Mycosis fungoides (MF) is usually characterized by infiltrate containing T α/β helper memory cells with a classic immunophenotype (βF1+, CD3+, CD4+, CD5+, CD8−, CD45RO+). However, the broad clinical and histological spectrum and unusual phenotypic variants associated with MF make diagnosis difficult.
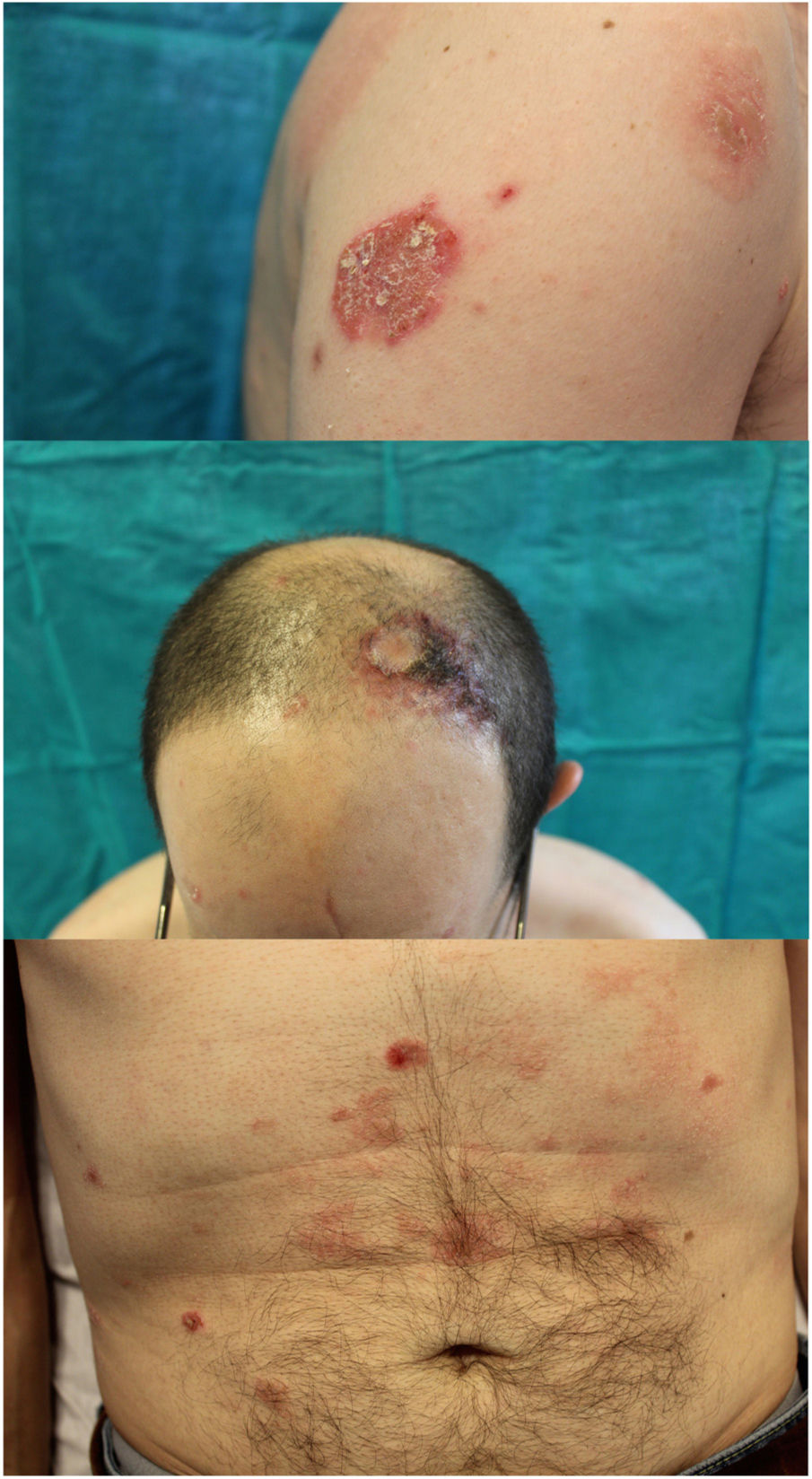
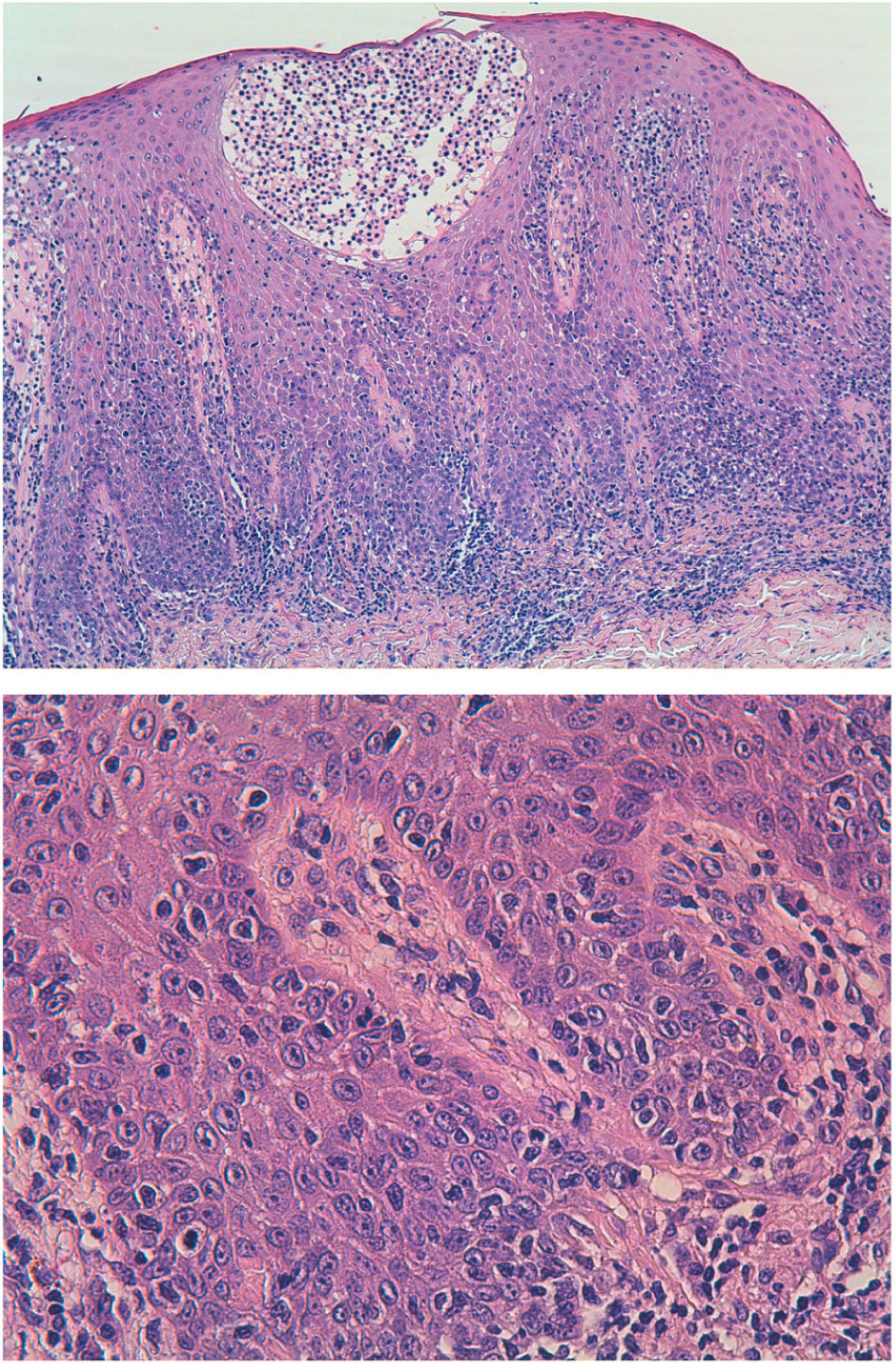
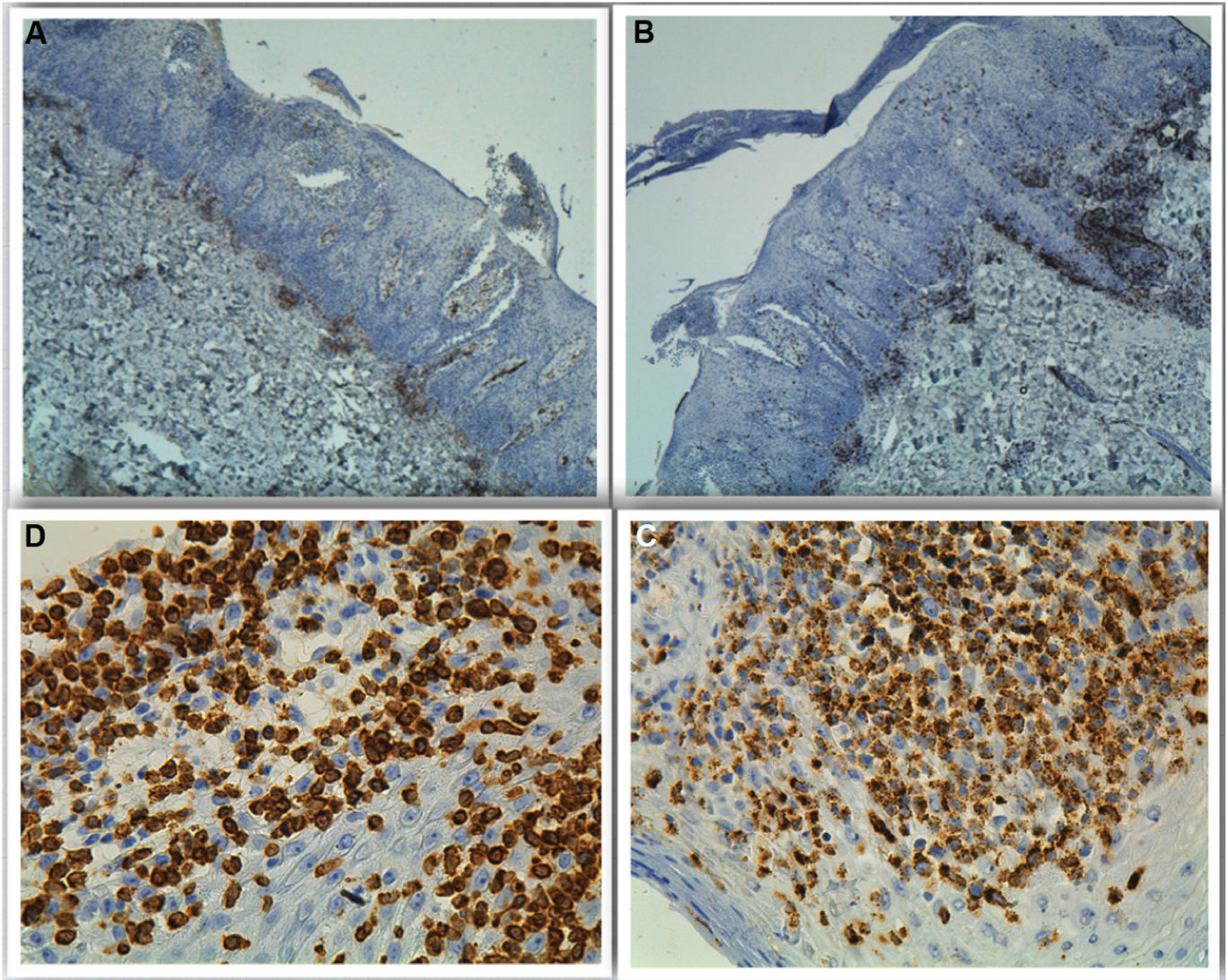
A 42-year-old man with no past history of interest was seen for asymptomatic lesions that had appeared 2 years earlier. These polymorphic and evanescent lesions consisted of psoriasiform and circular eczematous elements, some with circinate morphology (Fig. 1), and had been treated with multiple topical and oral treatments for the clinical diagnosis of dermatomycosis, eczema, and psoriasis. Fever, weight loss, profuse sweating, and other systemic clinical signs were absent. An initial biopsy revealed superficial lymphohistiocytic dermatitis with a psoriasiform pattern. A second biopsy showed atypical lymphocytic infiltrate (with angular, cerebriform, cleft nuclei) throughout the thickness of the epithelium, with a parabasal distribution, marked epidermotropism, and the presence of Pautrier microabscesses. These lymphocytes were also evident in the superficial dermis. The immunophenotype was positive for T-cell markers (cytoplasmic CD3 and CD2), with partial loss of CD5, and negative for CD4, CD8, CD7, and CD45RO. Analyses revealed negative T cell receptor (TCR) α and TCRβ gene rearrangement, and negative staining for CD30, PD1, and CD56. Cytotoxic markers (granzyme B, perforin, and TIA1) were detected (Figs. 2 and 3), and in situ hybridization for Epstein-Barr virus early transcripts (EBERs) was negative.
Histological image showing lymphocytic infiltrate throughout the thickness of the epithelium, with a parabasal distribution, marked epidermotropism, and the presence of Pautrier microabscesses. These lymphocytes are also observed in the superficial dermis. The lymphocytes are atypical, with angular, cerebriform, cleft nuclei.
Based on the finding of a cutaneous epidermotropic T cell lymphoma with a cytotoxic phenotype, the differential diagnosis included other cytotoxic lymphomas such as gamma/delta lymphoma, CD8+ lymphomatoid papulosis, and CD8+ epidermotropic cytotoxic T-cell lymphoma. The clinical–pathological correlation was essential to establish diagnosis of CD4-/CD8- cytotoxic MF. The results of a tumor extension analysis performed with positron emission tomography-computed tomography (PET-CT) were normal. Levels of lactate dehydrogenase and β2-microglobulin were normal, and peripheral blood flow cytometry revealed no findings of interest. The patient was treated with an ascending dose of methotrexate (up to 20 mg/wk), to which he showed a partial clinical response 12 weeks later. This was combined with narrowband ultraviolet B phototherapy 3 times per week, a regimen that the patient has continued.
Partial loss of T lymphocyte markers and positive cytotoxic markers have been described in cases of MF, although more frequently in late disease stages.1 Cases of CD4-/CD8- double-negative MF are rare. They are more common in early disease stages than in advanced forms,2,3 and tend to involve unusual clinical pictures (e.g. circinate or other polymorphic lesions) in addition to the classic lesions.4 However, the prognosis of this disease does not seem to be determined by the cellular phenotype.5 It is important to look out for these immunohistochemical variants of MF, and to bear in mind that a clinical–pathological correlation is essential to establish a correct diagnosis.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Ballano Ruiz A, Bakali Badesa S, Gómez Mateo MC, Yus Gotor MC. Micosis fungoide doble CD4-CD8 negativo de fenotipo citotóxico. Actas Dermosifiliogr. 2022;113:199–201.