We report the case of a 66-year-old man with a painful ulcer that he first noticed on the sole of his left foot 2 months previously. The lesion appeared during the month of August on atrophic and scarred skin that was compatible with chronic radiation-induced dermatitis over an area where 15 years earlier he had received radiation therapy for a skin lesion of unknown origin (no medical or histological data were available). The patient lived on the island of Mallorca and habitually walked along the seashore. He reported no history of diabetes, hypertension, smoking, or other systemic symptoms or conditions of interest.
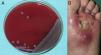
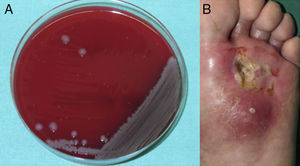
Examination of the skin revealed an ulcer with yellowish exudate, indurated margins, and atrophic skin in the adjacent areas. A blood workup revealed no leukocytosis or increased C-reactive protein levels. A substantial amount of tissue was taken from the margin and base of the ulcer for biopsy. Histopathology revealed collagenic fibrosis in the dermis and signs of vascular disease but no cellular atypia. These findings were compatible with radiation-induced dermatitis. Neoplastic processes were ruled out. Culture of the exudate revealed Vibrio alginolyticus (Fig. 1). Based on the results of the antibiogram, treatment was started with oral ciprofloxacin. However, the course was indolent, with the formation of a skin abscess (Fig. 1B) and development of osteomyelitis (Fig. 2) requiring admission to hospital. The lesion was debrided, even though no microorganisms grew in the culture. Antibiotic therapy was started with doxycycline and ceftriaxone for 10 days. Progress was good, and the ulcer resolved after 3 months.
V alginolyticus is a Gram-negative rod belonging to the genus Vibrio. It is the most halophilic of the Vibrio species, since it can grow in salt concentrations as high as 10%.1V alginolyticus is pathogenic for humans, although its virulence is low, and it is acquired after exposure to seawater or marine animals. V alginolyticus was the only microorganism isolated in the present case. However, it is often found in association with other Vibrio species such as Vibrio parahaemolyticus or Vibrio vulnificus.2V alginolyticus forms part of the habitual marine flora in temperate and tropical coastal waters. The incidence of infection by this microorganism in humans increases significantly during summer owing to the increase in the temperature of seawater.3 Similarly, the climate change observed in recent years leads us to believe that the density of this bacteria has been increasing both in tropical waters and in the colder waters of northern Europe.4
The microorganism is mainly associated with conjunctivitis, otitis, gastroenteritis, and superinfection of wounds that come into contact with contaminated seawater.5–7 Although its course is usually benign and it responds well to oral antibiotic therapy, cases of bacteremia and necrotizing fasciitis have also been reported.8 Patients usually present some degree of immunosuppression (eg, advanced age, diabetes mellitus, liver disease, or immunosuppressive therapy) that predisposes them to infection.8
Our literature search yielded only 1 other case of osteomyelitis caused by V alginolyticus. The patient had chronic hepatitis C and a surgical wound that became superinfected after exposure to seawater and progressed to involve bone tissue. As in the case we report, the patient's condition resolved with extensive surgical debridement and intravenous antibiotic therapy.9
Ulcers appearing on areas of radiation-induced dermatitis are particularly difficult to manage. Clinically, the skin is atrophic, sclerosed, and lacking adnexa, with altered pigment and telangiectases. Lesions on areas of chronic radiation-induced dermatitis appear at least 2 years after administration of ionizing radiation. The risk of secondary ulcers and cutaneous carcinoma is as high as 20%, since the skin is very deteriorated and chronically inflamed with a limited blood supply. Ulcers resulting from radiation-induced dermatitis usually have irregular margins and a base covered by very adherent yellowish slough. The indurated base of these lesions can lead us to suspect carcinoma. Hypoxia-induced tissue alterations and loss of skin integrity favor the risk of superinfection by various microorganisms.10
In the case we present, the dermatitis lesions remaining after treatment received several years previously are in themselves a predisposing factor and a source of local immunosuppression, thus potentially explaining the poor initial outcome of the ulcer.
In conclusion, this emerging microorganism should be taken into account in patients with infections of the skin and soft tissue who have been in contact with seawater or marine animals.
We are grateful to Drs Estrella Rojo and Jordi Reina for their help with this report.
Please cite this article as: Escudero MM, del Pozo LJ, Jubert E, Riera M. Úlcera cutánea sobre radiodermitis crónica por Vibrio alginolyticus. Actas Dermosifiliogr. 2015;106:774–775.