A 71-year-old ex-smoker, positive for hepatitis C virus (HCV), and with chronic renal insufficiency was being studied by the respiratory department due to a tumor in the left lung. He presented with a progressively growing bleeding, painful lesion that had appeared several months earlier on the pinna. The patient did not recall having suffered any trauma and had not undergone prior treatment.
Physical ExaminationThe physical examination revealed a crateriform nodule with a diameter of 1cm on the left pinna; the nodule appeared infiltrated on palpation. The lesion presented a central ulcerated area covered by a necrotic crust (Fig. 1). No satellite lesions or swollen cervical lymph nodes were observed.
Additional TestsLaboratory tests showed pancytopenia, abnormal liver function associated with HCV infection, and renal insufficiency, as reported previously. Tests for tumor markers in blood were negative. A biopsy of the lung nodule was negative for malignant cells.
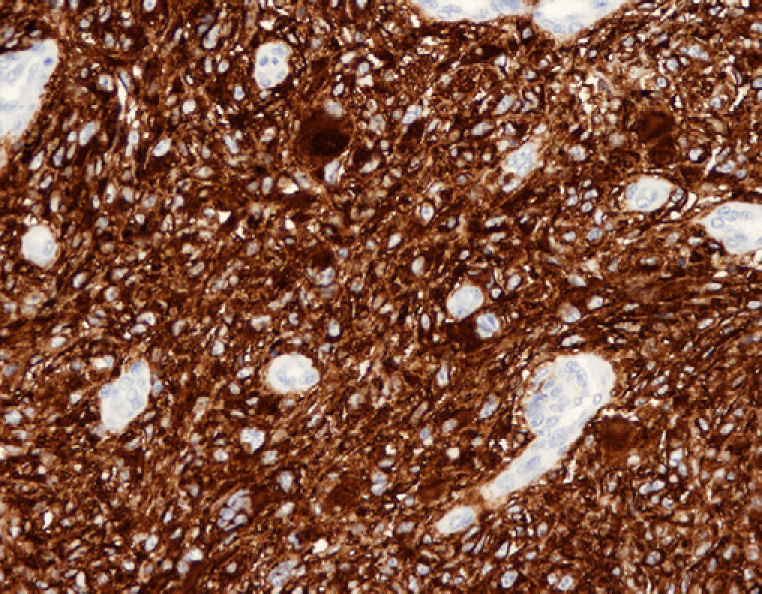
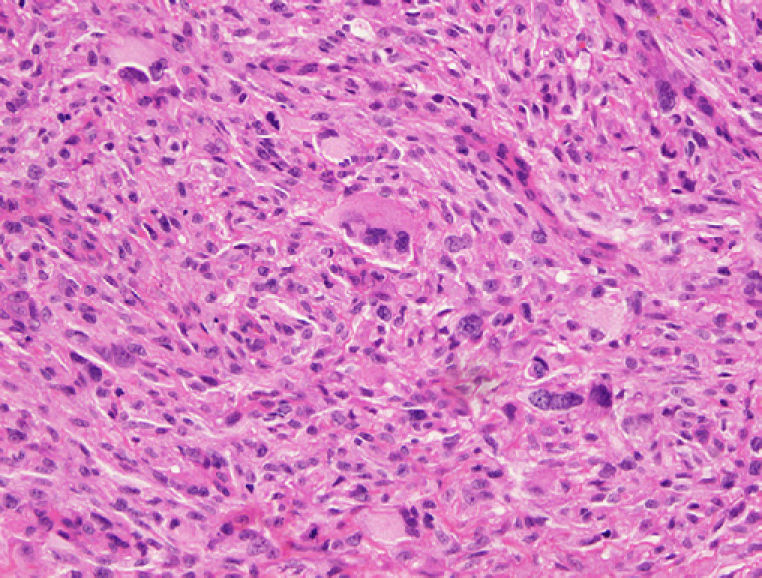
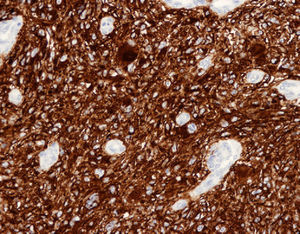
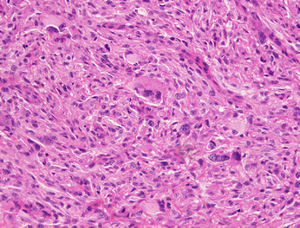
HistopathologyHistology revealed fusiform cells, together with multinucleated giant cells arranged in interlacing fascicles in the dermis. The nuclei showed varying degrees of atypia. Mitosis was abundant but no necrosis was observed (Fig. 2). Immunohistochemistry was positive for vimentin, smooth-muscle actin, and CD10 (Fig. 3), and negative for CD34 and S-100 protein.
What is your diagnosis?
DiagnosisAtypical fibroxanthoma.
Course and TreatmentThe lesion was fully excised with deep margins (to the cartilage). The patient died 4 months after surgery due to the progression of his renal insufficiency.
CommentAtypical fibroxanthoma was first described by Helwig in1961.1 It is a rare tumor that usually presents as a single nodule most frequently located on the head or neck.2 It affects men more than women and generally appears in elderly patients.3
The lesion presents clinically as a single painless nodule that usually measures up to 2cm3 and develops over a period of between 1 and 12 months.2
The lesion is located in the dermis. The tumor cells are of 3 types: fusiform cells (the majority) with varying degrees of nuclear atypia; histiocytoid cells, which give this tumor the name fibroxanthoma; and multinucleated giant cells. Necrosis, infiltration of deep layers of tissue, and vascular invasion, however, are more characteristic of malignant fibrous histiocytoma than of atypical fibroxanthoma.2 Immunohistochemistry shows these cells to be positive for vimentin alone, whereas melanoma is positive for vimentin and S100 proteins; spindle cell carcinoma is positive for cytokeratin; and leiomyosarcoma is positive for vimentin and desmin.4 Variable positivity has been reported in atypical fibroxanthoma for CD68, factor XIIIa, and CD99 and intense positivity for CD105.
In our case, the clinical differential diagnosis should include lung cancer metastasis, spindle cell carcinoma, basal cell carcinoma, keratoacanthoma, pyogenic granuloma, and desmoplastic malignant melanoma.2 The histologic differential diagnosis should include cutaneous leiomyosarcoma, malignant fibrous histiocytoma, spindle cell carcinoma, and malignant melanoma.2,5
Atypical fibroxanthoma is a cutaneous tumor that is considered to be a member of the family of fibrous histiocytic tumors. It has traditionally been thought to be a tumor of mesenchymal origin. It is thought to be a more superficial version of malignant fibrous histiocytoma because of its histologic similarity. It has been argued that atypical fibroxanthoma may be an undifferentiated variant of spindle cell carcinoma or melanoma, but immunohistochemistry findings rule out this argument and it is currently thought to be a tumor arising from fibroblasts or myofibroblasts.6 In terms of histology, it is a malignant tumor and may be locally aggressive, but with little tendency to metastasize (less than 1% of cases).3,6
Treatment of atypical fibroxanthoma is the subject of debate. Most studies recommend Mohs surgery4,6 over local excision with a wide margin,2 due to a lower observed rate of local recurrence. A follow-up of at least 2 years is recommended, as most recurrences are observed before this cut-off.6
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Maldonado P, et al. Nódulo crateriforme en el hélix. Actas Dermosifiliogr. 2011;102:629-30.