend the original damage.26
The sites found in our series were as follows: the face (34.5%), the lower limbs (25%), the upper limbs (16.6%), and the hands (15.5%). The most common site in men was the legs (51%) and in women the face (40%).
If, as Fabisch64 has suggested, the anatomical site of the lesion has a psychological significance that should be taken into account by the psychotherapist, it is interesting to highlight the large number of women in our case series with lesions affecting the breasts (Fig. 17), in some cases involving very destructive clinical forms.
The Patient's DemeanorGreat importance is placed on the appearance and demeanor of the patient with DA. Typical descriptions include anxiousness, fine tremor of the facial muscles, tearful eyes, or on the contrary, a poker face or Mona Lisa expression.27 Some patients exhibit the calm of a tense person or a gaze with erotic connotations (bedroom eyes). Another remarkable characteristic seen in some patients is an attitude of great mental calm and complacency about their condition (what the French call la belle indifference).
Young patients are sometimes accompanied by domineering parents or solicitous parents will accompany a difficult and precocious child. The patient's interest in their lesions, a tendency to display them and to express anger are all signs that should raise a suspicion of self-harm.
The patient's expression can range from guilty, furtive, or unfriendly to one of obvious pretense. Some patients may be reserved and uncommunicative or display signs of low intelligence, although in Lyell's12 view a high level of intelligence is also compatible with a diagnosis of DA, while a mature personality is not. Obviously none of these criteria is absolute.
TimingRecurrence following periods of stress, sleepwalking episodes, the patient's failure to return after several visits, the appearance of lesions on certain dates, and lesions that appear overnight are all signs of self-harm. Another circumstance that may suggest DA is when the recurrence of lesions coincides with a new job, moving house, a new school, the death of a family member, or any other event likely to cause mental stress, depending on the age and circumstances of the patient. In such cases, the lesion can be interpreted as an attempt at nonverbal communication.64
The patients’ inability to talk about the origin of their lesions or their lack of interest in the subject prevents the dermatologist from gaining a clear idea of the situation. The patient's account of the lesions is sometimes so lacking in substance that Gandy25 coined the term hollow history. This perplexity about what is happening is expressed by the patient in bitter and hostile terms, and new lesions will continue to appear as long as the conditions are favorable, that is, as long as the patient enjoys privacy and a supply of the necessary materials.
Another term used in DA is melodramatic prophecy, referring to predictions by patients concerning when and where new lesions will appear.12 Many patients with DA play games with their physicians informing them 12 or 24hours before the lesions appear what sites will be affected, explaining that the lesion will be preceded by heat, burning, or some other abnormal sensation.63 In other cases lesions appear in a place where the dermatologist has suggested they might occur.61
Assessment of Neurological Signs and SymptomsSubjective sensations, such as pain and burning, may be exaggerated by patients with DA. The patient's psychiatric history should be investigated to establish whether he or she has had any previous psychiatric diagnosis or has a family history of mental illness.
Study of MotivesIn the case of patients with a hysterical personality, the motive for self-harm is to deceive, but the underlying cause is solely the desire to be a sick person in order to escape personal obligations and inner conflicts65,66 even though there may be no apparent justification for the patient's conduct.67 The possible motives for DA will be as varied as are human personalities and the situations of life itself.25 The motive can sometimes be a simple desire to arouse the sympathy of relatives or friends or an attempt to rationalize feelings of frustration or failure in life; in other cases the behavior may be a result of conflict in the patient's social environment, financial problems, a lack of self-esteem, atonement for guilt, revenge, or a way to escape responsibilities.68 Patients who create skin artifacts are also trying, often unconsciously, to attract the attention of those around them to an inner conflict for which they have no solution.
Malingerers and fraudsters do not easily fool doctors10,69 because the patient who merely contrives disease is an impostor; in such cases the external incentive for the behavior must be found to confirm the diagnosis.25 Such individuals typically use lesions to achieve a secondary goal: to excuse failure, attract sympathy, escape responsibilities, or simply to delay making a payment that is due.70 They may have criminal motives, such as fraud or avoidance of a legal obligation,67 or even use the situation to obtain privileges, money, or narcotics.10
HistologyA fairly common characteristic in the histology of DA is that superficial involvement predominates over deeper involvement.61 Typically, abnormal findings are restricted to the epidermis and no accumulation of lymphocytes or signs of vasculitis are found. However, the findings are not diagnostic and in most cases will depend on the method used to create the lesion. A wide range of histologic findings have been reported, including71 erosion, acanthotic epidermis, chronic perivascular infiltrate, and foreign-body reaction with birefringent material.33,34
Whenever possible a biopsy should be obtained because histologic findings have in many cases been fundamental to the diagnosis, particularly when other skin conditions have been confused with DA. Perhaps the dermatological diagnosis most often confused with DA is pyoderma gangrenosum. DA has also been confused with pyoderma and vice versa.72–74 Conditions misdiagnosed as DA on the basis of clinical findings have been shown by histologic findings to be genuine panniculitis-like T-cell lymphoma.75 By contrast, a case of DA on a girl's face mimicked a lymphoma,76 while in other cases erosive lichen planus,77 cryoglobulinemia,78 and acquired hemophilia79 were misdiagnosed as DA. In other cases DA presented clinically as vasculitis80 and trigeminal trophic syndrome was misdiagnosed as DA due to the absence of abnormal histologic findings.81
It is sometimes essential to use more complex histologic techniques, such as X-ray analysis and spectrophotometry. In one case, spectrophotometry demonstrated that the cause of recurrent abscesses was cellulose.82 In an earlier case, electron probe microanalysis was used to determine the presence and nature of factitious granulomas.83 Friction blisters at the level of the distal stratum granulosum have been reported.84 The presence of birefringent material and pseudocystic spaces replacing fat are important indications that will help to establish the diagnosis of factitious panniculitis.
There is no doubt that DA lesions can mimic other skin processes. McCormac67 makes the point that, while it is clear that a patient cannot produce lesions that simulate psoriasis or lichen planus, they can create lesions with a very obvious inflammatory substrate.
Differential DiagnosisThe dermatological condition most likely to cause problems in the differential diagnosis of DA is neurotic excoriation.85 While the lesions in this condition are also self-inflicted, the patients do not try to deceive the physician; they are victims of an irresistible urge to pick, scratch, or otherwise manipulate the skin, nails, or hair.16 Another important difference between neurotic excoriation and DA is that patients with the former only use their nails while patients with DA may use a range of methods to damage the skin.
DA must be differentiated from the skin lesions produced by psychotic patients, who may use their fingernails to excoriate the skin and cause ulcers that may become infected. In such cases, there is no doubt about the origin of the lesions because the patient causes them in view of other people.
PsychopathologyExperts concur that DA is a cutaneous manifestation of a psychiatric disorder and the condition is classified in the DSM-IV (Table 2).8
DSM-IV Criteria for Factitious Disorder with Predominantly Physical Signs and Symptoms (300.19).
| A. Intentional production or feigning of physical (but not psychological symptoms) signs or symptoms |
| B. A psychological need to assume the role of a sick person, evidenced by the absence of any external incentive for the behavior, such as economic gain, obtaining better care, or improving physical well-being |
| C. The disturbance does not occur exclusively during the course of an axis 1 disorder, such as schizophrenia. |
Source: DSM-IV: Diagnostic and Statistical Manual of Mental Disorders.8
One of the chief concerns of physicians who study DA is to identify a motive that would justify the behavior of patients who self-harm, although some clinicians and dermatologists have minimized the role of the mind in the development and perpetuation of certain types of skin disease by applying the frivolous designation “nervous” and have failed to ensure that the patient receive appropriate psychiatric treatment.86 Fortunately, the work of English,87 Cormia,88 and Zaidens89 has led to a better understanding of psychosomatic conditions and improved treatment.
There is no consensus about the personality type involved in DA. Some authors consider that there are 2 types of patients, some hysterical and others who are simply malingerers.17,25,67,70,90 Others classify patients with DA as hysterical or psychotic.68,86 Michelson66 and Susskind90 believe that all DA patients are hysterical, while Koblenzer91 considers them all to be borderline psychotic. Factitious disease appears to be a kind of emotional safety valve in emotionally immature patients who typically present hysterical and masochistic characteristics.10 Lesions may be produced when patients are in an altered psychogenic, borderline,92 or dissociative state, so that they are not conscious of their actions.6 The psychological importance of DA is that while the patients consciously produce the lesions, they are unaware of the reasons for their self-destructive behavior. Patients may exaggerate pain, adopting the role of martyr, and this posture is confirmed by their great capacity to take pleasure in tolerating pain.86
Although they cannot be considered to have psychotic personalities, many patients with DA do have a borderline personality structure and are unable to develop mature relationships. They use their lesions to maintain contact with others and to get the attention they desperately need to fill their emotional vacuum. Another motive for self-harm may be a desire to do penance for unconscious sins or their behavior may be a displaced expression of infantile rage.91
Musaph93 considers that patients with DA produce their symptoms unconsciously, and psychiatric-psychological studies have revealed that the condition is in part due to aggressive sexual feelings directed against key figures in the patient's childhood.
Zaidens92 is the author who has perhaps contributed the most psychological and psychiatric studies on DA. She believes that self-inflicted dermatitis represents frustration, resentment, a demand for attention, anxiety, hostility, and helplessness. The self-destruction is proportional to the severity of the underlying emotional disturbance.
Auto-destructive mechanisms develop in dependent and timid individuals who are unable to express themselves. These patients have been conceived and reared in an environment fettered by emotional barriers, and their growth has not been very important to their parents, particularly their mothers. Most patients with DA are adults in middle-age who have not achieved their life goals or have not achieved the levels of success typical of their class models, in either social or economic terms.94 In psychological terms, they use DA to get sympathy, attention, pity, or compensation. Moreover, since patients with DA are unable to deal with their problems, or to even admit that they have a problem, the lesions provide them with an excuse they can use to rationalize their frustrations.
DA sometimes appears in the context of a folie à deux or shared dementia. Shared dementia is a psychotic disorder characterized by the development of a hallucinatory pattern shared by 2 people. Since those affected have a long-lasting intimate relationship, the disorder is not uncommon in older adults.95,96 It sometimes involves a mother and her children97 and forms part of a syndrome of childhood abuse.
Self-inflicted dermatoses are also observed in patients with anorexia nervosa.
Factitious disease involves many paradoxes, the most important of which is that the patient causes the physical symptoms and seeks a remedy for them. The psychodynamic etiology of factitious disorders may be related to a history of abuse or neglect in childhood, early emotional deprivation, or lack of care. All of these factors are found frequently in the history of these patients.47,98 Some authors have interpreted DA to be a disorder caused by borderline personality. In their opinion, the patient is both victim and punisher, a person intent on capturing the attention of doctors while at the same time challenging them and devaluing their usefulness. The additional benefit of playing the role of a sick person (thereby obtaining attention, support, and sympathy while escaping responsibilities) may also be important to these patients. By simulating a disease patients can evade responsibilities and satisfy their dependence needs, even though in DA this goal is achieved in a bizarre and self-destructive manner.
DA is not indicative of a particular personality organization, but the patient's personality type is a prognostic factor, as is the age of onset. In adolescents the disorder is usually a cry for help. The most common personality type in men with DA is paranoid while in women it is hysterical.13
It is currently thought that DA occurs in patients with a borderline personality disorder, although an association has also been described with impulse control disorder99 and obsessive compulsive disorder.100,101
PrognosisSeveral follow-up studies have been carried out to assess the prognosis in patients with DA. The first of these was undertaken by McCormack,67 who sent a questionnaire to 10 patients. Only 5 answered, and the findings of that study indicated that the condition is more uncommon in patients over 25 years of age. Subsequently, Sneddon et al,101 who studied 43 patients (38 women and 5 men), reported that DA was only one incident in a long history of mental illness. However, 30% of the patients in that study (12 women and one man) continued to self-inflict lesions or had other mental illnesses 12 years after the onset of DA. Years later, Haenel et al.98 invited 59 patients (52 women and 7 men) who had been diagnosed with DA to be reassessed. Of the 36 women and 2 men who responded, DA had resolved in 9, but the others still had recurrent lesions. Eight of the 36 women reported one or more suicide attempts. In a follow-up study carried out in our own department,26,102 61 patients who had been diagnosed with DA were invited to attend the clinic for reassessment. Nine (8 women and 1 man) of the 34 patients who responded (24 women and 10 men) were still affected by DA, an indication that this is a chronic and insidious disorder.
Malignant transformation of a lesion was reported in a woman with DA who persistently excoriated a cholecystectomy scar over 40 years.103 Another similar case involved the development of a malignant tumor in an ulcer on the face of a 49-year-old man, which the patient scratched compulsively.104 In both these cases, the malignancy was a Marjolin ulcer, a squamous cell carcinoma that arises in a chronic ulcer. The most common complications of DA are related to infections.
TreatmentDA probably represents one of the greatest therapeutic challenges in dermatology.12 Consoli13 suggested that the 3 pillars of treatment should be a) restructuring the patient's personality, b) drug treatment for the psychiatric condition, and c) medical treatment of the skin lesions. A prolonged period during which a friendly relationship can be established with the patient may help to prevent abrupt termination of treatment when the patient is finally confronted with the real situation. If this initial confrontation does not provoke a negative reaction or cause the patient to abandon treatment, a mental health treatment plan can be implemented, if possible including inpatient treatment. A supportive approach avoiding condemnation is always preferable. The dermatologist should be prepared for a prolonged course of treatment with repeated relapses and should never express disappointment or hostility over these failures. The cost of treating DA in 1 patient over 5 years of consultations has been estimated at €64 500.105
The treatment of factitious disease is often unsatisfactory, whether it is managed by a dermatologist, a psychiatrist, or both. Maybe the underlying reason is that these patients are in hiding and although they have to consult a physician because their symptoms are so obvious they do not wish to be cured.
The ideal approach is to refer the patient to a psychiatrist, but patients find such a referral incomprehensible because they believe they have a dermatological condition and do not understand why the dermatologist does not want to cure the lesions. As Sneddon27 has said, the treatment of patients with DA is difficult because, although they need the help of a psychiatrist, they reject this advice and any suggestion that their disease is not organic leads to a traumatic and conflictive visit after which they change doctors. When it is impossible to convince the patient to consult a psychiatrist, therapy with psychotropic drugs can be very helpful. The following drugs have been shown to be useful: selective serotonin reuptake inhibitors,58 pimozide (0.5-1mg/d), aripiprazole (2-5mg/d), or risperidone (0.5mg/d).106,107 Other measures and treatments that have been proposed include relaxation therapy, anxiolytics, antidepressants, and low doses of second-generation antipsychotics.108The skin lesions can be cured with the aid of occlusive dressings (adhesive zinc or sometimes plaster wrap).106 Rapid healing of a bandaged ulcer that has previously proved refractory to all treatment is a sign of great diagnostic value, as is the appearance of new lesions on unbandaged and, in most cases, previously unaffected areas. As occlusive bandages can be pierced by sharp instruments and patients can inject substances through the dressing, a sheet of aluminum foil may be included in the dressing to record the evidence of any such manipulations on the part of the patient.
Ethical DisclosuresProtection of human and animal subjectsThe authors state that no experiments were performed on humans or animals for this investigation.
Confidentiality of dataThe authors declare that they have followed the protocols of their workplace concerning the publication of patient data, and that all the patients included in this study have been appropriately informed and gave their written informed consent to participate in this study.
Right to privacy and informed consentThe authors declare that no private patient data are disclosed in this article
Conflicts of InterestsThe authors declare that they have no conflicts of interest.
Please cite this article as: Rodríguez Pichardo A, García Bravo B. Dermatitis artefacta: revisión. Actas Dermosifiliogr. 2013;104:854–866.