Glomuvenous malformations (GVM), previously known as glomangiomas, show a familial tendency and are characterized histologically by the presence of vascular channels surrounded by a variable number of glomus cells. There is a rare form that presents as plaques. The treatment of these lesions has still not been standardized.
Our patient was a newborn boy from a twin pregnancy, born preterm at 34 weeks, with erythematous plaques present on his back since birth. There was no family history of similar lesions. On physical examination, nonpulsatile, depressed erythematous-violaceous plaques were observed on the boy's back (Fig. 1A). We performed skin biopsy to clarify our differential diagnosis of capillary malformation, multiple myofibromas, or subcutaneous fat necrosis. Histopathology showed an increased number of ectatic vessels in the dermis and was interpreted as a capillary malformation.
Clinical course of the lesions. A, Newborn: erythematous-violaceous plaques on the back. B, At 6 months of age: plaques with prominent vessels, erythematous borders, and a blue-violaceous center. C, Before laser treatment (7 years of age). D, After 10 sessions of combined pulsed dye and neodymium-doped yttrium aluminium garnet laser treatment (11 years of age).
At 6 months, the plaques had acquired an annular pattern, with an erythematous halo, depressed blue-violaceous center, ectatic vessels, and flaccid skin (Fig. 1B).
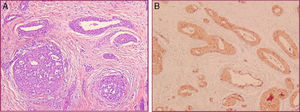
A further biopsy, performed because of the lack of clinical-pathological correlation, revealed a dermis with vascular structures surrounded by several layers of monomorphic round cells with eosinophilic cytoplasm (Fig. 2A). Immunohistochemistry showed the perivascular glomus cells to be positive for vimentin and α-actin and negative for desmin and S100 (Fig. 2B). Based on these findings, we made a diagnosis of congenital plaque-type GVM.
Initially we took a wait-and-see approach. Over the following years, the plaques extended to the adjacent skin and took on a more atrophic appearance, with very dilated vessels. No new lesions appeared.
At 7 years of age, the lesions were still asymptomatic, but their appearance (Fig. 1C) negatively affected the patient's self-esteem, leading us to evaluate the treatment options. The size of the lesions limited a possible surgical intervention. It was decided to start treatment with combined pulsed dye (PDL) (595nm) and neodymium-doped yttrium aluminium garnet (Nd:YAG) (1064nm) lasers (Cynergy Multiplex™, Cynosure, Westford, Massachusetts, United States), with a spot size of 10mm, a PDL pulse duration of 0.5ms and fluence of 8.5-9J/cm2, followed by a pulse of Nd:YAG with a duration of 15ms and fluence of 50J/cm2. A cooling system was used simultaneously to prevent epidermal damage. The sessions were performed under general anesthesia every 2 or 3 months. The post-treatment recommendations included oral analgesia and photoprotection. At the time of writing, the patient has received 10 sessions of laser therapy, with lightening of the color of the lesions and a reduction in lesion volume and in the caliber of the vessels (Fig. 1D). Treatment has been well tolerated and no complications have been detected.
GVMs account for 5% of venous malformations (VM) and are distinct from sporadic VMs and from hereditary mucocutaneous VMs. A familial tendency is detected in 88%, with an autosomal dominant inheritance pattern and incomplete penetrance (90%). Their etiology has been related to mutations in the glomulin gene (GLMN).1 GVMs are usually multiple and tend to appear at an early age. They can present as papular-nodular lesions or as plaques, and may be congenital2 or acquired.3
Congenital plaque-type GVMs present clinically as bluish plaques with a cobblestone surface,1 or as atrophic plaques with telangiectasias,2,4–9 as in our patient. A segmental distribution is often observed.5
Histology is characterized by a nonencapsulated proliferation of ectatic vascular channels surrounded by 1 or several layers of polygonal glomus cells. Immunohistochemistry is positive for α-smooth muscle actin and vimentin and negative for desmin.1–3
The clinical course of plaque-type GVMs varies. Progressive thickening and darkening of the lesions has been reported, as well as a tendency to spread into adjacent unaffected areas,2 as was seen in our patient.
The objectives of treatment of GVMs are to relieve pain and improve function and cosmetic appearance.6,7,9 Surgery is an option for small localized lesions. Treatments such as sclerotherapy and ablative therapy have been used in multiple or extensive GVMs, but results have not been consistent.10 There are also descriptions of cases treated with Nd:YAG laser with good results,9 and PDL lasers have been reported to be useful for the more superficial component of the lesions.6 The dual laser (PDL/Nd:YAG) allows us to treat different depths of the skin using lower fluences and thus minimize the risk of scars or necrosis. There are 2 previous reports of congenital plaque-type GVM treated successfully with the combined PDL/Nd:YAG laser,10 using higher Nd:YAG fluences than those employed in our patient, with no complications (Table 1).
Patients With Congenital Plaque-Type Glomuvenous Malformations Treated With Combined Pulsed Dye and Neodymium-Doped Yttrium Aluminium Garnet Laser.
| Reference | Age and Sex | Site Affected | Fluence | Pulse Duration | Spot Size | No. of Sessions | Follow-up Period | Response | Complications |
|---|---|---|---|---|---|---|---|---|---|
| 6 | 34 y Male | Left arm | PDL 8J/cm2 Ns:YAG 70J/cm2 | PDL: 0.5ms Ns:YAG: 15ms | 10mm | 4 | 1 y | Resolution of the pain, lightening of color and volume reduction | None |
| 7 | 6 mo Female | Scalp, trunk, abdomen, back, right inguinal region and thighs | PDL: 6J/cm2 Ns:YAG: 110J/cm2 | PDL: 0.5ms Ns:YAG: 20ms | 10mm | 6 | 18 mo | Lightening of color and size reduction | None |
| Our patient | 11 y Male | Back | PDL: 8.5J/cm9 Ns:YAG: 50J/cm9 | PDL: 0.5ms Ns:YAG: 15ms | 10mm | 10 | 11 y | Lightening of color and reduction of volume and of vessel caliber | None |
In conclusion, we have presented a case of congenital plaque-type GVM that, in its initial phases, was included in the series by Mallory et al.2 We draw attention to its uncommon clinical presentation, which was a diagnostic challenge and required histopathological confirmation, the atypical clinical course over 11 years, and the favorable response to combined laser treatment.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
Please cite this article as: Vargas-Navia N, Baselga E, Muñoz-Garza FZ, Puig L. Malformación glomovenosa congénita en placas: 11 años de seguimiento y respuesta al tratamiento con láser combinado PDL/Nd: YAG. Actas Dermosifiliogr. 2017;108:72–74.